Naltrexone (injection)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Turky Alkathery, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Naltrexone (injection) is an opioid antagonist that is FDA approved for the treatment of alcohol dependence in patients who are able to abstain from alcohol in an outpatient setting prior to initiation of treatment with Naltrexone (injection). Common adverse reactions include nausea, vomiting, injection site reactions (including induration, pruritus, nodules and swelling), muscle cramps, dizziness or syncope, somnolence or sedation, anorexia, decreased appetite or other appetite disorders.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
- Treatment with Naltrexone (injection) should be part of a comprehensive management program that includes psychosocial support.
Alcohol Dependence
- Naltrexone (injection) is indicated for the treatment of alcohol dependence in patients who are able to abstain from alcohol in an outpatient setting prior to initiation of treatment with Naltrexone (injection). Patients should not be actively drinking at the time of initial Naltrexone (injection) administration.
Opioid Dependence
- Naltrexone (injection) is indicated for the prevention of relapse to opioid dependence, following opioid detoxification.
Dosage
- Naltrexone (injection) must be prepared and administered by a healthcare provider.
- Prior to initiating Naltrexone (injection), an opioid-free duration of a minimum of 7-10 days is recommended for patients, to avoid precipitation of opioid withdrawal that may be severe enough to require hospitalization.
- The recommended dose of Naltrexone (injection) is 380 mg delivered intramuscularly every 4 weeks or once a month. The injection should be administered by a healthcare provider as an intramuscular (IM) gluteal injection, alternating buttocks for each subsequent injection, using the carton components provided. The needles provided in the carton are customized needles. Naltrexone (injection) must not be injected using any other needle. The needle lengths (either 1.5 or 2 inches) may not be adequate in every patient because of body habitus. Body habitus should be assessed prior to each injection for each patient to assure that needle length is adequate for intramuscular administration. For patients with a larger amount of subcutaneous tissue overlying the gluteal muscle, the administering healthcare provider may utilize the supplied 2-inch needle with needle protection device to help ensure that the injectate reaches the intramuscular mass. For very lean patients, the 1.5-inch needle may be appropriate to prevent the needle contacting the periosteum. Either needle may be used for patients with average body habitus. Healthcare providers should ensure that the Naltrexone (injection) injection is given correctly, and should consider alternate treatment for those patients whose body habitus precludes an intramuscular gluteal injection with one of the provided needles.
- Naltrexone (injection) must not be administered intravenously or subcutaneously.
- If a patient misses a dose, he/she should be instructed to receive the next dose as soon as possible.
- Pretreatment with oral naltrexone is not required before using Naltrexone (injection).
Reinitiation of Treatment in Patients Previously Discontinued
- There are no data to specifically address reinitiation of treatment. Patients reinitiating treatment with Naltrexone (injection) should be opioid-free at the time of dose administration.
Switching From Oral Naltrexone
- There are no systematically collected data that specifically address the switch from oral naltrexone to Naltrexone (injection).
Switching from Buprenorphine, Buprenorphine/Naloxone, or Methadone
- There are no systematically collected data that specifically address the switch from buprenorphine or methadone to Naltrexone (injection); however, review of postmarketing case reports have indicated that some patients may experience severe manifestations of precipitated withdrawal when being switched from opioid agonist therapy to opioid antagonist therapy. Patients transitioning from buprenorphine or methadone may be vulnerable to precipitation of withdrawal symptoms for as long as 2 weeks. Healthcare providers should be prepared to manage withdrawal symptomatically with non-opioid medications.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
- There is limited information regarding Off-Label Guideline-Supported Use of Naltrexone (injection) in adult patients.
Non–Guideline-Supported Use
- There is limited information regarding Off-Label Non–Guideline-Supported Use of Naltrexone (injection) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
- The safety and efficacy of Naltrexone (injection) have not been established in the pediatric population.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
- There is limited information regarding Off-Label Guideline-Supported Use of Naltrexone (injection) in pediatric patients.
Non–Guideline-Supported Use
- There is limited information regarding Off-Label Non–Guideline-Supported Use of Naltrexone (injection) in pediatric patients.
Contraindications
- Naltrexone (injection) is contraindicated in:
- Patients receiving opioid analgesics.
- Patients with current physiologic opioid dependence.
- Patients in acute opioid withdrawal.
- Any individual who has failed the naloxone challenge test or has a positive urine screen for opioids.
- Patients who have previously exhibited hypersensitivity to naltrexone, PLG, carboxymethylcellulose, or any other components of the diluent.
Warnings
Vulnerability to Opioid Overdose
- After opioid detoxification, patients are likely to have reduced tolerance to opioids. Naltrexone (injection) blocks the effects of exogenous opioids for approximately 28 days after administration. However, as the blockade wanes and eventually dissipates completely, patients who have been treated with Naltrexone (injection) may respond to lower doses of opioids than previously used, just as they would have shortly after completing detoxification. This could result in potentially life-threatening opioid intoxication (respiratory compromise or arrest, circulatory collapse, etc.) if the patient uses previously tolerated doses of opioids. Cases of opioid overdose with fatal outcomes have been reported in patients who used opioids at the end of a dosing interval, after missing a scheduled dose, or after discontinuing treatment.
- Patients should be alerted that they may be more sensitive to opioids, even at lower doses, after Naltrexone (injection) treatment is discontinued, especially at the end of a dosing interval (i.e., near the end of the month that Naltrexone (injection) was administered), or after a dose of Naltrexone (injection) is missed. It is important that patients inform family members and the people closest to the patient of this increased sensitivity to opioids and the risk of overdose.
