Minimal change disease electron microscopy
|
Minimal Change Disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Minimal change disease electron microscopy On the Web |
|
American Roentgen Ray Society Images of Minimal change disease electron microscopy |
|
Risk calculators and risk factors for Minimal change disease electron microscopy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Yazan Daaboul, Serge Korjian, Vamsikrishna Gunnam M.B.B.S [2]
Overview
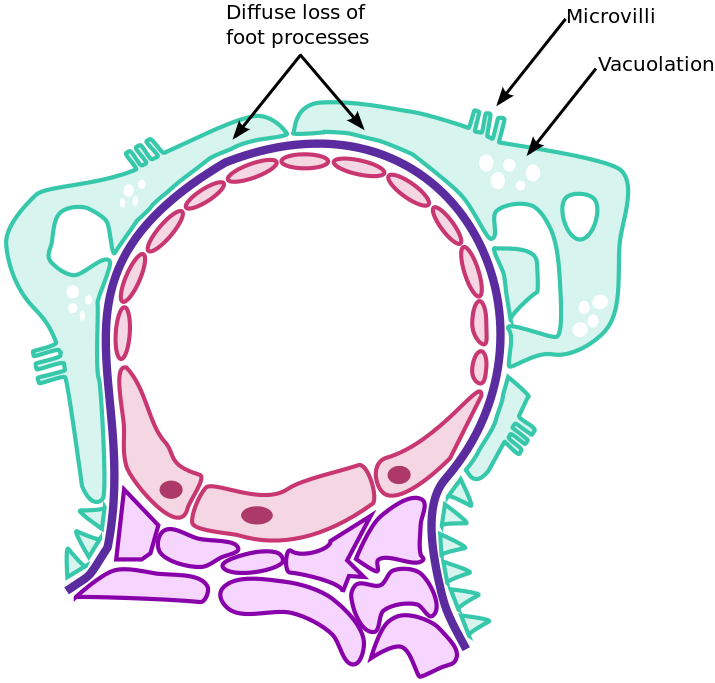
A kidney biopsy is not routinely performed as soon as the nephrotic syndrome is found in lab work-up. According to the National Kidney Foundation (NKF) Kidney Disease – Improve Global Outcomes (KDIGO) guidelines in 2012, an initial attempt using corticosteroids should be performed before a renal biopsy is performed. Electron microscopy is required for the diagnosis of minimal change disease. It shows effacement (fusion) of podocytes, which are visceral epithelial cells, with slit-pore membrane obliteration between podocyte foot processes. However, podocyte effacement is not specific and should not be considered pathognomonic of the disease.
Electron microscopy
- Effacement of foot processes is seen in minimal change disease on electron microscopy and this is the only morphologic feature of minimal change disease on electron microscopy.[1][2][3]
References
- ↑ Vivarelli, Marina; Massella, Laura; Ruggiero, Barbara; Emma, Francesco (2017). "Minimal Change Disease". Clinical Journal of the American Society of Nephrology. 12 (2): 332–345. doi:10.2215/CJN.05000516. ISSN 1555-9041.
- ↑ Beck L, Bomback AS, Choi MJ, Holzman LB, Langford C, Mariani LH; et al. (2013). "KDOQI US commentary on the 2012 KDIGO clinical practice guideline for glomerulonephritis". Am J Kidney Dis. 62 (3): 403–41. doi:10.1053/j.ajkd.2013.06.002. PMID 23871408.
- ↑ D'Agati V (2003). "Pathologic classification of focal segmental glomerulosclerosis". Semin Nephrol. 23 (2): 117–34. doi:10.1053/snep.2003.50012. PMID 12704572.