Lower gastrointestinal bleeding initial resuscitation
|
Lower gastrointestinal bleeding Microchapters |
|
Differentiating Lower gastrointestinal bleeding from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Management |
|
Surgery |
|
Case Studies |
|
Lower gastrointestinal bleeding initial resuscitation On the Web |
|
American Roentgen Ray Society Images of Lower gastrointestinal bleeding initial resuscitation |
|
FDA on Lower gastrointestinal bleeding initial resuscitation |
|
CDC on Lower gastrointestinal bleeding initial resuscitation |
|
Lower gastrointestinal bleeding initial resuscitation in the news |
|
Blogs on Lower gastrointestinal bleeding initial resuscitation |
|
Risk calculators and risk factors for Lower gastrointestinal bleeding initial resuscitation |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor(s)-in-Chief: Aditya Ganti M.B.B.S. [2]
Overview
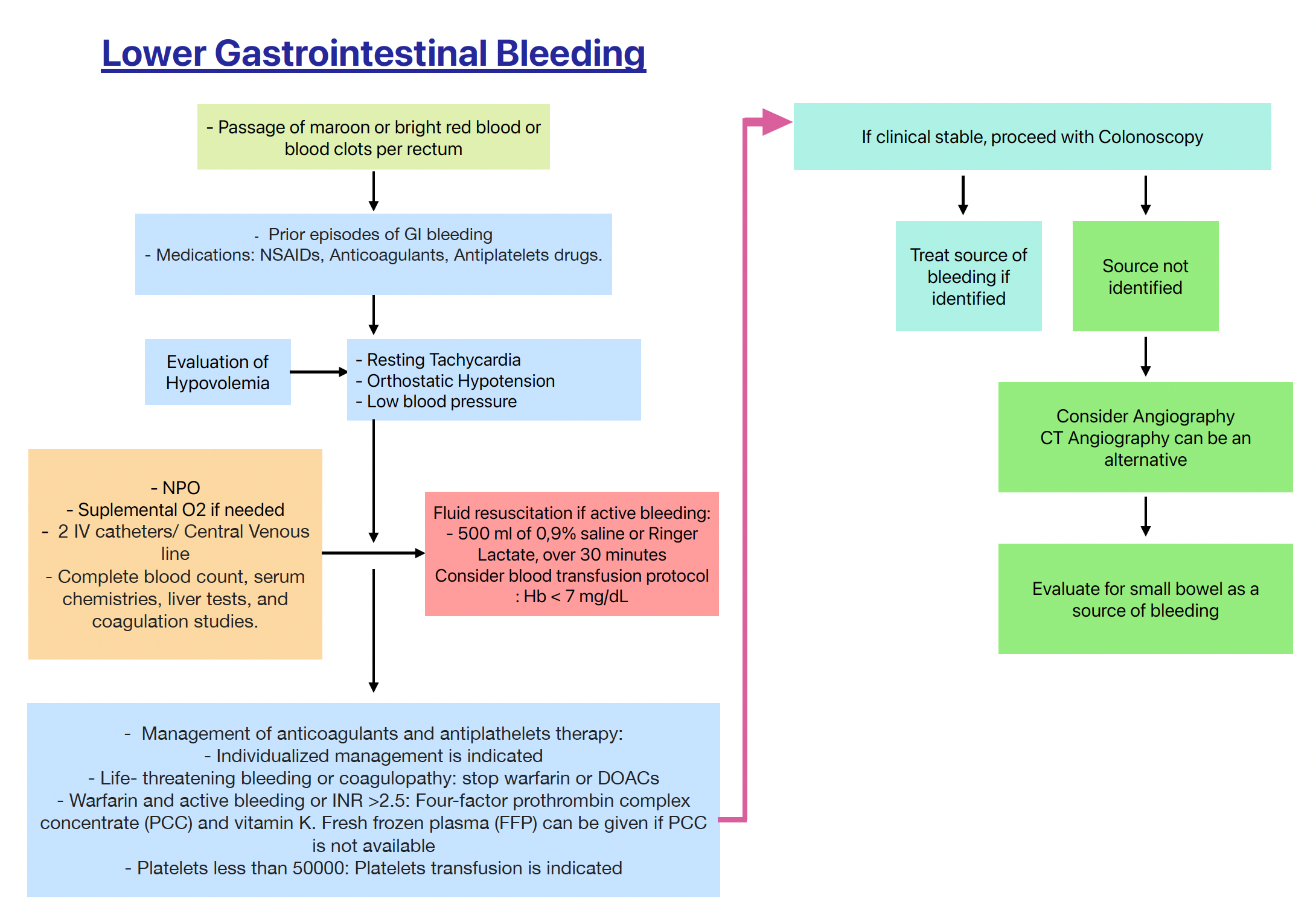
The aims of treatment in a patient presenting with lower gastrointestinal bleeding are to resuscitate the patient, identify the source of blood loss and stop any ongoing bleeding, and reduce the risk of a recurrent bleed. It is essential to identify patients who are high risk. This would include elderly patients; those with severe ongoing bleeding or recurrent bleeding; and patients with multiple comorbid conditions, in particular, those patients with cardiac, renal, respiratory, and liver disease. Treatment depends on the mode of presentation, the severity of the bleed, and the underlying pathology. Bleeding points can be treated with endoscopy, interventional radiology, or surgery. After identification of the source of bleeding using endoscopy, therapeutic options include monopolar or bipolar diathermy, argon plasma coagulation (APC), epinephrine injections, and endoloops and hemoclips, used individually or in combination. These methods can be used to treat many of the causes of LGIB, including diverticular bleeding, angiodysplasia, radiation proctitis, and post-polypectomy bleeding interventional radiology can be used to visualize a bleeding vessel and to stop the bleeding through embolization of the vessel. Surgery may be required if less invasive measures cannot be applied or are not effective.