- There is also the possibility that a patient who is treated with Naltrexone (injection) could overcome the opioid blockade effect of Naltrexone (injection). Although Naltrexone (injection) is a potent antagonist with a prolonged pharmacological effect, the blockade produced by Naltrexone (injection) is surmountable. The plasma concentration of exogenous opioids attained immediately following their acute administration may be sufficient to overcome the competitive receptor blockade. This poses a potential risk to individuals who attempt, on their own, to overcome the blockade by administering large amounts of exogenous opioids. Any attempt by a patient to overcome the antagonism by taking opioids is especially dangerous and may lead to life-threatening opioid intoxication or fatal overdose. Patients should be told of the serious consequences of trying to overcome the opioid blockade.
Injection Site Reactions
- Naltrexone (injection) injections may be followed by pain, tenderness, induration, swelling, erythema, bruising, or pruritus; however, in some cases injection site reactions may be very severe. In the clinical trials, one patient developed an area of induration that continued to enlarge after 4 weeks, with subsequent development of necrotic tissue that required surgical excision. In the postmarketing period, additional cases of injection site reaction with features including induration, cellulitis, hematoma, abscess, sterile abscess, and necrosis, have been reported. Some cases required surgical intervention, including debridement of necrotic tissue. Some cases resulted in significant scarring. The reported cases occurred primarily in female patients.
- Naltrexone (injection) is administered as an intramuscular gluteal injection, and inadvertent subcutaneous injection of Naltrexone (injection) may increase the likelihood of severe injection site reactions. The needles provided in the carton are customized needles. Naltrexone (injection) must not be injected using any other needle. The needle lengths (either 1.5 inches or 2 inches) may not be adequate in every patient because of body habitus. Body habitus should be assessed prior to each injection for each patient to assure that the proper needle is selected and that the needle length is adequate for intramuscular administration. For patients with a larger amount of subcutaneous tissue overlying the gluteal muscle, the administering healthcare provider may utilize the supplied 2-inch needle with needle protection device to help ensure that the injectate reaches the intramuscular mass. For very lean patients, the 1.5-inch needle may be appropriate to prevent the needle contacting the periosteum. Either needle may be used for patients with average body habitus. Healthcare providers should ensure that the Naltrexone (injection) is given correctly, and should consider alternate treatment for those patients whose body habitus precludes an intramuscular gluteal injection with one of the provided needles.
- Patients should be informed that any concerning injection site reactions should be brought to the attention of the healthcare provider. Patients exhibiting signs of abscess, cellulitis, necrosis, or extensive swelling should be evaluated by a physician to determine if referral to a surgeon is warranted.
Precipitation of Opioid Withdrawal
- The symptoms of spontaneous opioid withdrawal (which are associated with the discontinuation of opioid in a dependent individual) are uncomfortable, but they are not generally believed to be severe or necessitate hospitalization. However, when withdrawal is precipitated abruptly by the administration of an opioid antagonist to an opioid-dependent patient, the resulting withdrawal syndrome can be severe enough to require hospitalization. Review of postmarketing cases of precipitated opioid withdrawal in association with naltrexone treatment has identified cases with symptoms of withdrawal severe enough to require hospital admission, and in some cases, management in the intensive care unit.
- To prevent occurrence of precipitated withdrawal in patients dependent on opioids, or exacerbation of a pre-existing subclinical withdrawal syndrome, opioid-dependent patients, including those being treated for alcohol dependence, should be opioid-free (including tramadol) before starting Naltrexone (injection) treatment. An opioid-free interval of a minimum of 7-10 days is recommended for patients previously dependent on short-acting opioids. Patients transitioning from buprenorphine or methadone may be vulnerable to precipitation of withdrawal symptoms for as long as two weeks.
- If a more rapid transition from agonist to antagonist therapy is deemed necessary and appropriate by the healthcare provider, monitor the patient closely in an appropriate medical setting where precipitated withdrawal can be managed.
- In every case, healthcare providers should always be prepared to manage withdrawal symptomatically with non-opioid medications because there is no completely reliable method for determining whether a patient has had an adequate opioid-free period. A naloxone challenge test may be helpful; however, a few case reports have indicated that patients may experience precipitated withdrawal despite having a negative urine toxicology screen or tolerating a naloxone challenge test (usually in the setting of transitioning from buprenorphine treatment). Patients should be made aware of the risks associated with precipitated withdrawal and encouraged to give an accurate account of last opioid use. Patients treated for alcohol dependence with Naltrexone (injection) should also be assessed for underlying opioid dependence and for any recent use of opioids prior to initiation of treatment with Naltrexone (injection). Precipitated opioid withdrawal has been observed in alcohol-dependent patients in circumstances where the prescriber had been unaware of the additional use of opioids or co-dependence on opioids.
Hepatotoxicity
- Cases of hepatitis and clinically significant liver dysfunction were observed in association with Naltrexone (injection) exposure during the clinical development program and in the postmarketing period. Transient, asymptomatic hepatic transaminase elevations were also observed in the clinical trials and postmarketing period. Although patients with clinically significant liver disease were not systematically studied, clinical trials did include patients with asymptomatic viral hepatitis infections. When patients presented with elevated transaminases, there were often other potential causative or contributory etiologies identified, including pre-existing alcoholic liver disease, hepatitis B and/or C infection, and concomitant usage of other potentially hepatotoxic drugs. Although clinically significant liver dysfunction is not typically recognized as a manifestation of opioid withdrawal, opioid withdrawal that is precipitated abruptly may lead to systemic sequelae including acute liver injury.
- Patients should be warned of the risk of hepatic injury and advised to seek medical attention if they experience symptoms of acute hepatitis. Use of Naltrexone (injection) should be discontinued in the event of symptoms and/or signs of acute hepatitis.
Depression and Suicidality
- Alcohol- and opioid-dependent patients, including those taking Naltrexone (injection), should be monitored for the development of depression or suicidal thinking. Families and caregivers of patients being treated with Naltrexone (injection) should be alerted to the need to monitor patients for the emergence of symptoms of depression or suicidality, and to report such symptoms to the patient's healthcare provider.
