Prochlorperazine (injection)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aparna Vuppala, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
Warning
See full prescribing information for complete Boxed Warning.
Increased Mortality in Elderly Patients with Dementia-Related Psychosis :
|
Overview
Prochlorperazine (injection) is a antiemetic that is FDA approved for the treatment of severe nausea and vomiting, schizophrenia. There is a Black Box Warning for this drug as shown here. Common adverse reactions include drowsiness, dizziness, amenorrhea, blurred vision, skin reactions and hypotension.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- To control severe nausea and vomiting. For the treatment of schizophrenia.
- Prochlorperazine has not been shown effective in the management of behavioral complications in patients with mental retardation.
Dosage
- Notes on Injection
- For intramuscular administration, inject deeply into the upper, outer quadrant of the buttock.Subcutaneous administration is not advisable because of local irritation.
- Stability
- This solution should be protected from light. A slight yellowish discoloration will not alter potency. If markedly discolored, solution should be discarded.
- Compatibility
- It is recommended that prochlorperazine injection not be mixed with other agents in the syringe.
ADULTS
- (For children's dosage and administration, see below.) Dosage should be increased more gradually in debilitated or emaciated patients.
Elderly Patients
- In general, dosages in the lower range are sufficient for most elderly patients. Since they appear to be more susceptible to hypotension and neuromuscular reactions, such patients should be observed closely. Dosage should be tailored to the individual, response carefully monitored and dosage adjusted accordingly. Dosage should be increased more gradually in elderly patients.
- To Control Severe Nausea and Vomiting: Adjust dosage to the response of the individual. Begin with the lowest recommended dosage.
- I.M. Dosage: Initially 5 to 10 mg (1 to 2 mL) injected deeply into the upper outer quadrant of the buttock. If necessary, repeat every 3 or 4 hours. Total I.M. dosage should not exceed 40 mg per day.
- I.V. Dosage: 2.5 to 10 mg (0.5 to 2 mL) by slow I.V. injection or infusion at a rate not to exceed 5 mg per minute. Prochlorperazine edisylate injection may be administered either undiluted or diluted in isotonic solution. A single dose ofthe drug should not exceed 10 mg; total I.V. dosage should not exceed 40 mg per day. When administered I.V., do not use bolus injection. Hypotension is a possibility if the drug is given by I.V. injection or infusion.
- Subcutaneous administration is not advisable because of local irritation.
- Adult Surgery (for severe nausea and vomiting): Total parenteral dosage should not exceed 40 mg per day. Hypotension is a possibility if the drug is given by I.V. injection or infusion.
- I.M. Dosage: 5 to 10 mg (1 to 2 mL) 1 to 2 hours before induction of anesthesia (repeat once in 30 minutes, if necessary), or to control acute symptoms during and after surgery (repeat once if necessary).
- I.V. Dosage: 5 to 10 mg (1 to 2 mL) as a slow I.V. injection or infusion 15 to 30 minutes before induction of anesthesia, or to control acute symptoms during or after surgery. Repeat once if necessary. Prochlorperazine may be administered either undiluted or diluted in isotonic solution, but a single dose of the drug should not exceed 10 mg. The rate of administration should not exceed 5 mg per minute. When administered I.V., do not use bolus injection.
- In Adult Psychiatric Disorders: Adjust dosage to the response of the individual and according to the severity of the condition. Begin with the lowest recommended dose. Although response ordinarily is seen within a day or 2, longer treatment is usually required before maximal improvement is seen.
- I.M. Dosage: For immediate control of adult schizophrenic patients with severe symptomatology, inject an initial dose of 10 to 20 mg (2 to 4 mL) deeply into the upper outer quadrant of the buttock. Many patients respond shortly after the first injection. If necessary, however, repeat the initial dose every 2 to 4 hours (or, in resistant cases, every hour) to gain control of the patient. More than three or four doses are seldom necessary. After control is achieved, switch patient to an oral form of the drug at the same dosage level or higher. If, in rare cases, parenteral therapy is needed for a prolonged period, give 10 to 20 mg (2 to 4 mL) every 4 to 6 hours. Pain and irritation at the site of injection have seldom occurred.
