Total parenteral nutrition
Editor-in-Chief: Kenneth Storch, M.D., Ph.D. [2], Director of Medical Nutrition, Overlook Hospital, Summit, NJ
Overview
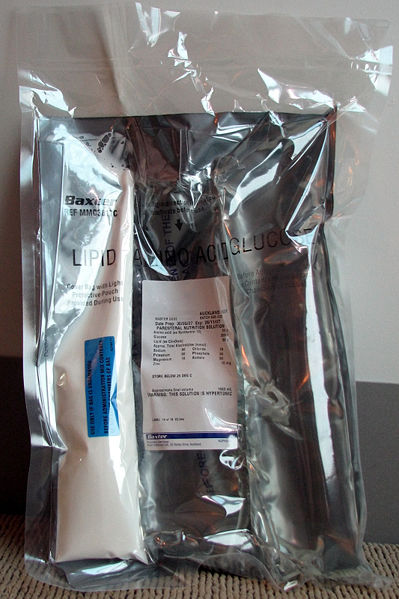
Total parenteral nutrition (TPN), is the practice of feeding a person intravenously, bypassing the usual process of eating and digestion. The person receives nutritional formulas containing salts, glucose, amino acids, lipids and added vitamins.
General Usage
TPN is normally used following surgery, when feeding by mouth or using the gut is not possible, when a person's digestive system cannot absorb nutrients due to chronic disease, or, alternatively, if a person's nutrient requirement cannot be met by enteral feeding (tube feeding) and supplementation. It has been used for comatose patients, although enteral feeding is usually preferable, and less prone to complications. Short-term TPN may be used if a person's digestive system has shut down (for instance by Peritonitis), and they are at a low enough weight to cause concerns about nutrition during an extended hospital stay. Long-term TPN is occasionally used to treat people suffering the extended consequences of an accident or surgery. Most controversially, TPN has extended the life of a small number of children born with nonexistent or severely birth-deformed guts. The oldest were eight years old in 2003.
The preferred method of delivering TPN is with a medical infusion pump. A sterile bag of nutrient solution, between 500 mL and 4 L is provided. The pump infuses a small amount (0.1 to 10 mL/hr) continuously in order to keep the vein open. Feeding schedules vary, but one common regimen ramps up the nutrition over a few hours, levels off the rate for a few hours, and then ramps it down over a few more hours, in order to simulate a normal set of meal times.
The nutrient solution consists of water, glucose, salts, amino acids, vitamins and (more controversially) sometimes emulsified fats. Long term TPN patients sometimes suffer from lack of trace nutrients or electrolyte imbalances. Because increased blood sugar commonly occurs with TPN, insulin may also be added to the infusion. Often though, an insignificant amount of insulin is added, sometimes 10 units or less in 2 liters of TPN. In actuality, the patient will probably get less than that. Occasionally, other drugs are added as well, sometimes unnecessarily.
Chronic TPN is performed through a central intravenous catheter, usually in the subclavian or jugular vein. Another common practice is to use a PICC line, which originates in the arm, and exends to one of the central veins, such as the subclavian. In infants, sometimes the umbilical vein is used.
Battery-powered ambulatory infusion pumps can be used with chronic TPN patients. Usually the pump and a small (100 ml) bag of nutrient (to keep the vein open) are carried in a small bag around the waist or on the shoulder. Outpatient TPN practices are still being refined.
Aside from their dependence on a pump, chronic TPN patients live quite normal lives.