Alcohol Dependence
- In controlled clinical trials of Naltrexone (injection) administered to adults with alcohol dependence, adverse events of a suicidal nature (suicidal ideation, suicide attempts, completed suicides) were infrequent overall, but were more common in patients treated with Naltrexone (injection) than in patients treated with placebo (1% vs 0). In some cases, the suicidal thoughts or behavior occurred after study discontinuation, but were in the context of an episode of depression that began while the patient was on study drug. Two completed suicides occurred, both involving patients treated with Naltrexone (injection).
- Depression-related events associated with premature discontinuation of study drug were also more common in patients treated with Naltrexone (injection) (~1%) than in placebo-treated patients (0).
- In the 24-week, placebo-controlled pivotal trial in 624 alcohol-dependent patients, adverse events involving depressed mood were reported by 10% of patients treated with Naltrexone (injection) 380 mg, as compared to 5% of patients treated with placebo injections.
Opioid Dependence
- In an open-label, long-term safety study conducted in the US, adverse events of a suicidal nature (depressed mood, suicidal ideation, suicide attempt) were reported by 5% of opioid-dependent patients treated with Naltrexone (injection) 380 mg (n=101) and 10% of opioid-dependent patients treated with oral naltrexone (n=20). In the 24-week, placebo-controlled pivotal trial that was conducted in Russia in 250 opioid-dependent patients, adverse events involving depressed mood or suicidal thinking were not reported by any patient in either treatment group (Naltrexone (injection) 380 mg or placebo).
When Reversal of Naltrexone (injection) Blockade Is Required for Pain Management
- In an emergency situation in patients receiving Naltrexone (injection), suggestions for pain management include regional analgesia or use of non-opioid analgesics. If opioid therapy is required as part of anesthesia or analgesia, patients should be continuously monitored in an anesthesia care setting by persons not involved in the conduct of the surgical or diagnostic procedure. The opioid therapy must be provided by individuals specifically trained in the use of anesthetic drugs and the management of the respiratory effects of potent opioids, specifically the establishment and maintenance of a patent airway and assisted ventilation.
- Irrespective of the drug chosen to reverse Naltrexone (injection) blockade, the patient should be monitored closely by appropriately trained personnel in a setting equipped and staffed for cardiopulmonary resuscitation.
Eosinophilic Pneumonia
- In clinical trials with Naltrexone (injection), there was one diagnosed case and one suspected case of eosinophilic pneumonia. Both cases required hospitalization, and resolved after treatment with antibiotics and corticosteroids. Similar cases have been reported in postmarketing use. Should a person receiving Naltrexone (injection) develop progressive dyspnea and hypoxemia, the diagnosis of eosinophilic pneumonia should be considered. Patients should be warned of the risk of eosinophilic pneumonia, and advised to seek medical attention should they develop symptoms of pneumonia. Clinicians should consider the possibility of eosinophilic pneumonia in patients who do not respond to antibiotics.
Hypersensitivity Reactions Including Anaphylaxis
- Cases of urticaria, angioedema, and anaphylaxis have been observed with use of Naltrexone (injection) in the clinical trial setting and in postmarketing use. Patients should be warned of the risk of hypersensitivity reactions, including anaphylaxis. In the event of a hypersensitivity reaction, patients should be advised to seek immediate medical attention in a healthcare setting prepared to treat anaphylaxis. The patient should not receive any further treatment with Naltrexone (injection).
Intramuscular Injections
- As with any intramuscular injection, Naltrexone (injection) should be administered with caution to patients with thrombocytopenia or any coagulation disorder (eg, hemophilia and severe hepatic failure).
Alcohol Withdrawal
- Use of Naltrexone (injection) does not eliminate nor diminish alcohol withdrawal symptoms.
Interference with Laboratory Tests
- Naltrexone (injection) may be cross-reactive with certain immunoassay methods for the detection of drugs of abuse (specifically opioids) in urine. For further information, reference to the specific immunoassay instructions is recommended.
Adverse Reactions
Clinical Trials Experience
- Serious adverse reactions that may be associated with Naltrexone (injection) therapy in clinical use include: severe injection site reactions, eosinophilic pneumonia, serious allergic reactions, unintended precipitation of opioid withdrawal, accidental opioid overdose and depression and suicidality.
- The adverse events seen most frequently in association with Naltrexone (injection) therapy for alcohol dependence (ie, those occurring in ≥ 5% and at least twice as frequently with Naltrexone (injection) than placebo) include nausea, vomiting, injection site reactions (including induration, pruritus, nodules and swelling), muscle cramps, dizziness or syncope, somnolence or sedation, anorexia, decreased appetite or other appetite disorders.
- The adverse events seen most frequently in association with Naltrexone (injection) therapy in opioid-dependent patients (ie, those occurring in ≥ 2% and at least twice as frequently with Naltrexone (injection) than placebo) were hepatic enzyme abnormalities, injection site pain, nasopharyngitis, insomnia, and toothache.
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- In all controlled and uncontrolled trials during the premarketing development of Naltrexone (injection), more than 1100 patients with alcohol and/or opioid dependence have been treated with Naltrexone (injection). Approximately 700 patients have been treated for 6 months or more, and more than 400 for 1 year or longer.
Adverse Events Leading to Discontinuation of Treatment
- Alcohol Dependence
- In controlled trials of 6 months or less in alcohol-dependent patients, 9% of alcohol-dependent patients treated with Naltrexone (injection) discontinued treatment due to an adverse event, as compared to 7% of the alcohol-dependent patients treated with placebo. Adverse events in the Naltrexone (injection) 380-mg group that led to more dropouts than in the placebo-treated group were injection site reactions (3%), nausea (2%), pregnancy (1%), headache (1%), and suicide-related events (0.3%). In the placebo group, 1% of patients withdrew due to injection site reactions, and 0% of patients withdrew due to the other adverse events.
