Porphyria pathophysiology
|
Porphyria Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Porphyria pathophysiology On the Web |
|
American Roentgen Ray Society Images of Porphyria pathophysiology |
|
Risk calculators and risk factors for Porphyria pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief:
Please help WikiDoc by adding content here. It's easy! Click here to learn about editing.
Overview
Pathophysiology
In humans, porphyrins are the main precursors of heme, an essential constituent of hemoglobin, myoglobin, catalase, peroxidase, respiratory and P450 liver cytochromes.
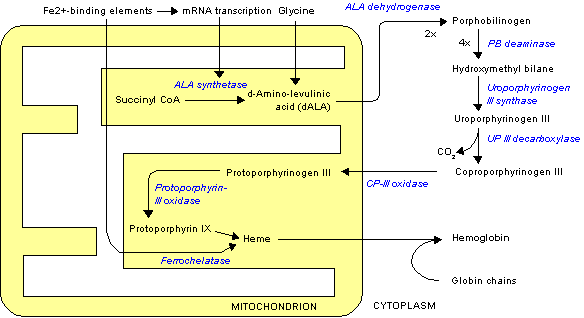
Deficiency in the enzymes of the porphyrin pathway leads to insufficient production of heme. Heme function plays a central role in cellular metabolism. This is not the main problem in the porphyrias; most heme synthesis enzymes—even dysfunctional enzymes—have enough residual activity to assist in heme biosynthesis. The principal problem in these deficiencies is the accumulation of porphyrins, the heme precursors, which are toxic to tissue in high concentrations. The chemical properties of these intermediates determine the location of accumulation, whether they induce photosensitivity, and whether the intermediate is excreted (in the urine or feces).
There are eight enzymes in the heme biosynthetic pathway, four of which—the first one and the last three—are in the mitochondria, while the other four are in the cytosol. Defects in any of these can lead to some form of porphyria.
The hepatic porphyrias are characterized by acute neurological attacks (seizures, psychosis, extreme back and abdominal pain and an acute polyneuropathy), while the erythropoietic forms present with skin problems, usually a light-sensitive blistering rash and increased hair growth.
Variegate porphyria (also porphyria variegata or mixed porphyria), which results from a partial deficiency in PROTO oxidase, manifests itself with skin lesions similar to those of porphyria cutanea tarda combined with acute neurologic attacks. All other porphyrias are either skin- or nerve-predominant.
Genetics
Evaluation of family members is necessary to identify latent porphyria. All acute porphyrias are autosomal dominant except for ALA-D which is autosomal recessive.