Prednisolone (injection)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Kiran Singh, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Prednisolone (injection) is a corticosteroid that is FDA approved for the treatment of leukemias, lymphomas, asthma, atopic dermatitis, contact dermatitis, bullous dermatitis herpetiformis,adrenocortical insufficiency,ulcerative colitis, idiopathic thrombocytopenic purpura, uveitis. Common adverse reactions include anaphylaxis, angioedema, bradycardia, nausea, pancreatitis, peptic ulcer, thromboembolism, thrombophlebitis, vasculitis, acne, allergic dermatitis.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
When oral therapy is not feasible, and the strength, dosage form and route of administration of the drug reasonably lend the preparation to the treatment of the condition, A-METHAPRED™ sterile powder is indicated for intravenous or intramuscular use in the following conditions:
- Allergic states: Control of severe or incapacitating allergic conditions intractable to adequate trials of conventional treatment in asthma, atopic dermatitis, contact dermatitis, drug hypersensitivity reactions, perennial or seasonal allergic rhinitis, serum sickness, transfusion reactions.
- Dermatologic diseases: Bullous dermatitis herpetiformis, exfoliative erythroderma, mycosis fungoides, pemphigus, severe erythema multiforme (Stevens-Johnson syndrome).
- Endocrine disorders: Primary or secondary adrenocortical insufficiency (hydrocortisone or cortisone is the drug of choice; synthetic analogs may be used in conjunction with mineralocorticoids where applicable; in infancy, mineralocorticoid supplementation is of particular importance), congenital adrenal hyperplasia, hypercalcemia associated with cancer, non suppurative thyroiditis.
- Gastrointestinal diseases: To tide the patient over a critical period of the disease in regional enteritis (systemic therapy) and ulcerative colitis.
- Hematologic disorders: Acquired (autoimmune) hemolytic anemia, congenital (erythroid) hypoplastic anemia (Diamond-Blackfan anemia), idiopathic thrombocytopenic purpura in adults (intravenous administration only; intramuscular administration is contraindicated), pure red cell aplasia, selected cases of secondary thrombocytopenia.
- Miscellaneous: Trichinosis with neurologic or myocardial involvement, tuberculous meningitis with subarachnoid block or impending block when used concurrently with appropriate antituberculous chemotherapy.
- Neoplastic diseases: For the palliative management of leukemias and lymphomas.
- Nervous System: Acute exacerbations of multiple sclerosis; cerebral edema associated with primary or metastatic brain tumor, or craniotomy.
- Ophthalmic diseases: Sympathetic ophthalmia, uveitis and ocular inflammatory conditions unresponsive to topical corticosteroids.
- Renal diseases: To induce diuresis or remission of proteinuria in idiopathic nephrotic syndrome or that due to lupus erythematosus.
- Respiratory diseases: Berylliosis, fulminating or disseminated pulmonary tuberculosis when used concurrently with appropriate antituberculous chemotherapy, idiopathic eosinophilic pneumonias, symptomatic sarcoidosis.
- Rheumatic disorders: As adjunctive therapy for short-term administration (to tide the patient over an acute episode or exacerbation) in acute gouty arthritis; acute rheumatic carditis; ankylosing spondylitis; psoriatic arthritis; rheumatoid arthritis, including juvenile rheumatoid arthritis (selected cases may require low-dose maintenance therapy). For the treatment of dermatomyositis, temporal arteritis, polymyositis, and systemic lupus erythematosus.
Dosage
NOTE: CONTAINS BENZYL ALCOHOL
- Because of possible physical incompatibilities, A-METHAPRED™, should not be diluted or mixed with other solutions.
- Use only Bacteriostatic Water For Injection with Benzyl Alcohol when reconstituting A-METHAPRED™. Use within 48 hours after mixing.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
- This preparation may be administered by intravenous injection, by intravenous infusion, or by intramuscular injection, the preferred method for initial emergency use being intravenous injection. Following the initial emergency period, consideration should be given to employing a longer acting injectable preparation or an oral preparation.
- There are reports of cardiac arrhythmias and/or cardiac arrest following the rapid administration of large IV doses of methylprednisolone (greater than 0.5 gram administered over a period of less than 10 minutes). Bradycardia has been reported during or after the administration of large doses of methylprednisolone sodium succinate, and may be unrelated to the speed or duration of infusion.
- When high dose therapy is desired, the recommended dose of A-METHAPRED™ Sterile Powder is 30 mg/kg administered intravenously over at least 30 minutes. This dose may be repeated every 4 to 6 hours for 48 hours.