- Opioid Dependence
- In a controlled trial of 6 months, 2% of opioid-dependent patients treated with Naltrexone (injection) discontinued treatment due to an adverse event, as compared to 2% of the opioid-dependent patients treated with placebo.
Common Adverse Reactions
- TABLE 1 lists all treatment-emergent clinical adverse reactions, regardless of causality, occurring in ≥5% of patients with alcohol dependence, for which the incidence was greater in the combined Naltrexone (injection) group than in the placebo group. A majority of patients treated with Naltrexone (injection) in clinical studies had adverse reactions with a maximum intensity of “mild” or “moderate”.

- Opioid Dependence
- In the open-label, long-term safety study conducted in the US, the commonly reported adverse reactions among the opioid-dependent patients in the study were similar to those commonly observed events in the alcohol-dependent populations in Naltrexone (injection) clinical trials as displayed in TABLE 1, above. For example, injection site reactions of all types, nausea and diarrhea occurred in more than 5% of patients on Naltrexone (injection) in the open-label study. In contrast, 48% percent, of the opioid-dependent patients had at least one adverse event in the “Infections and Infestations” Body System. Adverse Reactions/Preferred Terms of nasopharyngitis, upper respiratory tract infection, urinary tract infection, and sinusitis were most commonly reported.
- In the placebo-controlled study in opioid-dependent patients conducted in Russia, the overall frequency of adverse events was lower than in the U.S. population described above. TABLE 2 lists treatment-emergent clinical adverse events, regardless of causality, occurring in ≥2% of patients with opioid dependence, for which the incidence was greater in the Naltrexone (injection) group than in the placebo group. All adverse events were assessed as having a maximum intensity of “mild” or “moderate.”

- Laboratory Tests
- Eosinophil Count:
- In clinical trials, subjects on Naltrexone (injection) had increases in eosinophil counts relative to subjects on placebo. With continued use of Naltrexone (injection), eosinophil counts returned to normal over a period of several months.
- Platelet Count:
- Naltrexone (injection) 380 mg was associated with a decrease in platelet count. In clinical trials, alcohol-dependent patients treated with Naltrexone (injection) experienced a mean maximal decrease in platelet count of 17.8 x 103/μL, compared to 2.6 x 103/μL in placebo patients.
- After 24 weeks of treatment, opioid-dependent patients treated with Naltrexone (injection) experienced a mean maximal decrease in platelet count of 62.8 x 103/μL, compared to 39.9 x 103/μL in placebo patients. In randomized controlled trials, Naltrexone (injection) was not associated with an increase in bleeding-related adverse events.
- Hepatic Enzyme Elevations:
- In short-term, controlled trials, in alcohol-dependent patients, the incidence of AST elevations associated with Naltrexone (injection) treatment was similar to that observed with oral naltrexone treatment (1.5% each) and slightly higher than observed with placebo treatment (0.9%).
- In the 6-month controlled trial conducted in opioid-dependent subjects, 89% had a baseline diagnosis of hepatitis C infection, and 41% had a baseline diagnosis of HIV infection. There were frequently observed elevated liver enzyme levels (ALT, AST, and GGT); these were more commonly reported as adverse events in the Naltrexone (injection) 380-mg group than in the placebo group. Patients could not enroll in this trial if they had a baseline ALT or AST value that was more than three times the upper limit of normal. More patients treated with Naltrexone (injection) in this study experienced treatment-emergent elevations in transaminases to more than three times the upper limit of normal than patients treated with placebo. Shifts to more than three times the upper limit of normal occurred in 20% of patients treated with Naltrexone (injection) as compared with 13% of placebo patients. Shifts in values of AST to more than three times the upper limit were also more common in the Naltrexone (injection) (14%) arm compared with the placebo (11%) arm. Opioid-dependent patients treated with Naltrexone (injection) experienced a mean maximal increase from baseline ALT levels of 61 IU/L compared with 48 IU/L in placebo patients. Similarly for AST, opioid-dependent patients treated with Naltrexone (injection) experienced a mean maximal increase from baseline AST levels of 40 IU/L compared with 31 IU/L in placebo patients.
- Creatinine Phosphokinase:
- In short-term controlled trials in alcohol-dependent patients, more patients treated with Naltrexone (injection) 380 mg (11%) and oral naltrexone (17%) shifted from normal creatinine phosphokinase (CPK) levels before treatment to abnormal CPK levels at the end of the trials, compared to placebo patients (8%). In open-label trials, 16% of patients dosed for more than 6 months had increases in CPK. For both the oral naltrexone and Naltrexone (injection) 380-mg groups, CPK abnormalities were most frequently in the range of 1–2 x ULN. However, there were reports of CPK abnormalities as high as 4x ULN for the oral naltrexone group, and 35 x ULN for the Naltrexone (injection) 380-mg group. Overall, there were no differences between the placebo and naltrexone (oral or injectable) groups with respect to the proportions of patients with a CPK value at least three times the upper limit of normal. No factors other than naltrexone exposure were associated with the CPK elevations.
- More opioid-dependent patients treated with Naltrexone (injection) 380-mg (39%) shifted from normal creatinine phosphokinase (CPK) levels before treatment to abnormal CPK levels during the study as compared to patients treated with placebo (32%). There were reports of CPK abnormalities as high as 41.8 x ULN for the placebo group, and 22.1 x ULN for the Naltrexone (injection) 380-mg group.
Other Events Observed During the Naltrexone (injection) Clinical Studies
- The following is a list of treatment-emergent adverse reactions reported by alcohol- and/or opioid-dependent subjects treated with Naltrexone (injection) in all clinical trials. The listing does not include those events already listed in the previous tables or elsewhere in labeling, those events for which a drug cause was remote, those events that were so general as to be uninformative, and those events reported only once that did not have a substantial probability of being acutely life-threatening.