- Subcutaneous administration is not advisable because of local irritation.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Prochlorperazine (injection) in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Prochlorperazine (injection) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
- DO NOT USE IN PEDIATRIC SURGERY.
- Children seem more prone to develop extrapyramidal reactions, even on moderate doses. Therefore, use lowest effective dosage. Tell parents not to exceed prescribed dosage, since the possibility of adverse reactions increases as dosage rises. Occasionally the patient may react to the drug with signs of restlessness and excitement; if this occurs, do not administer
additional doses. Take particular precaution in administering the drug to children with acute illnesses or dehydration .
- Severe Nausea and Vomiting in Children: Prochlorperazine should not be used in pediatric patients under 20 pounds in weight or 2 years of age. It should not be used in conditions for which children's dosages have not been established. Dosage and frequency of administration should be adjusted according to the severity of the symptoms and the response of the patient. The duration of activity following intramuscular administration may last up to 12 hours. Subsequent doses may be given by the same route if necessary.
- I.M. Dosage: Calculate each dose on the basis of 0.06 mg of the drug per lb of body weight; give by deep I.M. injection. Control is usually obtained with one dose.
Children with Schizophrenia:
- I.M. Dosage: For ages under 12, calculate each dose on the basis of 0.06 mg of prochlorperazine per lb of body weight; give by deep I.M. injection. Control is usually obtained with one dose. After control is achieved, switch the patient to an oral form of the drug at the same dosage level or higher.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Prochlorperazine (injection) in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Prochlorperazine (injection) in pediatric patients.
Contraindications
- Do not use in patients with known hypersensitivity to phenothiazines.
- Do not use in comatose states or in the presence of large amounts of central nervous system depressants (alcohol, barbiturates, narcotics, etc.).
- Do not use in pediatric surgery.
- Do not use in pediatric patients under 2 years of age or under 20 lbs. Do not use in children for conditions for which dosage has not been established.
Warnings
|
Warning
See full prescribing information for complete Boxed Warning.
Increased Mortality in Elderly Patients with Dementia-Related Psychosis :
|
Precautions
Leukopenia, Neutropenia and Agranulocytosis:
- In clinical trial and postmarketing experience, events of leukopenia/neutropenia and agranulocytosis have been reported temporally related to antipsychotic agents. Possible risk factors for leukopenia/neutropenia include preexisting low white blood cell count (WBC) and history of drug induced leukopenia/neutropenia. Patients with a preexisting low WBC or a history of drug induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and should discontinue Prochlorperazine Edisylate Injection USP at the first sign of a decline in WBC in the absence of other causative factors. Patients with neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count less than 1000/mm3) should discontinue Prochlorperazine Edisylate Injection USP and have their WBC followed until recovery. Prochlorperazine's antiemetic action may mask signs and symptoms of overdosage of other drugs and may obscure the diagnosis and treatment of other conditions such as intestinal obstruction, brain tumor and Reye's syndrome .When prochlorperazine is used with cancer chemotherapeutic drugs, vomiting as a sign of the toxicity of these agents may be obscured by the antiemetic effect of prochlorperazine. Because hypotension may occur, large doses and parenteral administration should be used cautiously in patients with impaired cardiovascular systems. To minimize the occurrence of hypotension after injection, keep patient lying down and observe for at least 1/2 hour. If hypotension occurs after parenteral dosing, place patient in head-low position with legs raised. If a vasoconstrictor is required, norepinephrine and phenylephrine are suitable. Other pressor agents, including epinephrine, should not be used because they may cause a paradoxical further lowering of blood pressure. Aspiration of vomitus has occurred in a few post-surgical patients who have received prochlorperazine as an antiemetic. Although no causal relationship has been established, this possibility should be borne in mind during surgical aftercare. Deep sleep, from which patients can be aroused, and coma have been reported, usually with overdosage. Antipsychotic drugs elevate prolactin levels; the elevation persists during chronic administration. Tissue culture experiments indicate that approximately one third of human breast cancers are prolactin-dependent in vitro, a factor of potential importance if the prescribing of these drugs is contemplated in a patient with a previously detected breast cancer. Although disturbances such as galactorrhea, amenorrhea, gynecomastia and impotence have been reported, the clinical significance of elevated serum prolactin levels is unknown for most patients. An increase in mammary neoplasms has been found in rodents after chronic administration of antipsychotic drugs. Neither clinical nor epidemiologic studies conducted to date, however, have shown an association between chronic administration of these drugs and mammary tumorigenesis; the available evidence is considered too limited to be conclusive at this time. Chromosomal aberrations in spermatocytes and abnormal sperm have been demonstrated in rodents treated with certain antipsychotics. As with all drugs which exert an anticholinergic effect, and/or cause mydriasis, prochlorperazine should be used with caution in patients with glaucoma. Because phenothiazines may interfere with thermoregulatory mechanisms, use with caution in persons who will be exposed to extreme heat.