- In general, high dose corticosteroid therapy should be continued only until the patient’s condition has stabilized; usually not beyond 48 to 72 hours.
- In other indications initial dosage will vary from 10 to 40 mg of methylprednisolone depending on the specific disease entity being treated. However, in certain overwhelming, acute, life-threatening situations, administrations in dosages exceeding the usual dosages may be justified and may be in multiples of the oral dosages.
- It Should Be Emphasized that Dosage Requirements are Variable and Must Be Individualized on the Basis of the Disease Under Treatment and the Response of the Patient. After a favorable response is noted, the proper maintenance dosage should be determined by decreasing the initial drug dosage in small decrements at appropriate time intervals until the lowest dosage which will maintain an adequate clinical response is reached. Situations which may make dosage adjustments necessary are changes in clinical status secondary to remissions or exacerbations in the disease process, the patient’s individual drug responsiveness, and the effect of patient exposure to stressful situations not directly related to the disease entity under treatment. In this latter situation it may be necessary to increase the dosage of the corticosteroid for a period of time consistent with the patient’s condition. If after long-term therapy the drug is to be stopped, it is recommended that it be withdrawn gradually rather than abruptly.
- A-METHAPRED™ may be administered by intravenous or intramuscular injection or by intravenous infusion, the preferred method for initial emergency use being intravenous injection. To administer by intravenous (or intramuscular) injection, prepare solution as directed. The desired dose may be administered intravenously over a period of several minutes.
- Dosage may be reduced for infants and children but should be governed more by the severity of the condition and response of the patient than by age or size. It should not be less than 0.5 mg per kg every 24 hours.
- Dosage must be decreased or discontinued gradually when the drug has been administered for more than a few days. If a period of spontaneous remission occurs in a chronic condition, treatment should be discontinued. Routine laboratory studies, such as urinalysis, two-hour postprandial blood sugar, determination of blood pressure and body weight, and a chest X-ray should be made at regular intervals during prolonged therapy. Upper GI X-rays are desirable in patients with an ulcer history or significant dyspepsia.
- To prepare solutions for intravenous infusion, first prepare the solution for injection as directed. This solution may then be added to indicated amounts of 5% dextrose in water, isotonic saline solution or 5% dextrose in isotonic saline solution.
- In pediatric patients, the initial dose of methylprednisolone may vary depending on the specific disease entity being treated. The range of initial doses is 0.11 to 1.6 mg/kg/day in three or four divided doses (3.2 to 48 mg/m2bsa/day).
- The National Heart, Lung, and Blood Institute (NHLBI) recommended dosing for systemic prednisone, prednisolone or methylprednisolone in pediatric patients whose asthma is uncontrolled by inhaled corticosteroids and long-acting bronchodilators is 1-2 mg/kg/day in single or divided doses. It is further recommended that short course, or “burst” therapy, be continued until the patient achieves a peak expiratory flow rate of 80% of his or her personal best or symptoms resolve. This usually requires 3 to 10 days of treatment, although it can take longer. There is no evidence that tapering the dose after improvement will prevent a relapse.
- In treatment of acute exacerbations of multiple sclerosis, daily doses of 160 mg of methylprednisolone for a week followed by 64 mg every other day for 1 month have been shown to be effective.
- For the purpose of comparison, the following is the equivalent milligram dosage of the various glucocorticoids:
- Glucocorticoids:
Cortisone, 25 Triamcinolone, 4
Hydrocortisone, 20 Paramethasone, 2
Prednisolone, 5 Betamethasone, 0.75
Prednisone, 5 Dexamethasone, 0.75
Methylprednisolone, 4
- These dose relationships apply only to oral or intravenous administration of these compounds. When these substances or their derivatives are injected intramuscularly or into joint spaces, their relative properties may be greatly altered.
- Directions for Reconstitution
- Remove protective cap.
- Cleanse stopper with suitable germicide.
- Aseptically add 1 mL Bacteriostatic Water for Injection, USP (with benzyl alcohol) for the 40 mg vial or 2 mL Bacteriostatic Water for Injection, USP (with benzyl alcohol) for the 125 mg vial.
- Agitate to effect solution.
- Invert vial. Insert needle through target area of stopper until tip is just visible. Withdraw dose.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Indications and Dosage
- When used for more than a few days, methylprednisolone should be decreased or discontinued gradually.