- Blood and Lymphatic System Disorders – lymphadenopathy (including cervical adenitis), white blood cell count increased
- Cardiac Disorders – angina pectoris, angina unstable, atrial fibrillation, cardiac failure congestive, coronary artery atherosclerosis, myocardial infarction, palpitations
- Eye Disorders – conjunctivitis, vision blurred
- Gastrointestinal Disorders – abdominal discomfort, colitis, constipation, flatulence, gastroesophageal reflux disease, gastrointestinal hemorrhage, hemorrhoids, pancreatitis acute, paralytic ileus, perirectal abscess
- General Disorders and Administration Site Conditions – chest pain, chest tightness, chills, face edema, irritability, lethargy, pyrexia, rigors
- Hepatobiliary Disorders – cholecystitis acute, cholelithiasis
- Immune System Disorders – seasonal allergy, hypersensitivity reaction (including angioneurotic edema and urticaria)
- Infections and Infestations – bronchitis, gastroenteritis, laryngitis, pneumonia, sinusitis, tooth abscess, upper respiratory tract infection, urinary tract infection, advanced HIV disease in HIV-infected patients
- Investigations – weight decreased, weight increased
- Metabolism and Nutrition Disorders – appetite increased, dehydration, heat exhaustion, hypercholesterolemia
- Musculoskeletal and Connective Tissue Disorders –joint stiffness, muscle spasms, myalgia, pain in limb
- Nervous System Disorders – cerebral arterial aneurysm, convulsions, disturbance in attention, dysgeusia, mental impairment, migraine, ischemic stroke, paresthesia
- Pregnancy, Puerperium, and Perinatal Conditions – abortion missed
- Psychiatric Disorders – abnormal dreams, agitation, alcohol withdrawal syndrome, euphoric mood, delirium, libido decreased
- Respiratory, Thoracic, and Mediastinal Disorders – chronic obstructive pulmonary disease, dyspnea, pharyngolaryngeal pain, sinus congestion
- Skin and Subcutaneous Tissue Disorders –night sweats, pruritus, sweating increased
- Vascular Disorders –deep venous thrombosis, hot flushes, pulmonary embolism
Postmarketing Experience
Hypersensitivity Reactions including Anaphylaxis
- Hypersensitivity reactions including anaphylaxis have been reported during postmarketing surveillance.
Reports From Other Intramuscular Drug Products Containing Polylactide-co-glycolide (PLG) Microspheres
- Retinal Artery Occlusion
- Retinal artery occlusion after injection with another drug product containing polylactide-co-glycolide (PLG) microspheres has been reported very rarely during postmarketing surveillance. This event has been reported in the presence of abnormal arteriovenous anastomosis. No cases of retinal artery occlusion have been reported during Naltrexone (injection) clinical trials or postmarketing surveillance. Naltrexone (injection) should be administered by intramuscular (IM) injection into the gluteal muscle, and care must be taken to avoid inadvertent injection into a blood vessel.
Drug Interactions
- Patients taking Naltrexone (injection) may not benefit from opioid-containing medicines. Naltrexone antagonizes the effects of opioid-containing medicines, such as cough and cold remedies, antidiarrheal preparations and opioid analgesics.
Use in Specific Populations
Pregnancy
- There are no adequate and well-controlled studies of either naltrexone or Naltrexone (injection) in pregnant women. Naltrexone (injection) should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Reproduction and developmental studies have not been conducted for Naltrexone (injection). Studies with naltrexone administered via the oral route have been conducted in pregnant rats and rabbits.
- Teratogenic Effects: Naltrexone has been shown to increase the incidence of early fetal loss when given to rats at doses ≥30 mg/kg/day (11 times the human exposure based on an AUC(0-28d) comparison) and to rabbits at oral doses ≥60 mg/kg/day (2 times the human exposure based on an AUC(0-28d) comparison).
- There was no evidence of teratogenicity when naltrexone was administered orally to rats and rabbits during the period of major organogenesis at doses up to 200 mg/kg/day (175- and 14-times the human exposure based on an AUC(0-28d) comparison, respectively).
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Naltrexone (injection) in women who are pregnant.
Labor and Delivery
- The potential effect of Naltrexone (injection) on duration of labor and delivery in humans is unknown.
Nursing Mothers
- Transfer of naltrexone and 6β-naltrexol into human milk has been reported with oral naltrexone. Because of the potential for tumorigenicity shown for naltrexone in animal studies, and because of the potential for serious adverse reactions in nursing infants from Naltrexone (injection), a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
- The safety and efficacy of Naltrexone (injection) have not been established in the pediatric population. The pharmacokinetics of Naltrexone (injection) have not been evaluated in a pediatric population.
Geriatic Use
- In trials of alcohol-dependent subjects, 2.6% (n=26) of subjects were >65 years of age, and one patient was >75 years of age. Clinical studies of Naltrexone (injection) did not include sufficient numbers of subjects age 65 and over to determine whether they respond differently from younger subjects. No subjects over age 65 were included in studies of opioid-dependent subjects. The pharmacokinetics of Naltrexone (injection) have not been evaluated in the geriatric population.
Gender
There is no FDA guidance on the use of Naltrexone (injection) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Naltrexone (injection) with respect to specific racial populations.
Renal Impairment
- Pharmacokinetics of Naltrexone (injection) are not altered in subjects with mild renal insufficiency (creatinine clearance of 50-80 mL/min). Dose adjustment is not required in patients with mild renal impairment. Naltrexone (injection) pharmacokinetics have not been evaluated in subjects with moderate and severe renal insufficiency. Because naltrexone and its primary metabolite are excreted primarily in the urine, caution is recommended in administering Naltrexone (injection) to patients with moderate to severe renal impairment.
Hepatic Impairment
- The pharmacokinetics of Naltrexone (injection) are not altered in subjects with mild to moderate hepatic impairment (Groups A and B of the Child-Pugh classification). Dose adjustment is not required in subjects with mild or moderate hepatic impairment. Naltrexone (injection) pharmacokinetics were not evaluated in subjects with severe hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Naltrexone (injection) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Naltrexone (injection) in patients who are immunocompromised.
