Pyonephrosis overview
|
Pyonephrosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pyonephrosis overview On the Web |
|
American Roentgen Ray Society Images of Pyonephrosis overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Harsh Vardhan Chawla, M.B.B.S.[2]
Overview
Pyonephrosis (Greek pyon "pus" + nephros "kidney") is an infection of obstructed renal collecting system leading to accumulation of pus in the renal collecting system. Pus collects in the renal pelvis and eventually causes destruction of the renal parenchyma. Pyonephrosis is sometimes a complication of renal stones, which can be a source of persisting infection. It may also occur spontaneously.
It needs an early diagnosis and immediate intervention as it may progress to Urosepsis. Treatment may require drainage, best performed by nephrostomy.
Pathophysiology
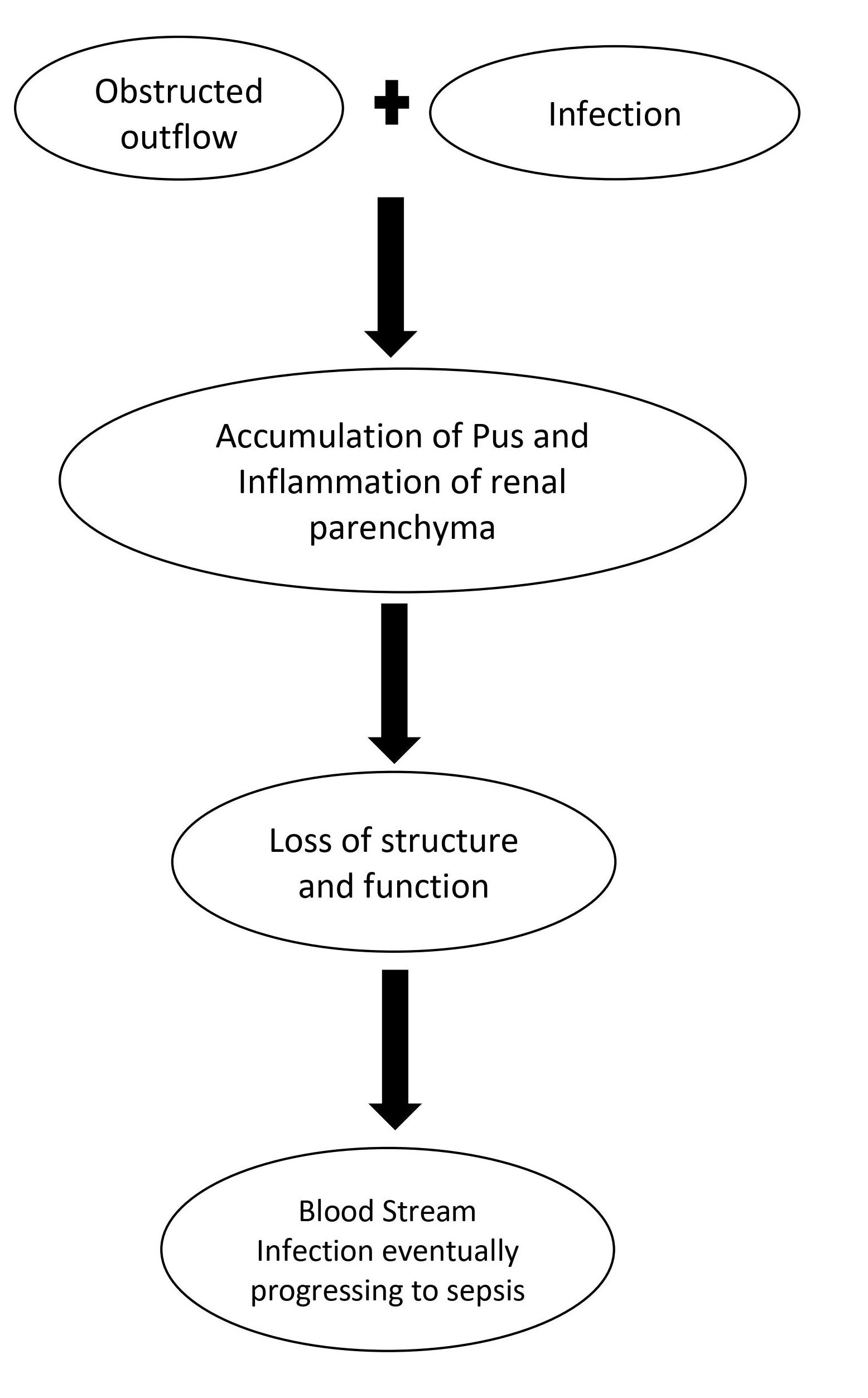
Pyonephrosis can be seen as a complication of acute pyelonephritis, usually seen with complete or incomplete obstruction of tubules. Obstruction of ureter and renal pelvis causes dilatation of tubular system which in turn leads to hydronephrosis. The dilatation of the tubular system serves as a nidus for infection because the pathogens multiply easily in obstructed and dilated tubules leading to suppurative inflammation.