- Acute lymphoid leukemia, Palliative: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Allergic condition, Severe or intractable: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Asthma: (moderate and severe exacerbation; NHLBI asthma guidelines) 40 to 80 mg/day IV in 1 or 2 divided doses until peak expiratory flow reaches 70% of predicted or personal best.
- Carcinoma of breast: Optimal dosing and timing not yet defined.
- Collagen disease: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Crohn's disease: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Disorder of endocrine system: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hour.
- Disorder of eye: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Disorder of hematopoietic structure: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Disorder of respiratory system: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Disorder of skin: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Exacerbation of multiple sclerosis (Acute): 160 mg IV or IM daily for 1 week, followed by 64 mg every other day for 1 month.
- Fever, due to malignancy: Optimal dosing and timing not yet defined.
- Hypercalcemia of malignancy: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Idiopathic thrombocytopenic purpura: initial dose, 10 to 40 mg IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Inflammatory disorder of musculoskeletal system; Adjunct: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Intracranial tumor, Primary: Optimal dosing and timing not yet established.
- Multiple myeloma: Optimal dosing and timing not yet established.
- Mycosis fungoides: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Nephrotic syndrome: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Pneumocystis pneumonia (Moderate to Severe); Adjunct: IV, 30 mg twice daily on days 1 to 5, 30 mg once a day on days 6 to 10, 15 mg once a day on days 11 to 21; begin as early as possible and within 72 hours of Pneumocystis carinii pneumonia therapy.
- Prostate cancer: Optimal dosing and timing not yet defined.
- Pulmonary tuberculosis; Adjunct: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Rheumatoid carditis, Acute; Adjunct: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Temporal arteritis: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Trichinosis, With neurologic and myocardial involvement: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Tuberculosis of meninges, With subarachnoid block or impending block; Adjunct: initial dose, 10 to 40 mg IM or IV over at least several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
- Ulcerative colitis: initial dose, 10 to 40 mg IM or IV over several minutes; for high-dose therapy, 30 mg/kg IV over at least 30 minutes, may repeat every 4 to 6 hours for up to 72 hours.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Prednisolone in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Prednisolone (injection) FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
Indications and Dosage
- when used for more than a few days, methylpredniSolone should be decreased or discontinued gradually.
- Acute lymphoid leukemia, Palliative: older than 1 month, initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Allergic condition, Severe or intractable: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Asthma: (moderate and severe exacerbation, 12 years or younger; NHLBI asthma guidelines) 1 to 2 mg/kg/day IV in 2 divided doses (maximum 60 mg/day) until peak expiratory flow reaches 70% of predicted or personal best [6], for infants and children may reduce dose but to no less than 0.5 mg/kg/day.
- Asthma: (moderate and severe exacerbation, over 12 years; NHLBI asthma guidelines) 40 to 80 mg/day IV in 1 or 2 divided doses until peak expiratory flow reaches 70% of predicted or personal best.
- Collagen disease: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Crohn's disease: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Disorder of endocrine system: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Disorder of eye: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Disorder of hematopoietic structure: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Disorder of respiratory system: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Disorder of skin: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Hypercalcemia of malignancy: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Inflammatory disorder of musculoskeletal system; Adjunct: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Mycosis fungoides: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Nephrotic syndrome: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Pneumocystis pneumonia (Moderate to Severe); Adjunct: IV (adolescents), 30 mg twice daily on days 1 to 5, 30 mg once a day on days 6 to 10, 15 mg once a day on days 11 to 21; begin as early as possible and within 72 hours of Pneumocystis carinii pneumonia therapy.
- Pneumocystis pneumonia (Moderate to Severe); Adjunct: IV (infants and children), 1 mg/kg every 6 hours on days 1 to 7, 1 mg/kg twice daily on days 8 to 9, 0.5 mg/kg twice daily on days 10 to 11, 1 mg/kg once a day on days 12 to 16; begin as early as possible and within 72 hours of Pneumocystis carinii pneumonia therapy.
- Pulmonary tuberculosis; Adjunct: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Rheumatoid carditis, Acute; Adjunct: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Temporal arteritis: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Trichinosis, With neurologic and myocardial involvement: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Tuberculosis of meninges, With subarachnoid block or impending block; Adjunct: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
- Ulcerative colitis: initial dose, 0.11 to 1.6 mg/kg/day (3.2 to 48 mg/m(2)/day) IM or IV over at least several minutes in 3 to 4 divided doses.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Prednisolone in pediatric patients.
Contraindications
A-METHAPRED™ sterile powder is contraindicated:
- In systemic fungal infections and patients with known hypersensitivity to the product and its constituents.