Administration and Monitoring
Administration
- Intramuscular
Directions for Use

Monitoring
- Monitor patients for the development of depression or suicidal thinking
- If opioid therapy is required as part of anesthesia or analgesia, patients should be continuously monitored in an anesthesia care setting by persons not involved in the conduct of the surgical or diagnostic procedure.
IV Compatibility
There is limited information regarding the compatibility of Naltrexone (injection) and IV administrations.
Overdosage
- There is limited experience with overdose of VIVITROL. Single doses up to 784 mg were administered to 5 healthy subjects. There were no serious or severe adverse events. The most common effects were injection site reactions, nausea, abdominal pain, somnolence, and dizziness. There were no significant increases in hepatic enzymes.
In the event of an overdose, appropriate supportive treatment should be initiated.
Pharmacology
Mechanism of Action
- Naltrexone is an opioid antagonist with highest affinity for the mu opioid receptor. Naltrexone has little or no opioid agonist activity.
- Naltrexone has few, if any, intrinsic actions besides its opioid blocking properties. However, it does produce some pupillary constriction, by an unknown mechanism.
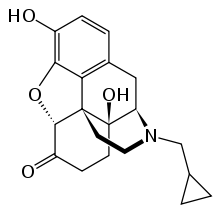
Structure
- VIVITROL® (naltrexone for extended-release injectable suspension) is supplied as a microsphere formulation of naltrexone for suspension, to be administered by intramuscular injection. Naltrexone is an opioid antagonist with little, if any, opioid agonist activity.
- Naltrexone is designated chemically as morphinan-6-one, 17 (cyclopropylmethyl) 4,5-epoxy-3,14-dihydroxy-(5α) (CAS Registry # 16590-41-3). The molecular formula is C20H23NO4 and its molecular weight is 341.41 in the anhydrous form (ie, < 1% maximum water content). The structural formula is:

- Naltrexone base anhydrous is an off-white to a light tan powder with a melting point of 168-170ºC (334-338ºF). It is insoluble in water and is soluble in ethanol.
- Naltrexone (injection) is provided as a carton containing a vial each of Naltrexone (injection) microspheres and diluent, one 5-mL syringe, one 1-inch 20-gauge preparation needle, two 1.5-inch 20-gauge and two 2-inch 20-gauge administration needles with needle protection device.
- Naltrexone (injection) microspheres consist of a sterile, off-white to light tan powder that is available in a dosage strength of 380 mg of naltrexone per vial. Naltrexone is incorporated in 75:25 polylactide-co-glycolide (PLG) at a concentration of 337 mg of naltrexone per gram of microspheres.
- The diluent is a clear, colorless solution. The composition of the diluent includes carboxymethylcellulose sodium salt, polysorbate 20, sodium chloride, and water for injection. The microspheres must be suspended in the diluent prior to injection.
Pharmacodynamics
- The administration of Naltrexone (injection) is not associated with the development of tolerance or dependence. In subjects physically dependent on opioids, Naltrexone (injection) will precipitate withdrawal symptomatology.
- Occupation of opioid receptors by naltrexone may block the effects of endogenous opioid peptides. It markedly attenuates or completely blocks, reversibly, the subjective effects of exogenous opioids. The neurobiological mechanisms responsible for the reduction in alcohol consumption observed in alcohol-dependent patients treated with naltrexone are not entirely understood. However, involvement of the endogenous opioid system is suggested by preclinical data.
- Naltrexone blocks the effects of opioids by competitive binding at opioid receptors. This makes the blockade produced potentially surmountable, but overcoming full naltrexone blockade by administration of opioids may result in non-opioid receptor-mediated symptoms such as histamine release.
- Naltrexone (injection) is not aversive therapy and does not cause a disulfiram-like reaction either as a result of opiate use or ethanol ingestion.
Pharmacokinetics
- Absorption
- Naltrexone (injection) is an extended-release, microsphere formulation of naltrexone designed to be administered by intramuscular (IM) gluteal injection every 4 weeks or once a month. After IM injection, the naltrexone plasma concentration time profile is characterized by a transient initial peak, which occurs approximately 2 hours after injection, followed by a second peak observed approximately 2-3 days later. Beginning approximately 14 days after dosing, concentrations slowly decline, with measurable levels for greater than 1 month.
- Maximum plasma concentration (Cmax) and area under the curve (AUC) for naltrexone and 6β-naltrexol (the major metabolite) following Naltrexone (injection) administration are dose proportional. Compared to daily oral dosing with naltrexone 50 mg over 28 days, total naltrexone exposure is 3 to 4-fold higher following administration of a single dose of Naltrexone (injection) 380 mg. Steady state is reached at the end of the dosing interval following the first injection. There is minimal accumulation (<15%) of naltrexone or 6β-naltrexol upon repeat administration of Naltrexone (injection).
- Distribution
- In vitro data demonstrate that naltrexone plasma protein binding is low (21%).
- Metabolism
- Naltrexone is extensively metabolized in humans. Production of the primary metabolite, 6β-naltrexol, is mediated by dihydrodiol dehydrogenase, a cytosolic family of enzymes. The cytochrome P450 system is not involved in naltrexone metabolism. Two other minor metabolites are 2-hydroxy-3-methoxy-6β-naltrexol and 2-hydroxy-3-methoxy-naltrexone. Naltrexone and its metabolites are also conjugated to form glucuronide products.
- Significantly less 6β-naltrexol is generated following IM administration of Naltrexone (injection) compared to administration of oral naltrexone due to a reduction in first-pass hepatic metabolism.
- Elimination
- Elimination of naltrexone and its metabolites occurs primarily via urine, with minimal excretion of unchanged naltrexone.
- The elimination half life of naltrexone following Naltrexone (injection) administration is 5-10 days and is dependent on the erosion of the polymer. The elimination half life of 6β-naltrexol following Naltrexone (injection) administration is 5-10 days.
