Prurigo nodularis
| Prurigo nodularis | |
| ICD-10 | L28.1 |
|---|---|
| ICD-9 | 698.3 |
| DiseasesDB | 32152 |
| eMedicine | derm/350 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Kiran Singh, M.D. [2]
Overview
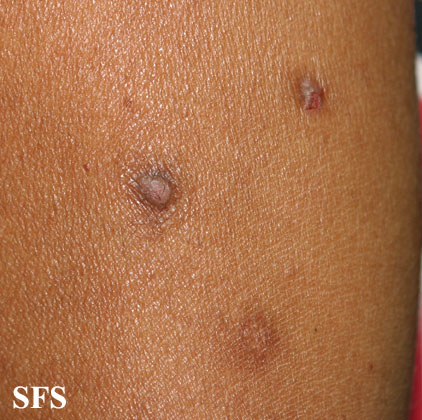
Prurigo nodularis (PN) is a skin disease characterised by pruritic (itchy) nodules which usually appear on the arms or legs. Patients often present with multiple excoriated lesions caused by scratching.
History
It was first described by Hyde and Montgomery in 1909.[1]
Causes
The cause is unknown, although other conditions may induce PN. These include HIV[2] and other immunodeficiency diseases. Internal malignancies, liver failure, renal failure, and psychiatric illnesses may induce PN, although more recent research has refuted a psychiatric cause for PN. Lockshin et al recently linked PN to Becker's nevus;[3] Torchia et al recently found PN to be linked to linear IgA disease, an autoimmune condition;[4] and Sonkoly et al report a link between T cells and PN.[5] Patients report an ongoing battle to distinguish themselves from those with psychiatric disorders such as delusions of parasitosis and other psychiatric conditions.[6]
Pathophysiology
Chronic and repetitive scratching, picking, or rubbing of the nodules may result in permanent changes to the skin, including nodular lichenification, hyperkeratosis, hyperpigmentation, and skin thickening. Unhealed, excoriated lesions are often scaly, crusted or scabbed. Many patients report a lack of wound healing even when medications relieve the itching and subsequent scratching.[7]
Patients often:
- seek treatment during middle-age, although PN can occur at any age.
- have a history of chronic severe pruritus.
- have a significant medical history for unrelated conditions.
- suffer from liver or kidney dysfunctions.
- suffer secondary skin infections.
- have a personal or family history of atopic dermatitis.
- have other autoimmune disorders.
Lesions and Nodules
- Nodules are discrete, generally symmetric, hyperpigmented or purpuric, and firm. They are greater than 0.5cm in both width and depth (as opposed to papules which are less than 0.5cm). They can appear on any part of the body, but generally begin on the arms and legs.
- Excoriated lesions are often flat, umbilicated, or have a crusted top.
- Nodules may appear to begin in the hair follicles.
- Nodule pattern may be follicular.
- In true prurigo nodularis, a nodule forms before any itching begins. Typically, these nodules are extremely pruritic and are alleviated only by steroids.
Diagnosis
Diagnosis is based on visual examination and the presence of itching. A skin biopsy is often performed to exclude other diseases. Lesion biopsies will typically show a high level of eosinophils in PN.[8]
Physical Examination
Skin
Extremities
-
Prurigo nodularis. With permission from Dermatology Atlas.[9]
-
Prurigo nodularis. With permission from Dermatology Atlas.[9]
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.[9]
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.[9]
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.[9]
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.[9]
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.[9]
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.[9]
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.[9]
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.[9]
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.[9]
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.
-
Prurigo nodularis. With permission from Dermatology Atlas.[9]
Treatment
Prurigo nodularis is very hard to treat, but current therapies include steroids, vitamins, cryosurgery, thalidomide and UVB light. A physician may administer a strong dose of prednisone, which will almost immediately stop the itch/scratch cycle. However, cessation of steroids allows relapse to occur, usually within a few weeks. Horiuchi et al recently reported significant improvement in PN with antibiotic therapy.[10]
Synonyms
Hyde prurigo nodularis, Picker nodules, lichen simplex chronicus, atypical nodular form of neurodermatitis circumscripta, lichen corneus obtusus. PN patients of the 21st century consider "Picker's disease" to be an offensive and medieval reference.
Notes
- ↑ Hyde JN, Montgomery FH: A practical treatise on disease of the skin for the use of students and practitioners. 1909; 174–175.
- ↑ Berger TG, Hoffman C, Thieberg MD (1995). "Prurigo nodularis and photosensitivity in AIDS: treatment with thalidomide". J. Am. Acad. Dermatol. 33 (5 Pt 1): 837–8. PMID 7593791.
- ↑ Lockshin BN, Brogan B, Billings S, Billings S (2006). "Eczematous dermatitis and prurigo nodularis confined to a Becker's nevus". Int. J. Dermatol. 45 (12): 1465–6. doi:10.1111/j.1365-4632.2006.02971.x. PMID 17184268.
- ↑ Torchia D, Caproni M, Del Bianco E, Cozzani E, Ketabchi S, Fabbri P (2006). "Linear IgA disease presenting as prurigo nodularis". Br. J. Dermatol. 155 (2): 479–80. doi:10.1111/j.1365-2133.2006.07315.x. PMID 16882196.
- ↑ Sonkoly E, Muller A, Lauerma AI; et al. (2006). "IL-31: a new link between T cells and pruritus in atopic skin inflammation". J. Allergy Clin. Immunol. 117 (2): 411–7. doi:10.1016/j.jaci.2005.10.033. PMID 16461142.
- ↑ Prurigo Nodularis Support: http://p205.ezboard.com/fprurigonodularissupportfrm1
- ↑ Prurigo Nodularis Support: http://p205.ezboard.com/fprurigonodularissupportfrm1
- ↑ Johansson O, Liang Y, Marcusson JA, Reimert CM (2000). "Eosinophil cationic protein- and eosinophil-derived neurotoxin/eosinophil protein X-immunoreactive eosinophils in prurigo nodularis". Arch. Dermatol. Res. 292 (8): 371–8. PMID 10994770.
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 "Dermatology Atlas".
- ↑ Horiuchi Y, Bae S, Katayama I (2006). "Uncontrollable prurigo nodularis effectively treated by roxithromycin and tranilast". Journal of drugs in dermatology : JDD. 5 (4): 363–5. PMID 16673805.
References
- Feuerman EJ, Sandbank M (1975). "Prurigo nodularis. Histological and electron microscopical study". Archives of dermatology. 111 (11): 1472–7. PMID 1200655.
- Hann SK, Cho MY, Park YK (1990). "UV treatment of generalized prurigo nodularis". Int. J. Dermatol. 29 (6): 436–7. PMID 2397971.*Hyde JN, Montgomery FH. A practical treatise on disease of the skin for the use of students and practitioners. 1909; 174–175.
- Jacob CI, Patten SF (1999). "Strongyloides stercoralis infection presenting as generalized prurigo nodularis and lichen simplex chronicus". J. Am. Acad. Dermatol. 41 (2 Pt 2): 357–61. PMID 10426933.
- Lee MR, Shumack S (2005). "Prurigo nodularis: a review". Australas. J. Dermatol. 46 (4): 211–18, quiz 219-20. doi:10.1111/j.1440-0960.2005.00187.x. PMID 16197418.
- Matthews SN, Cockerell CJ (1998). "Prurigo nodularis in HIV-infected individuals". Int. J. Dermatol. 37 (6): 401–9. PMID 9646121.
- Miyauchi H, Uehara M (1988). "Follicular occurrence of prurigo nodularis". J. Cutan. Pathol. 15 (4): 208–11. PMID 3183136.
- Noppakun N, Apisarnthanarax P (1981). "Multiple cutaneous granular cell tumors simulating prurigo nodularis". Int. J. Dermatol. 20 (2): 126–9. PMID 7216595.
- Roenigk RK, Dahl MV (1986). "Bullous pemphigoid and prurigo nodularis". J. Am. Acad. Dermatol. 14 (5 Pt 2): 944–7. PMID 3519701.
- Sandbank M (1976). "Cutaneous nerve lesions in prurigo nodularis. Electron microscopic study of two patients". J. Cutan. Pathol. 3 (3): 125–32. PMID 1002871.
- Seeburger J, Anderson-Wilms N, Jacobs R (1993). "Lennert's lymphoma presenting as prurigo nodularis". Cutis; cutaneous medicine for the practitioner. 51 (5): 355–8. PMID 8513688.
- Stoll DM, Fields JP, King LE (1983). "Treatment of prurigo nodularis: use of cryosurgery and intralesional steroids plus lidocaine". The Journal of dermatologic surgery and oncology. 9 (11): 922–4. PMID 6630706.
- Szeidemann Z, Shanabrough M, Leranth C (1995). "Hypothalamic Leu-enkephalin-immunoreactive fibers terminate on calbindin-containing somatospiny cells in the lateral septal area of the rat". J. Comp. Neurol. 358 (4): 573–83. doi:10.1002/cne.903580410. PMID 7593751.
- Tupker RA, Coenraads PJ, van der Meer JB (1992). "Treatment of prurigo nodularis, chronic prurigo and neurodermatitis circumscripta with topical capsaicin". Acta Derm. Venereol. 72 (6): 463. PMID 1362846.
- Vaalasti A, Suomalainen H, Rechardt L (1989). "Calcitonin gene-related peptide immunoreactivity in prurigo nodularis: a comparative study with neurodermatitis circumscripta". Br. J. Dermatol. 120 (5): 619–23. PMID 2474315.
- Waldinger TP, Wong RC, Taylor WB, Voorhees JJ (1984). "Cryotherapy improves prurigo nodularis". Archives of dermatology. 120 (12): 1598–600. PMID 6508332.
![Prurigo nodularis. With permission from Dermatology Atlas.[9]](/images/e/eb/Prurigo_nodularis01.jpg)
![Prurigo nodularis. With permission from Dermatology Atlas.[9]](/images/0/00/Prurigo_nodularis02.jpg)