- For intrathecal administration. Reports of severe medical events have been associated with this route of administration.
- Intramuscular corticosteroid preparations are contraindicated for idiopathic thrombocytopenic purpura.
- Additional contraindication for the use of A-METHAPRED™ sterile powder preserved with benzyl alcohol:
- Formulations preserved with benzyl alcohol are contraindicated for use in premature infants.
Warnings
General
- Reconstituted A-METHAPRED™ contains benzyl alcohol, which is potentially toxic when administered locally to neural tissue. Exposure to excessive amounts of benzyl alcohol has been associated with toxicity (hypotension, metabolic acidosis), particularly in neonates, and an increased incidence of kernicterus, particularly in small preterm infants. There have been rare reports of deaths, primarily in preterm infants, associated with exposure to excessive amounts of benzyl alcohol. The amount of benzyl alcohol from medications is usually considered negligible compared to that received in flush solutions containing benzyl alcohol. Administration of high dosages of medications containing this preservative must take into account the total amount of benzyl alcohol administered. The amount of benzyl alcohol at which toxicity may occur is not known. If the patient requires more than the recommended dosages or other medications containing this preservative, the practitioner must consider the daily metabolic load of benzyl alcohol from these combined sources.
- Injection of methylprednisolone may result in dermal and/or subdermal changes forming depressions in the skin at the injection site. In order to minimize the incidence of dermal and subdermal atrophy, care must be exercised not to exceed recommended doses in injections. Injection into the deltoid muscle should be avoided because of a high incidence of subcutaneous atrophy.
- Rare instances of anaphylactoid reactions have occurred in patients receiving corticosteroid therapy.
- Increased dosage of rapidly acting corticosteroids is indicated in patients on corticosteroid therapy subjected to any unusual stress before, during, and after the stressful situation.
- Results from one multicenter, randomized, placebo controlled study with methylprednisolone hemisuccinate, an IV corticosteroid, showed an increase in early (at 2 weeks) and late (at 6 months) mortality in patients with cranial trauma who were determined not to have other clear indications for corticosteroid treatment. High doses of systemic corticosteroids, including A-METHAPRED™, should not be used for the treatment of traumatic brain injury.
Cardio-renal
- Average and large doses of corticosteroids can cause elevation of blood pressure, salt and water retention, and increased excretion of potassium. These effects are less likely to occur with the synthetic derivatives except when used in large doses. Dietary salt restriction and potassium supplementation may be necessary. All corticosteroids increase calcium excretion.
- Literature reports suggest an apparent association between use of corticosteroids and left ventricular free wall rupture after a recent myocardial infarction; therefore, therapy with corticosteroids should be used with great caution in these patients.
Endocrine
- Hypothalamic-pituitary adrenal (HPA) axis suppression. Cushing’s syndrome, and hyperglycemia. Monitor patients for these conditions with chronic use. Corticosteroids can produce reversible HPA axis suppression with the potential for glucocorticosteroid insufficiency after withdrawal of treatment. Drug induced secondary adrenocortical insufficiency may be minimized by gradual reduction of dosage. This type of relative insufficiency may persist for months after discontinuation of therapy; therefore, in any situation of stress occurring during that period, hormone therapy should be reinstituted.
Infections
General
- Patients who are on corticosteroids are more susceptible to infections than are healthy individuals. There may be decreased resistance and inability to localize infection when corticosteroids are used. Infection with any pathogen (viral, bacterial, fungal, protozoan or helminthic) in any location of the body may be associated with the use of corticosteroids alone or in combination with other immunosuppressive agents.
- These infections may be mild, but can be severe and at times fatal. With increasing doses of corticosteroids, the rate of occurrence of infectious complications increases. Corticosteroids may also mask some signs of current infection. Do not use intraarticularly, intrabursally or for intratendinous administration for local effect in the presence of acute local infection.
- A study has failed to establish the efficacy of methylprednisolone sodium succinate in the treatment of sepsis syndrome and septic shock. The study also suggests that treatment of these conditions with methylprednisolone sodium succinate may increase the risk of mortality in certain patients (i.e., patients with elevated serum creatinine levels or patients who develop secondary infections after methylprednisolone sodium succinate).
Fungal infections
- Corticosteroids may exacerbate systemic fungal infections and therefore should not be used in the presence of such infections unless they are needed to control drug reactions. There have been cases reported in which concomitant use of amphotericin B and hydrocortisone was followed by cardiac enlargement and congestive heart failure.