Initial Resuscitation
Initial Evaluation
- In patients with acute lower gastrointestinal bleeding who are unstable rapid assessment and resuscitation should be initiated even before diagnostic evaluation.[1][2][3][1][4][5][6][7]
- The initial steps in the management of a patient with lower gastrointestinal bleeding are to assess the severity of bleeding, and then institute fluid and blood resuscitation as needed.
- Once hemodynamic stability is achieved, nasogastric lavage should be performed to rule of upper GI source.
- Equilibration between the intravascular and extravascular volumes cannot be achieved until 24 to 72 hours after bleeding has occurred.
Role of Nasogastric tube (NGT)
- Nasogastric tube (NGT) lavage is recommended in all patients with lower gastrointestinal bleeding once the patient is stabilized.
- A carefully placed nasogastric tube (NGT) with irrigation and aspiration of bile is necessary to ensure sampling of duodenal contents.
- If there is a bloody NGT aspirate then an esophagogastroduodenoscopy (EGD) is warranted (11 to 15% of patients despite “negative” NGT aspirates are due to upper GI bleeding).
- Obtaining clear fluid favors a lower GI source of bleeding.
| Workup and Initial Management | |
|---|---|
| Initial Evaluation |
|
| Supportive Therapy |
|
| Blood transfusion |
|
Assessment of severity of bleeding
| Bleeding severity | Vital signs | Blood loss |
|---|---|---|
| Minor | Normal | <10% |
| Moderate | Postural hypotension | 10-20% |
| Severe | Shock | >25% |
Fluid resuscitation
- Two large caliber (16-gauge) peripheral catheters or a central venous line should be inserted in patients who are hemodynamically unstable.
- The rate of fluid resuscitation is proportional to the severity of bleeding with the goal of restoring and maintaining the patient’s blood pressure.
- Infusion of 500 mL of normal saline or lactated Ringer's solution over 30 minutes is preferred treatment for patients with active bleeding before blood type matching and blood transfusion.
- Intensive monitoring with a pulmonary artery catheter is recommended to monitor the response of initial resuscitation efforts and any complications of fluid overload.