![Prurigo nodularis. With permission from Dermatology Atlas.[9]](/images/0/0b/Prurigo_nodularis06.jpg)

![Prurigo nodularis. With permission from Dermatology Atlas.[9]](/images/5/5b/Prurigo_nodularis08.jpg)










![Prurigo nodularis. With permission from Dermatology Atlas.[9]](/images/0/0b/Prurigo_nodularis20.jpg)










![Prurigo nodularis. With permission from Dermatology Atlas.[9]](/images/3/32/Prurigo_nodularis32.jpg)



![Prurigo nodularis. With permission from Dermatology Atlas.[9]](/images/0/03/Prurigo_nodularis36.jpg)


![Prurigo nodularis. With permission from Dermatology Atlas.[9]](/images/3/38/Prurigo_nodularis40.jpg)




![Prurigo nodularis. With permission from Dermatology Atlas.[9]](/images/7/74/Prurigo_nodularis46.jpg)




![Prurigo nodularis. With permission from Dermatology Atlas.[9]](/images/9/96/Prurigo_nodularis52.jpg)



![Prurigo nodularis. With permission from Dermatology Atlas.[9]](/images/7/71/Prurigo_nodularis56.jpg)


![Prurigo nodularis. With permission from Dermatology Atlas.[9]](/images/9/90/Prurigo_nodularis59.jpg)