Special pathogens
- Latent disease may be activated or there may be an exacerbation of intercurrent infections due to pathogens, including those caused by Amoeba, Candida, Cryptococcus, Mycobacterium, Nocardia, Pneumocystis, Toxoplasma.
- It is recommended that latent amebiasis or active amebiasis be ruled out before initiating corticosteroid therapy in any patient who has spent time in the tropics or in any patient with unexplained diarrhea.
- Similarly, corticosteroids should be used with great care in patients with known or suspected Strongyloides (threadworm) infestation. In such patients, corticosteroid-induced immunosuppression may lead to Strongyloides hyperinfection and dissemination with widespread larval migration, often accompanied by severe enterocolitis and potentially fatal gram-negative septicemia.
- Corticosteroids should not be used in cerebral malaria. There is currently no evidence of benefit from steroids in this condition.
Tuberculosis
- The use of corticosteroids in active tuberculosis should be restricted to those cases of fulminating or disseminated tuberculosis in which the corticosteroid is used for the management of the disease in conjunction with an appropriate antituberculous regimen.
- If corticosteroids are indicated in patients with latent tuberculosis or tuberculin reactivity, close observation is necessary as reactivation of the disease may occur. During prolonged corticosteroid therapy these patients should receive chemoprophylaxis.
Vaccination
- Administration of live or live, attenuated vaccines is contraindicated in patients receiving immunosuppressive doses of corticosteroids. Killed or inactivated vaccines may be administered. However, the response to such vaccines can not be predicted. Immunization procedures may be undertaken in patients who are receiving corticosteroids as replacement therapy, e.g., for Addison’s disease.
Viral infections
- Chicken pox and measles can have a more serious or even fatal course in pediatric and adult patients on corticosteroids. In pediatric and adult patients who have not had these diseases, particular care should be taken to avoid exposure. The contribution of the underlying disease and/or prior corticosteroid treatment to the risk is also not known. If exposed to chicken pox, prophylaxis with varicella zoster immune globulin (VZIG) may be indicated. If exposed to measles, prophylaxis with immunoglobulin (IG) may be indicated. If chicken pox develops, treatment with antiviral agents should be considered.
Neurologic
- Reports of severe medical events have been associated with the intrathecal route of administration.
Ophthalmic
- Use of corticosteroids may produce posterior subcapsular cataracts, glaucoma with possible damage to the optic nerves, and may enhance the establishment of secondary ocular infections due to bacteria, fungi, or viruses. The use of oral corticosteroids is not recommended in the treatment of optic neuritis and may lead to an increase in the risk of new episodes. Corticosteroids should be used cautiously in patients with ocular herpes simplex because of corneal perforation. Corticosteroids should not be used in active ocular herpes simplex.
Adverse Reactions
Clinical Trials Experience
The following adverse reactions have been reported with methylprednisolone or other corticosteroids:
- Allergic reactions: Allergic or hypersensitivity reactions, anaphylactoid reaction, anaphylaxis, angioedema.
- Cardiovascular: bradycardia, cardiac arrest, cardiac arrhythmias, cardiac enlargement, circulatory collapse, congestive heart failure, fat embolism, hypertension, hypertrophic cardiomyopathy in premature infants, myocardial rupture following recent myocardial infarction , pulmonary edema, syncope, tachycardia, thromboembolism, thrombophlebitis, vasculitis.
- Dermatologic: Acne, allergic dermatitis, burning or tingling (especially in the perineal area, after intravenous injection), cutaneous and subcutaneous atrophy, dry scaly skin, ecchymoses and petechiae, edema, erythema, hyperpigmentation, hypopigmentation, impaired wound healing, increased sweating, rash, sterile abscess, striae, suppressed reactions to skin tests, thin fragile skin, thinning scalp hair, urticaria.
- Endocrine: Decreased carbohydrate and glucose tolerance, development of cushingoid state, glycosuria, hirsutism, hypertrichosis, increased requirements for insulin or oral hypoglycemic agents in diabetes, manifestations of latent diabetes mellitus, menstrual irregularities, secondary adrenocortical and pituitary unresponsiveness (particularly in times of stress, as in trauma, surgery, or illness), suppression of growth in pediatric patients.
- Fluid and electrolyte disturbances: Congestive heart failure in susceptible patients, fluid retention, hypokalemic alkalosis, potassium loss, sodium retention.