- Phenothiazines can diminish the effect of oral anticoagulants. Phenothiazines can produce alpha-adrenergic blockade. Thiazide diuretics may accentuate the orthostatic hypotension that may occur with phenothiazines. Antihypertensive effects of guanethidine and related compounds may be counteracted when phenothiazines are used concomitantly. Concomitant administration of propranolol with phenothiazines results in increased plasma levels of both drugs. Phenothiazines may lower the convulsive threshold; dosage adjustments of anticonvulsants may be necessary. Potentiation of anticonvulsant effects does not occur. However, it has been reported that phenothiazines may interfere with the metabolism of phenytoin and thus precipitate phenytoin toxicity. The presence of phenothiazines may produce false-positive phenylketonuria (PKU) test results.
Long-Term Therapy
- Given the likelihood that some patients exposed chronically to antipsychotics will develop tardive dyskinesia, it is advised that all patients in whom chronic use is contemplated be given, if possible, full information about this risk. The decision to inform patients and/or their guardians must obviously take into account the clinical circumstances and the competency of the patient to understand the information provided. To lessen the likelihood of adverse reactions related to cumulative drug effect, patients with a history of long-term therapy with prochlorperazine and/or other antipsychotics should be evaluated periodically to decide whether the maintenance dosage could be lowered or drug therapy discontinued. Children with acute illnesses (e.g., chickenpox, CNS infections, measles, gastroenteritis) or dehydration seem to be much more susceptible to neuromuscular reactions, particularly dystonias, than are adults. In such patients, the drug should be used only under close supervision. Drugs which lower the seizure threshold, including phenothiazine derivatives, should not be used with metrizamide. As with other phenothiazine derivatives, prochlorperazine should be discontinued at least 48 hours before myelography, should not be resumed for at least 24 hours postprocedure, and should not be used for the control of nausea and vomiting occurring either prior to myelography with metrizamide, or postprocedure.
Adverse Reactions
Clinical Trials Experience
- Drowsiness, dizziness, amenorrhea, blurred vision, skin reactions and hypotension may occur. Neuroleptic Malignant Syndrome (NMS) has been reported in association with antipsychotic drugs (see WARNINGS). Cholestatic jaundice has occurred. If fever with grippe-like symptoms occurs, appropriate liver studies should be conducted. If tests indicate an abnormality, stop treatment. There have been a few observations of fatty changes in the livers of patients who have died while receiving the drug. No causal relationship has been established. Leukopenia and agranulocytosis have occurred. Warn patients to report the sudden appearance of sore throat or other signs of infection. If white blood cell and differential counts indicate leukocyte depression, stop treatment and start antibiotic and other suitable therapy.