Causes
Pyonephrosis is commonly caused by bacteria such as Enterococcus spp., K. pneumoniae, Candida spp., S. aureus, P. mirabilis, P. aeruginosa and Group B Streptococcus. The accumulation of pus combined with inability to drain due to obstruction results in pyonephrosis.
Risk Factors
Risk factors for pyonephrosis include immunosuppression, local factors of the genitourinary tract like nephrolithiasis, pregnancy, tumors, congenital urological anomalies etc.
Epidemiology and Demographics
Although an uncommon condition overall, pyonephrosis has been reported in neonates, children, as well as adults, indicating it can develop in any age group.
Natural History, Complications, and Prognosis
Pyonephrosis is a urological emergency. If left untreated, it can rapidly lead to septic shock and death. Upon early treatment, the prognosis of pyonephrosis is good. There is a significant improvement in the condition within 24-48 hours after drainage of the pus. Structural changes like scarring, fistulas, and abscess formations may occur if the treatment of the cause of obstruction is delayed.
Diagnosis
History and Symptoms
Patients with pyonephrosis can present with a history of Sudden onset of symptoms including fever and chills, recent urinary tract infection, previous history of pyelonephritis or nephrolithiasis. The patients can be asymptomatic or present with symptoms like fever with chills, flank pain, back pain, abdominal pain, nausea and vomiting among others.
Physical Examination
A patient with pyonephrosis usually appears uncomfortable and ill. Vital signs may be unstable if the patient is going into septic shock. On abdominal examination, costovertebral angle tenderness may be present. Digital rectal examination may reveal an enlarged prostate gland in an elderly male patient. The cardiovascular and pulmonary examination is usually within normal limits except for the presence of tachycardia.
Laboratory Findings
The initial workup done when suspecting a case of pyonephrosis include urinalysis and culture which may show white blood cells, bacteria, and pus cells; complete blood count with differentials showing neutrophilia, and blood culture which may be positive if bacteremia has already occurred. The urine and blood samples for culture must be obtained prior to starting the antibiotic therapy.
CT scan
CT scan provides anatomic details and helps in distinguishing intrarenal and extrarenal pathologies but it is difficult to distinguish hydronephrosis from pyonephrosis on a CT scan. The indirect signs of pyonephrosis on CT scan include enlarged kidneys, presence of an infected collecting system in the setting of hydronephrosis, perinephric fat stranding, pelvic wall thickening, fluid-fluid levels, and gas within the collecting system.
MRI
Magnetic resonance imaging (MRI) is used in genitourinary tract conditions if CT scan is non-diagnostic or when CT scan is contraindicated. Diffusion-weighted MRI (DW-MRI) can differentiate pyonephrosis from hydronephrosis.
Other Imaging Findings
Other investigations that might be used to diagnose pyonephrosis are renal nuclear scanning and antegrade nephrostography. Renal nuclear scanning aids in determining the functionality of the involved kidney after the infection has resolved whereas antegrade nephrostography is used to determine the cause of the obstruction contributing to pyonephrosis for definitive treatment.
Treatment
Medical Treatment
Pyonephrosis is a surgical emergency. Hemodynamically unstable patients may require aggressive fluid resuscitation with crystalloids and pressor agent (dopamine) to maintain adequate blood pressure. All patients with pyonephrosis should be empirically treated with intravenous long-acting, broad-spectrum antibiotics like ampicillin + gentamicin combined with urgent drainage of the pus. After treating the infection, additional investigations are required to find the cause of the obstruction e.g., nephrolithiasis, tumors, etc. for definitive treatment.
Surgery
Earlier, nephrectomy was the standard treatment for pyonephrosis. However, now interventional procedures like retrograde ureteral stenting or percutaneous nephrostomy catheter placement are done for urgent decompression depending on the hemodynamic stability of the patient and some other factors like the presence of urolithiasis.
Primary Prevention
There is no established method for the prevention of pyonephrosis.
Secondary Prevention
Immediate intravenous antibiotic treatment followed by prompt decompression of the pus is essential to prevent the development of septic shock and rapid worsening of the patient's condition. Structural changes like scarring, fistulas, and abscesses may occur if the definitive treatment is delayed after resolution of the infection.