- Gastrointestinal: Abdominal distention, bowel/bladder dysfunction (after intrathecal administration), elevation in serum liver enzyme levels (usually reversible upon discontinuation), hepatomegaly, increased appetite, nausea, pancreatitis, peptic ulcer with possible perforation and hemorrhage, perforation of the small and large intestine (particularly in patients with inflammatory bowel disease), ulcerative esophagitis.
- Metabolic: Negative nitrogen balance due to protein catabolism.
- Musculoskeletal: Aseptic necrosis of femoral and humeral heads, Charcot-like arthropathy, loss of muscle mass, muscle weakness, osteoporosis, pathologic fracture of long bones, postinjection flare (following intra-articular use), steroid myopathy, tendon rupture, vertebral compression fractures.
- Neurologic/Psychiatric: Convulsions, depression, emotional instability, euphoria, headache, increased intracranial pressure with papilledema (pseudotumor cerebri) usually following discontinuation of treatment, insomnia, mood swings, neuritis, neuropathy, paresthesia, personality changes, psychic disorders, vertigo. Arachnoiditis, meningitis, paraparesis/paraplegia, and sensory disturbances have occurred after intrathecal administration.
- Ophthalmic: Exophthalmos, glaucoma, increased intraocular pressure, posterior subcapsular cataracts, rare instances of blindness associated with periocular injections.
- Other: Abnormal fat deposits, decreased resistance to infection, hiccups, increased or decreased motility and number of spermatozoa, injection site infections following non-sterile administration , malaise, moon face, weight gain.
Postmarketing Experience
There is limited information regarding Prednisolone (injection) Postmarketing Experience in the drug label.
Drug Interactions
- Aminoglutethimide: Aminoglutethimide may lead to a loss of corticosteroid-induced adrenal suppression.
- Amphotericin B injection and potassium-depleting agents: When corticosteroids are administered concomitantly with potassium-depleting agents (i.e., amphotericin-B, diuretics), patients should be observed closely for development of hypokalemia. There have been cases reported in which concomitant use of amphotericin B and hydrocortisone was followed by cardiac enlargement and congestive heart failure.
- Antibiotics: Macrolide antibiotics have been reported to cause a significant decrease in corticosteroid clearance.
- Anticholinesterases: Concomitant use of anticholinesterase agents and corticosteroids may produce severe weakness in patients with myasthenia gravis. If possible, anticholinesterase agents should be withdrawn at least 24 hours before initiating corticosteroid therapy.
- Anticoagulants, oral: Coadministration of corticosteroids and warfarin usually results in inhibition of response to warfarin, although there have been some conflicting reports. Therefore, coagulation indices should be monitored frequently to maintain the desired anticoagulant effect.
- Antidiabetics: Because corticosteroids may increase blood glucose concentrations, dosage adjustments of antidiabetic agents may be required.
- Antitubercular drugs: Serum concentrations of isoniazid may be decreased.
- Cholestyramine: Cholestyramine may increase the clearance of corticosteroids.
- Cyclosporine: Increased activity of both cyclosporine and corticosteroids may occur when the two are used concurrently. Convulsions have been reported with this concurrent use.
- Digitalis glycosides: Patients on digitalis glycosides may be at increased risk of arrhythmias due to hypokalemia.
- Estrogens, including oral contraceptives: Estrogens may decrease the hepatic metabolism of certain corticosteroids, thereby increasing their effect.
- Hepatic Enzyme Inducers (e.g., barbiturates, phenytoin, carbamazepine, rifampin): Drugs which induce cytochrome P450 3A enzyme activity may enhance the metabolism of corticosteroids and require that the dosage of the corticosteroid be increased.
- Hepatic Enzyme Inhibitors (e.g., ketoconazole, macrolide antibiotics such as erythromycin and troleandomycin): Drugs which inhibit cytochrome P450 3A4 have the potential to result in increased plasma concentrations of corticosteroids.
- Ketoconazole: Ketoconazole has been reported to significantly decrease the metabolism of certain corticosteroids by up to 60%, leading to an increased risk of corticosteroid side effects.
- Nonsteroidal anti-inflammatory agents (NSAIDS): Concomitant use of aspirin (or other non steroidal anti-inflammatory agents) and corticosteroids increases the risk of gastrointestinal side effects. Aspirin should be used cautiously in conjunction with corticosteroids in hypoprothrombinemia. The clearance of salicylates may be increased with concurrent use of corticosteroids.
- Skin tests: Corticosteroids may suppress reactions to skin tests.