Neuromuscular (Extrapyramidal) Reactions
- These symptoms are seen in a significant number of hospitalized mental patients. They may be characterized by motor restlessness, be of the dystonic type, or they may resemble parkinsonism. Depending on the severity of symptoms, dosage should be reduced or discontinued. If therapy is reinstituted, it should be at a lower dosage. Should these symptoms occur in children or pregnant patients, the drug should be stopped and not reinstituted. In most cases barbiturates by suitable route of administration will suffice, or injectable diphenhydramine may be useful. In more severe cases, the administration of an anti-parkinsonism agent, except levodopa, usually produces rapid reversal of symptoms. Suitable supportive measures such as maintaining a clear airway and adequate hydration should be employed.
Motor Restlessness
- Symptoms may include agitation or jitteriness and sometimes insomnia. These symptoms often disappear spontaneously. At times these symptoms may be similar to the original neurotic or psychotic symptoms. Dosage should not be increased until these side effects have subsided.
- If these symptoms become too troublesome, they can usually be controlled by a reduction of dosage or change of drug. Treatment with antiparkinsonian agents, benzodiazepines or propranolol may be helpful.
Dystonia
- Class effect: Symptoms of dystonia, prolonged abnormal contractions of muscle groups, may occur in susceptible individuals during the first few days of treatment. Dystonic symptoms include: spasm of the neck muscles, sometimes progressing to tightness of the throat, swallowing difficulty, difficulty breathing, and/or protrusion of the tongue. While these symptoms can occur at low doses, they occur more frequently and with greater severity with high potency and at higher doses of first generation antipsychotic drugs. An elevated risk of acute dystonia is observed in males and younger age groups.
Pseudo-parkinsonism
- Symptoms may include: mask-like faces; drooling; tremors; pillrolling motion; cogwheel rigidity; and shuffling gait. Reassurance and sedation are important. In most cases these symptoms are readily controlled when an anti-parkinsonism agent is administered concomitantly. Anti-parkinsonism agents should be used only when required. Generally, therapy of a few weeks to 2 or 3 months will suffice. After this time patients should be evaluated to determine their need for continued treatment. (Note: Levodopa has not been found effective in pseudo-parkinsonism.) Occasionally it is necessary to lower the dosage of prochlorperazine or to discontinue the drug.
Tardive Dyskinesia
- As with all antipsychotic agents, tardive dyskinesia may appear in some patients on long-term therapy or may appear after drug therapy has been discontinued. The syndrome can also develop, although much less frequently, after relatively brief treatment periods at low doses. This syndrome appears in all age groups. Although its prevalence appears to be highest among elderly patients, especially elderly women, it is impossible to rely upon prevalence estimates to predict at the inception of antipsychotic treatment which patients are likely to develop the syndrome. The symptoms are persistent and in some patients appear to be irreversible. The syndrome is characterized by rhythmical involuntary movements of the tongue, face, mouth or jaw (e.g., protrusion of tongue, puffing of cheeks, puckering of mouth, chewing movements). Sometimes these may be accompanied by involuntary movements of extremities. In rare instances, these involuntary movements of the extremities are the only manifestations of tardive dyskinesia. A variant of tardive dyskinesia, tardive dystonia, has also been described.
- There is no known effective treatment for tardive dyskinesia; anti-parkinsonism agents do not alleviate the symptoms of this syndrome. It is suggested that all antipsychotic agents be discontinued if these symptoms appear. Should it be necessary to reinstitute treatment, or increase the dosage of the agent, or switch to a different antipsychotic agent, the syndrome may be masked.
- It has been reported that fine vermicular movements of the tongue may be an early sign of the syndrome and if the medication is stopped at that time the syndrome may not develop.
Contact Dermatitis
- Avoid getting the injection solution on hands or clothing because of the possibility of contact dermatitis.
- Adverse Reactions Reported with Prochlorperazine or Other Phenothiazine Derivatives Adverse reactions with different phenothiazines vary in type, frequency and mechanism of occurrence, i.e., some are dose-related, while others involve individual patient sensitivity. Some adverse reactions may be more Iikely to occur, or occur with greater intensity, in patients with special medical problems, e.g., patients with mitral insufficiency or pheochromocytoma have experienced severe hypotension following recommended doses of certain phenothiazines.