- If the blood pressure fails to respond to initial resuscitation, the rate of fluid administration should be increased and urgent intervention (eg, angiography) considered.
Blood transfusion
- Patients with severe bleeding need to be transfused.[8][9]
- Fresh frozen plasma, platelets, or both should be given to patients with coagulopathy who are actively bleeding and to those who have received more than 10 units of packed erythrocytes.
| Indications for transfusion | |
|---|---|
| Age | Target Hematocrit |
| Elderly patient ( >45) | 30% |
| Younger patient (<45) | 25% |
| Patients with portal hypertension | 28% |
Triage and consultations
- All patients with visible rectal bleeding warrants an immediate evaluation in all cases. The timing and setting of the evaluation depends upon the severity of bleeding and the patient's comorbid illnesses.
- A gastroenterology consultation should be obtained early in the hospital course of patients with acute lower GI bleeding.
| Evaluation setting | Patient catagories |
|---|---|
| ICU | Patients with high-risk features. |
| Outpatient | Patients with low-risk features.† |
| Regular Ward | Most other patients can be admitted to a regular medical ward.♦ |
| |
Risk stratification
- Clinical features can predict the risk of complications in patients with presumed acute lower GI bleeding. These features can also be used to categorize patients as either low or high risk.
- The presence of more number of high-risk features directly correlates with the likelihood of a poor outcome.
| High-risk features |
|---|
|
References
- ↑ 1.0 1.1 Strate LL, Gralnek IM (2016). "ACG Clinical Guideline: Management of Patients With Acute Lower Gastrointestinal Bleeding". Am. J. Gastroenterol. 111 (4): 459–74. doi:10.1038/ajg.2016.41. PMC 5099081. PMID 26925883.
- ↑ Barnert J, Messmann H (2009). "Diagnosis and management of lower gastrointestinal bleeding". Nat Rev Gastroenterol Hepatol. 6 (11): 637–46. doi:10.1038/nrgastro.2009.167. PMID 19881516.
- ↑ Barnert J, Messmann H (2008). "Management of lower gastrointestinal tract bleeding". Best Pract Res Clin Gastroenterol. 22 (2): 295–312. doi:10.1016/j.bpg.2007.10.024. PMID 18346685.
- ↑ Raphaeli T, Menon R (2012). "Current treatment of lower gastrointestinal hemorrhage". Clin Colon Rectal Surg. 25 (4): 219–27. doi:10.1055/s-0032-1329393. PMC 3577609. PMID 24294124.
- ↑ Ghassemi KA, Jensen DM (2013). "Lower GI bleeding: epidemiology and management". Curr Gastroenterol Rep. 15 (7): 333. doi:10.1007/s11894-013-0333-5. PMC 3857214. PMID 23737154.
- ↑ Beck DE, Margolin DA, Whitlow CB, Hammond KL (2007). "Evaluation and management of gastrointestinal bleeding". Ochsner J. 7 (3): 107–13. PMC 3096402. PMID 21603524.
- ↑ Triadafilopoulos G (2012). "Management of lower gastrointestinal bleeding in older adults". Drugs Aging. 29 (9): 707–15. doi:10.1007/s40266-012-0008-1. PMID 23018607.
- ↑ Al-Jaghbeer M, Yende S (2013). "Blood transfusion for upper gastrointestinal bleeding: is less more again?". Crit Care. 17 (5): 325. doi:10.1186/cc13020. PMC 4056793. PMID 24063362.
- ↑ Villanueva C, Colomo A, Bosch A, Concepción M, Hernandez-Gea V, Aracil C, Graupera I, Poca M, Alvarez-Urturi C, Gordillo J, Guarner-Argente C, Santaló M, Muñiz E, Guarner C (2013). "Transfusion strategies for acute upper gastrointestinal bleeding". N. Engl. J. Med. 368 (1): 11–21. doi:10.1056/NEJMoa1211801. PMID 23281973.