- Special Populations
- Pediatric: Pharmacokinetics of Naltrexone (injection) have not been evaluated in a pediatric population.
- Geriatric: Pharmacokinetics of Naltrexone (injection) have not been evaluated in the geriatric population.
- Race: Effect of race on the pharmacokinetics of Naltrexone (injection) has not been studied.
- Gender: In a study in healthy subjects (n=18 females and 18 males), gender did not influence the pharmacokinetics of Naltrexone (injection).
- Renal Insufficiency: A population pharmacokinetic analysis indicated mild renal insufficiency (creatinine clearance of 50-80 mL/min) had little or no influence on Naltrexone (injection) pharmacokinetics and that no dosage adjustment is necessary. Naltrexone (injection) pharmacokinetics have not been evaluated in subjects with moderate and severe renal insufficiency.
- Hepatic Insufficiency: The pharmacokinetics of Naltrexone (injection) are not altered in subjects with mild to moderate hepatic impairment (Groups A and B of the Child-Pugh classification). Naltrexone (injection) pharmacokinetics were not evaluated in subjects with severe hepatic impairment.
- Drug Interactions
- In vitro Studies: Because naltrexone is not a substrate for CYP drug metabolizing enzymes, inducers or inhibitors of these enzymes are unlikely to change the clearance of Naltrexone (injection). An in vitro CYP inhibition study demonstrated that naltrexone is not an inhibitor of major CYP enzymes (CYP 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, 3A4). An in vitro CYP induction study demonstrated that naltrexone is not an inducer of CYP3A4 and CYP1A2.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Carcinogenesis: Carcinogenicity studies have not been conducted with Naltrexone (injection).
- Carcinogenicity studies of oral naltrexone hydrochloride (administered via the diet) have been conducted in rats and mice.
- In a two-year carcinogenicity study in rats, there were small increases in the numbers of testicular mesotheliomas in males and tumors of vascular origin in males and females. The incidence of testicular mesothelioma in males given naltrexone at a dietary dose of 100 mg/kg/day (3-times the human exposure based on an AUC(0-28d) comparison) was 6%, compared with a maximum historical incidence of 4%. The incidence of vascular tumors in males and females given dietary doses of 100 mg/kg/day was 4% but only the incidence in females was increased compared with a maximum historical control incidence of 2% (3 and 32 times the human exposure based on an AUC(0-28d) comparison in males and females, respectively). There was no evidence of carcinogenicity in a 2-year dietary study with naltrexone in male and female mice (12 and 3 times the human exposure based on an AUC(0-28d) comparison, respectively). The clinical significance of these findings is not known.
- Mutagenesis: Naltrexone was negative in the following in vitro genotoxicity studies: bacterial reverse mutation assay (Ames test), the heritable translocation assay, CHO cell sister chromatid exchange assay, and the mouse lymphoma gene mutation assay. Naltrexone was also negative in an in vivo mouse micronucleus assay. In contrast, naltrexone tested positive in the following assays: Drosophila recessive lethal frequency assay, non-specific DNA damage in repair tests with E. coli and WI-38 cells, and urinalysis for methylated histidine residues.
- Impairment of Fertility: Naltrexone given via oral gavage caused a significant increase in pseudopregnancy and a decrease in pregnancy rates in rats at 100 mg/kg/day (75 times the human exposure based on an AUC(0-28d) comparison). There was no effect on male fertility at this dose level (6 times the human exposure based on an AUC(0-28d) comparison). The relevance of these observations to human fertility is not known.
Clinical Studies
Alcohol Dependence
- The efficacy of Naltrexone (injection) in the treatment of alcohol dependence was evaluated in a 24-week, placebo-controlled, multi-center, double-blind, randomized trial of alcohol-dependent (DSM-IV criteria) outpatients. Subjects were treated with an injection every 4 weeks of Naltrexone (injection) 190 mg, Naltrexone (injection) 380 mg or placebo. Oral naltrexone was not administered prior to the initial or subsequent injections of study medication. Psychosocial support was provided to all subjects in addition to medication.
- Subjects treated with Naltrexone (injection) 380 mg demonstrated a greater reduction in days of heavy drinking than those treated with placebo. Heavy drinking was defined as self-report of 5 or more standard drinks consumed on a given day for male patients and 4 or more drinks for female patients. Among the subset of patients (n=53, 8% of the total study population) who abstained completely from drinking during the week prior to the first dose of medication, compared with placebo-treated patients, those treated with Naltrexone (injection) 380 mg had greater reductions in the number of drinking days and the number of heavy drinking days. In this subset, patients treated with Naltrexone (injection) were also more likely than placebo-treated patients to maintain complete abstinence throughout treatment. The same treatment effects were not evident among the subset of patients (n=571, 92% of the total study population) who were actively drinking at the time of treatment initiation.
Opioid Dependence
- The efficacy of Naltrexone (injection) in the treatment of opioid dependence was evaluated in a 24-week, placebo-controlled, multi-center, double-blind, randomized trial of opioid-dependent (DSM-IV) outpatients, who were completing or had recently completed detoxification. Subjects were treated with an injection every 4 weeks of Naltrexone (injection) 380 mg or placebo. Oral naltrexone was not administered prior to the initial or subsequent injections of study medication. Standardized, manual-based psychosocial support was provided on a biweekly basis to all subjects in addition to medication.
- FIGURE 1, below, displays the cumulative percentage of subjects with opioid-free weeks ranging from no visits (0%) to all visits (100%). An opioid-free week was one in which urine drug test results were negative for opioids and self-reported opioid use was also zero. An initial period of engagement in treatment was permitted during which opiate use, if it occurred, was not considered in the analysis. Subjects discontinuing from the trial were assumed to have had opioid-use weeks for the weeks after dropout.