- Vaccines: Patients on prolonged corticosteroid therapy may exhibit a diminished response to toxoids and live or inactivated vaccines due to inhibition of antibody response. Corticosteroids may also potentiate the replication of some organisms contained in live attenuated vaccines. Routine administration of vaccines or toxoids should be deferred until corticosteroid therapy is discontinued if possible.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): Pregnancy Category C.
Corticosteroids have been shown to be teratogenic in many species when given in doses equivalent to the human dose. Animal studies in which corticosteroids have been given to pregnant mice, rats, and rabbits have yielded an increased incidence of cleft palate in the offspring. There are no adequate and well-controlled studies in pregnant women. Corticosteroids should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Infants born to mothers who have received corticosteroids during pregnancy should be carefully observed for signs of hypoadrenalism.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Prednisolone (injection) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Prednisolone (injection) during labor and delivery.
Nursing Mothers
Systemically administered corticosteroids appear in human milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. Because of the potential for serious adverse reactions in nursing infants from corticosteroids, a decision should be made whether to continue nursing, or discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
- This product contains benzyl alcohol as a preservative. Benzyl alcohol, a component of this product, has been associated with serious adverse events and death, particularly in pediatric patients. The “gasping syndrome”, (characterized by central nervous system depression, metabolic acidosis, gasping respirations, and high levels of benzyl alcohol and its metabolites found in the blood and urine) has been associated with benzyl alcohol dosages >99 mg/kg/day in neonates and low-birth-weight neonates. Additional symptoms may include gradual neurological deterioration, seizures, intracranial hemorrhage, hematologic abnormalities, skin breakdown, hepatic and renal failure, hypotension, bradycardia, and cardiovascular collapse. Although normal therapeutic doses of this product deliver amounts of benzyl alcohol that are substantially lower than those reported in association with the “gasping syndrome”, the minimum amount of benzyl alcohol at which toxicity may occur is not known. Premature and low-birth-weight infants, as well as patients receiving high dosages, may be more likely to develop toxicity. Practitioners administering this and other medications containing benzyl alcohol should consider the combined daily metabolic load of benzyl alcohol from all sources.
- The efficacy and safety of corticosteroids in the pediatric population are based on the well established course of effect of corticosteroids which is similar in pediatric and adult populations. Published studies provide evidence of efficacy and safety in pediatric patients for the treatment of nephrotic syndrome (>2 years of age), and aggressive lymphomas and leukemias (>1 month of age). Other indications for pediatric use of corticosteroids, e.g., severe asthma and wheezing, are based on adequate and well-controlled trials conducted in adults, on the premises that the course of the diseases and their pathophysiology are considered to be substantially similar in both populations.
- The adverse effects of corticosteroids in pediatric patients are similar to those in adults. Like adults, pediatric patients should be carefully observed with frequent measurements of blood pressure, weight, height, intraocular pressure, and clinical evaluation for the presence of infection, psychosocial disturbances, thromboembolism, peptic ulcers, cataracts, and osteoporosis. Pediatric patients who are treated with corticosteroids by any route, including systemically administered corticosteroids, may experience a decrease in their growth velocity. This negative impact of corticosteroids on growth has been observed at low systemic doses and in the absence of laboratory evidence of HPA axis suppression (i.e., cosyntropin stimulation and basal cortisol plasma levels). Growth velocity may therefore be a more sensitive indicator of systemic corticosteroid exposure in pediatric patients than some commonly used tests of HPA axis function. The linear growth of pediatric patients treated with corticosteroids should be monitored, and the potential growth effects of prolonged treatment should be weighed against clinical benefits obtained and the availability of treatment alternatives. In order to minimize the potential growth effects of corticosteroids, pediatric patients should be titrated to the lowest effective dose.
Geriatic Use
Clinical studies did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Gender
There is no FDA guidance on the use of Prednisolone (injection) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Prednisolone (injection) with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Prednisolone (injection) in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Prednisolone (injection) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Prednisolone (injection) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Prednisolone (injection) in patients who are immunocompromised.
Administration and Monitoring
Administration
- Intramuscular
- Intravenous
- NOT FOR USE IN NEONATES. CONTAINS BENZYL ALCOHOL.
Monitoring
There is limited information regarding Prednisolone (injection) Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Prednisolone (injection) and IV administrations.
Overdosage
Treatment of acute overdosage is by supportive and symptomatic therapy. For chronic overdosage in the face of severe disease requiring continuous steroid therapy, the dosage of the corticosteroid may be reduced only temporarily, or alternate day treatment may be introduced.