- Not all of the following adverse reactions have been observed with every phenothiazine derivative, but they have been reported with 1 or more and should be borne in mind when drugs of this class are administered: extrapyramidal symptoms (opisthotonos, oculogyric crisis, hyperreflexia, dystonia, akathisia, dyskinesia, parkinsonism) some of which have lasted months and even years -- particularly in elderly patients with previous brain damage; grand mal and petit mal convulsions, particularly in patients with EEG abnormalities or history of such disorders; altered cerebrospinal fluid proteins; cerebral edema; intensification and prolongation of the action of central nervous system depressants (opiates, analgesics, antihistamines, barbiturates, alcohol), atropine, heat, organophosphorus insecticides; autonomic reactions (dryness of mouth, nasal congestion, headache, nausea, constipation, obstipation, adynamic ileus, ejaculatory disorders/impotence, priapism, atonic colon, urinary retention, miosis and mydriasis); reactivation of psychotic processes, catatonic-like states; hypotension (sometimes fatal); cardiac arrest; blood dyscrasias (pancytopenia, thrombocytopenic purpura, leukopenia, agranulocytosis, eosinophilia, hemolytic anemia, aplastic anemia; liver damage (jaundice, biliary stasis); endocrine disturbances (hyperglycemia, hypoglycemia, glycosuria, lactation, galactorrhea, gynecomastia, menstrual irregularities, false-positive pregnancy tests); skin disorders (photosensitivity, itching, erythema, urticaria, eczema up to exfoliative dermatitis); other allergic reactions (asthma, laryngeal edema, angioneurotic edema, anaphylactoid reactions); peripheral edema; reversed epinephrine effect; hyperpyrexia; mild fever after large I.M. doses; increased appetite; increased weight; a systemic lupus erythematosus-like syndrome; pigmentary retinopathy; with prolonged administration of substantial doses, skin pigmentation, epithelial keratopathy, and lenticular and corneal deposits.
- EKG changes -- particularly nonspecific, usually reversible Q and T wave distortions -- have been observed in some patients receiving phenothiazine tranquilizers.
- Although phenothiazines cause neither psychic nor physical dependence, sudden discontinuance in long-term psychiatric patients may cause temporary symptoms, e.g., nausea and vomiting, dizziness, tremulousness.
Note: There have been occasional reports of sudden death in patients receiving phenothiazines. In some cases, the cause appeared to be cardiac arrest or asphyxia due to failure of the cough reflex.
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Prochlorperazine (injection) in the drug label.
Drug Interactions
There is limited information regarding Prochlorperazine (injection) Drug Interactions in the drug label.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): C
There is no FDA guidance on usage of Prochlorperazine (injection) in women who are pregnant.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Prochlorperazine (injection) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Prochlorperazine (injection) during labor and delivery.
Nursing Mothers
- There is evidence that phenothiazines are excreted in the breast milk of nursing mothers. *Caution should be exercised when prochlorperazine is administered to a nursing woman.
Pediatric Use
There is no FDA guidance on the use of Prochlorperazine (injection) with respect to pediatric patients.
Geriatic Use
There is no FDA guidance on the use of Prochlorperazine (injection) with respect to geriatric patients.
Gender
There is no FDA guidance on the use of Prochlorperazine (injection) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Prochlorperazine (injection) with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Prochlorperazine (injection) in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Prochlorperazine (injection) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Prochlorperazine (injection) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Prochlorperazine (injection) in patients who are immunocompromised.
Administration and Monitoring
Administration
Monitoring
There is limited information regarding Monitoring of Prochlorperazine (injection) in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Prochlorperazine (injection) in the drug label.
Overdosage
Symptoms:
- Primarily involvement of the extrapyramidal mechanism producing some of the dystonic reactions described above.