- The cumulative percentage of subjects achieving each observed percentage of opioid-free weeks was greater in the Naltrexone (injection) group compared to the placebo group. Complete abstinence (opioid-free at all weekly visits) was sustained by 23% of subjects in the placebo group compared with 36% of subjects in the Naltrexone (injection) group from Week 5 to Week 24.
Figure 1: Subjects Sustaining Varying Percentages of Opioid-Free Weeks

- A greater percentage of subjects in the Naltrexone (injection) group remained in the study compared to the placebo group.
How Supplied
VIVITROL (naltrexone for extended-release injectable suspension) is supplied in single-use cartons. Each carton contains one 380-mg vial of VIVITROL microspheres, one vial containing 4 mL (to deliver 3.4 mL) of diluent for the suspension of VIVITROL, one 5-mL prepackaged syringe, one 1-inch 20-gauge needle, two 1.5-inch 20-gauge needles and two 2-inch 20-gauge needles with needle protection devices: NDC 65757-300-01.
Storage
The entire dose pack should be stored in the refrigerator (2 - 8°C, 36 - 46°F). Unrefrigerated, VIVITROL can be stored at temperatures not exceeding 25°C (77°F) for no more than 7 days prior to administration. Do not expose the product to temperatures above 25°C (77°F). VIVITROL should not be frozen.
Parenteral products should be visually inspected for particulate matter and discoloration prior to administration whenever solution and container permit. A properly mixed suspension will be milky white, will not contain clumps, and will move freely down the wall of the vial.
Keep out of Reach of Children.
Images
Drug Images
{{#ask: Page Name::Naltrexone (injection) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel




{{#ask: Label Page::Naltrexone (injection) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Patient Information
- Physicians should include the following issues in discussions with patients for whom they prescribe VIVITROL:
- Advise patients that if they previously used opioids, they may be more sensitive to lower doses of opioids and at risk of accidental overdose should they use opioids when their next dose is due, if they miss a dose, or after VIVITROL treatment is discontinued. It is important that patients inform family members and the people closest to the patient of this increased sensitivity to opioids and the risk of overdose.
- Advise patients that because VIVITROL can block the effects of opioids, patients will not perceive any effect if they attempt to self-administer heroin or any other opioid drug in small doses while on VIVITROL. Further, emphasize that administration of large doses of heroin or any other opioid to try to bypass the blockade and get high while on VIVITROL may lead to serious injury, coma, or death.
- Patients on VIVITROL may not experience the expected effects from opioid-containing analgesic, antidiarrheal, or antitussive medications.
- Advise patients that a reaction at the site of VIVITROL injection may occur. Reactions include pain, tenderness, induration, swelling, erythema, bruising, or pruritus. Serious injection site reactions including necrosis may occur. Some of these injection site reactions have required surgery. Patients should receive their injection from a healthcare provider qualified to administer the injection. Patients should be advised to seek medical attention for worsening skin reactions.
- Advise patients that they should be off all opioids, including opioid-containing medicines, for a minimum of 7 – 10 days before starting VIVITROL in order to avoid precipitation of opioid withdrawal. :*Patients transitioning from buprenorphine or methadone may be vulnerable to precipitation of withdrawal symptoms for as long as two weeks. Ensure that patients understand that withdrawal precipitated by administration of an opioid antagonist may be severe enough to require hospitalization if they have not been opioid-free for an adequate period of time, and is different from the experience of spontaneous withdrawal that occurs with discontinuation of opioid in a dependent individual. :*Advise patients that they should not take VIVITROL if they have any symptoms of opioid withdrawal. :*Advise all patients, including those with alcohol dependence, that it is imperative to notify healthcare providers of any recent use of opioids or any history of opioid dependence before starting VIVITROL to avoid precipitation of opioid withdrawal.
- Advise patients that VIVITROL may cause liver injury. Patients should immediately notify their physician if they develop symptoms and/or signs of liver disease.
- Advise patients that they may experience depression while taking VIVITROL. It is important that patients inform family members and the people closest to the patient that they are taking VIVITROL and that they should call a doctor right away should they become depressed or experience symptoms of depression.
- Advise patients to carry documentation to alert medical personnel to the fact that they are taking VIVITROL (naltrexone for extended-release injectable suspension). This will help to ensure that patients obtain adequate medical treatment in an emergency.
- Advise patients that VIVITROL may cause an allergic pneumonia. Patients should immediately notify their physician if they develop signs and symptoms of pneumonia, including dyspnea, coughing, or wheezing.
- Advise patients that they should not take VIVITROL if they are allergic to VIVITROL or any of the microsphere or diluent components.
- Advise patients that they may experience nausea following the initial injection of VIVITROL. These episodes of nausea tend to be mild and subside within a few days post-injection. Patients are less likely to experience nausea in subsequent injections. Patients should be advised that they may also experience tiredness, headache, vomiting, decreased appetite, painful joints and muscle cramps.
- Advise patients that because VIVITROL is an intramuscular injection and not an implanted device, once VIVITROL is injected, it is not possible to remove it from the body.
- Advise patients that VIVITROL has been shown to treat alcohol and opioid dependence only when used as part of a treatment program that includes counseling and support.
- Advise patients that dizziness may occur with VIVITROL treatment, and they should avoid driving or operating heavy machinery until they have determined how VIVITROL affects them.
- Advise patients to notify their physician if they:
- become pregnant or intend to become pregnant during treatment with VIVITROL.
are breast-feeding.
- experience respiratory symptoms such as dyspnea, coughing, or wheezing when taking VIVITROL.
- experience any allergic reactions when taking VIVITROL.
- experience other unusual or significant side effects while on VIVITROL therapy.
- Patients should be advised of any other risks and information based on the clinical judgment of their physician.

Precautions with Alcohol
- Alcohol-Naltrexone (injection) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- VIVITROL®[1]
Look-Alike Drug Names
There is limited information regarding Naltrexone (injection) Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.