Pharmacology
Mechanism of Action
There is limited information regarding Prednisolone (injection) Mechanism of Action in the drug label.
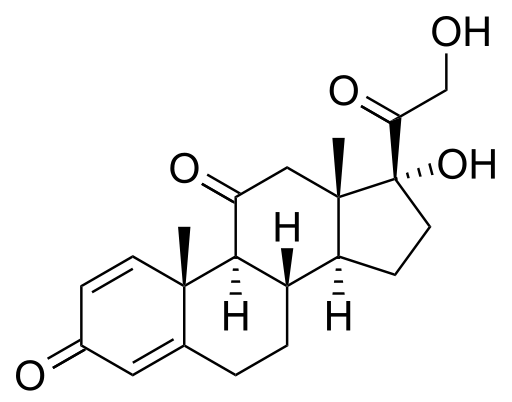
Structure
- A-METHAPRED™ Sterile Powder is an anti-inflammatory glucocorticoid, which contains methylprednisolone sodium succinate as the active ingredient. A-METHAPRED™ is available in several strengths and packages for intravenous or intramuscular administration.
- 40 mg Single-Dose Vial – Each mL (when mixed) contains methylprednisolone sodium succinate equivalent to 40 mg methylprednisolone; also 1.6 mg monobasic sodium phosphate anhydrous; 17.46 mg dibasic sodium phosphate anhydrous; 25 mg lactose anhydrous; 8.8 mg benzyl alcohol added as preservative.
- 125 mg Single-Dose Vial – Each 2 mL (when mixed) contains methylprednisolone sodium succinate equivalent to 125 mg methylprednisolone; also 1.6 mg monobasic sodium phosphate anhydrous; 17.4 mg dibasic sodium phosphate anhydrous; 17.6 mg benzyl alcohol added as preservative.
- When necessary, the pH of each formula was adjusted with sodium hydroxide so that the pH of the reconstituted solution is within the USP specified range of 7 to 8 and the tonicities are, for the 40 mg per mL solution, 0.50 osmolar; for the 125 mg per 2 mL, 0.40 osmolar; (Isotonic saline = 0.28 osmolar).
- The chemical name for methylprednisolone sodium succinate is pregna-1,4-diene-3,20-dione,21-(3-carboxy-1-oxo-propoxy)-11,17-dihydroxy-6-methyl-monosodium salt, (6α, 11β), and the molecular weight is 496.53.
The structural formula is represented below:

- A-METHAPRED™ (methylprednisolone sodium succinate for injection, USP) sterile powder contains methylprednisolone sodium succinate as the active ingredient. Methylprednisolone sodium succinate, USP, is the sodium succinate ester of methylprednisolone. Methylprednisolone sodium succinate, USP, occurs as a white, or nearly white, odorless hygroscopic, amorphous solid. It is very soluble in water and in alcohol; it is insoluble in chloroform and is very slightly soluble in acetone.
- Methylprednisolone sodium succinate is so extremely soluble in water that it may be administered in a small volume of diluent and is especially well suited for intravenous use in situations in which high blood levels of methylprednisolone are required rapidly.
- IMPORTANT – Use only Bacteriostatic Water For Injection with Benzyl Alcohol when reconstituting A-METHAPRED™.
- Use within 48 hours after mixing.
Pharmacodynamics
There is limited information regarding Prednisolone (injection) Pharmacodynamics in the drug label.
Pharmacokinetics
There is limited information regarding Prednisolone (injection) Pharmacokinetics in the drug label.
Nonclinical Toxicology
There is limited information regarding Prednisolone (injection) Nonclinical Toxicology in the drug label.
Clinical Studies
There is limited information regarding Prednisolone (injection) Clinical Studies in the drug label.
How Supplied
A-METHAPRED™ sterile powder is available in the following packages:

Storage
- Protect from light.
- Store unreconstituted product at 20 to 25°C (68 to 77°F). [See USP Controlled Room Temperature.]
- Store solution at 20 to 25°C (68 to 77°F). [See USP Controlled Room Temperature.]
- Use solution within 48 hours after mixing.
Images
Drug Images
{{#ask: Page Name::Prednisolone (injection) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Prednisolone (injection) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Prednisolone (injection) Patient Counseling Information in the drug label.
Precautions with Alcohol
Alcohol-Prednisolone interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Prednisolone (injection) Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Prednisolone (injection) Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Prednisolone (injection) |Label Name=A-METHAPRED ingredients and appearance.png
}}