- Symptoms of central nervous system depression to the point of somnolence or coma. Agitation and restlessness may also occur. Other possible manifestations include convulsions, EKG changes and cardiac arrhythmias, fever and autonomic reactions such as hypotension, dry mouth and ileus.
Treatment:
- It is important to determine other medications taken by the patient since multiple-dose therapy is common in overdosage situations. Treatment is essentially symptomatic and supportive. Early gastric lavage is helpful. Keep patient under observation and maintain an open airway, since involvement of the extrapyramidal mechanism may produce dysphagia and respiratory difficulty in severe overdosage. Do not attempt to induce emesis because a dystonic reaction of the head or neck may develop that could result in aspiration of vomitus. Extrapyramidal symptoms may be treated with anti-parkinsonism drugs, barbiturates or Benadryl. See prescribing information for these products. Care should be taken to avoid increasing respiratory depression.
- If administration of a stimulant is desirable, amphetamine, dextroamphetamine or caffeine with sodium benzoate is recommended.
- Stimulants that may cause convulsions (e.g., picrotoxin or pentylenetetrazol) should be avoided.
- If hypotension occurs, the standard measures for managing circulatory shock should be initiated. If it is desirable to administer a vasoconstrictor, Levophed and Neo-Synephrine are most suitable. Other pressor agents, including epinephrine, are not recommended because phenothiazine derivatives may reverse the usual elevating action of these agents and cause a further lowering of blood pressure.
- Limited experience indicates that phenothiazines are not dialyzable.
Pharmacology
Mechanism of Action
There is limited information regarding Prochlorperazine (injection) Mechanism of Action in the drug label.
Structure
- Prochlorperazine Edisylate Injection USP, 2-Chloro-10-[3-(4-methyl-1-piperazinyl)propyl]phenothiazine 1,2-ethanedisulfonate (1:1),
has the following structural formula:
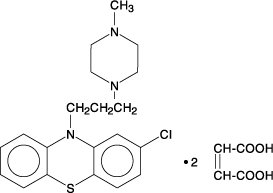
- Molecular Formula: C20H24CIN3S•C2H6O6S2 M.W. = 564.14
- Prochlorperazine Edisylate Injection, an antiemetic and antipsychotic, is a sterile solution intended for intramuscular or intravenous administration.
Each mL contains, in aqueous solution, 5 mg prochlorperazine as the edisylate salt, 5 mg sodium biphosphate, 12 mg sodium tartrate, 0.9 mg sodium saccharin and 0.75% benzyl alcohol as preservative. The pH range is 4.2 to 6.2.
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Prochlorperazine (injection) in the drug label.
Pharmacokinetics
There is limited information regarding Pharmacokinetics of Prochlorperazine (injection) in the drug label.
Nonclinical Toxicology
There is limited information regarding Nonclinical Toxicology of Prochlorperazine (injection) in the drug label.
Clinical Studies
There is limited information regarding Clinical Studies of Prochlorperazine (injection) in the drug label.
How Supplied
- Prochlorperazine Edisylate Injection USP is supplied as follows:
- 2 mL (5 mg/mL), in boxes of 10: NDC 55390-077-10
- 10 mL (5 mg/mL), individually boxed: NDC 55390-077-01
- Store prochlorperazine vials at 20° to 25°C (68° to 77°F). See USP controlled room temperature. Do not freeze. Protect from light.
Storage
There is limited information regarding Prochlorperazine (injection) Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Prochlorperazine (injection) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Prochlorperazine (injection) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Patient Counseling Information of Prochlorperazine (injection) in the drug label.
Precautions with Alcohol
- Alcohol-Prochlorperazine (injection) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Prochlorperazine (injection) Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Prochlorperazine (injection) Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Prochlorperazine (injection) |Label Name=Prochlorperazine (injection)02.png
}}
{{#subobject:
|Label Page=Prochlorperazine (injection) |Label Name=Prochlorperazine (injection)03.png
}}