TPN in Critical and/or Perioperative Care
Parenteral nutrition is indicated to prevent the adverse effects of malnutrition in patients who are unable to obtain adequate nutrients by oral or enteral routes. Other indications are short gut syndrome, high-output fistula, prolonged ileus, or bowel obstruction. However, the decision to initiate TPN needs to be made on an individual patient basis, as different patients will have differing abilities to tolerate starvation. [1]
The nutrient solution consists of water and electrolytes; glucose, amino acids, and lipids; essential vitamins, minerals and trace elements are added or given separately. Previously lipid emulsions were given separately but is becoming more common for a "three-in-one" solution of glucose, proteins, and lipids to be administered. [2] [3] [4] Complications are either related to Catheter insertion, or Metabolic (including the Refeeding Syndrome). Catheter complications include pneumothorax, accidental arterial puncture, and catheter-related sepsis. The complication rate at the time of insertion should be less than 5% [3]. Catheter-related infecions may be minimised by appropriate choice of catheter and insertion technique [5]. Metabolic complications include the Refeeding Syndrome characterized by hypophosphataemia and other electrolyte abnormalities. Hyperglycemia is common at the start of therapy, and hypoglycaemia is likely to occur with abrupt cessation of TPN. Liver dysfunction can be limited to a reversible cholestatic jaundice and to fatty infiltration (demonstrated by elevated transaminases). Severe hepatic dysfunction is a rare complication.[6]. Overall, patients receiving TPN have a higher rate of infectious complications. This is related to hyperglycemia [7]
Complications
The most common complication of TPN use is bacterial infection, usually due to the increased infection risk from having an indwelling central venous catheter. In patients with frequent bacterial infections, fungal infections can also occur. Liver failure, often related to Fatty liver, may sometimes occur. This condition is due to the difficulty in processing food taken in directly into the bloodstream.
Two related complications of TPN are venous thrombosis and rarely priapism. Fat infusion during TPN is assumed to contribute to both.[8]
Other complications of TPN are related to the difficulties the body has processing TPN. One complication is non-anion gap metabolic acidosis.
Total parenteral nutrition would increases the risk of acute cholecystitis due to complete unusage of gastrointestinal tract, which may result in bile stasis in the gallbladder. The risk of acute cholecystitis is increased accordingly.
A recent small-scale study at Children's Hospital Boston on the cause of liver failure suggests it may be due to a large difference in omega-6 to omega-3 ratio. When treated with Omegaven, a different fatty acid infusion (which is approved for limited use in the U.S.), two patients were able to recover from their condition.[9]
See also
References
- ↑ American Gastroenterological Association medical position statement: parenteral nutrition.[1]
- ↑ Didier M, Fischer S, Maki D. Total nutrient admixtures appear safer than lipid emulsion alone as regards microbial contamination. J Parenteral Enteral Nutr 1998; 22: 291-6.
- ↑ CJ Rollins, VA Elsberry, KA Pollack, PF Pollack, and Udall JN Jr , Three-in-one parenteral nutrition: a safe and economical method of nutritional support for infants, Journal of Parenteral and Enteral Nutrition, Vol 14, Issue 3, 290-294
- ↑ Kozier, B., & Erb, G., & Berman, A.J., & Burke, K., & Bouchal, S. R., & Hirst, S. P.. (2004). Fundamentals of Nursing: The Nature of Nursing Practice in Canada. Canadian Edition. Prentice Hall Health: Toronto.
- ↑ Horattas M, Trupiano J, Hopkins S, Pasini D, Martino C, Murty A. Changing concepts in long-term central venous access: catheter selection and cost savings. Am J Infect Control 2001; 29: 32-40
- ↑ G. Edward Morgan, Jr., Maged S. Mikhail, Michael J. MurrayClinical Anesthesiology, 4th Edition
- ↑ McCowen K, Friel C, Sternberg J et al. Hypocaloric total parenteral nutrition: effectiveness in prevention of hyperglycemia and infectious complications--a randomised clinical trial. Crit Care Med 2000; 28: 3606-11.
- ↑ X Hebuterne, AM Frere, J Bayle, and P Rampal Priapism in a patient treated with total parenteral nutrition Journal of Parenteral and Enteral Nutrition Vol. 16 No. 2 1992 p171-174
- ↑ Gura KM, Duggan CP, Collier SB, et al. Reversal of parenteral nutrition-associated liver disease in two infants with short bowel syndrome using parenteral fish oil: implications for future management. Pediatrics Vol. 118 No. 1 July 2006 p197-201
External links
- American Society for Parenteral and Enteral Nutrition
- TPN/PPN Calculator by Ryan Heinrick
- "Why does prolonged TPN cause liver damage in infants?", Children's Hospital Boston
- TPN-associated Liver Disease
- TPN Blogs on Nutrishare (a Home TPN provider)
- TPN Drug Information from MedlinePlus NIH Database
- TPN Care from the World Health Library