Junctional rhythm
|
WikiDoc Resources for Junctional rhythm |
|
Articles |
|---|
|
Most recent articles on Junctional rhythm Most cited articles on Junctional rhythm |
|
Media |
|
Powerpoint slides on Junctional rhythm |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Junctional rhythm |
|
Clinical Trials |
|
Ongoing Trials on Junctional rhythm at Clinical Trials.gov Trial results on Junctional rhythm Clinical Trials on Junctional rhythm at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Junctional rhythm NICE Guidance on Junctional rhythm
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Junctional rhythm Discussion groups on Junctional rhythm Patient Handouts on Junctional rhythm Directions to Hospitals Treating Junctional rhythm Risk calculators and risk factors for Junctional rhythm
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Junctional rhythm |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ahmed Elsaiey, MBBCH [2]
See also: Junctional bradycardia for slow junctional rhythms, and junctional tachycardia for fast jucntional rhythms
Overview
Junctional rhythm describes an abnormal heart rhythm resulting from impulses coming from a locus of tissue in the area of the atrioventricular node, the "junction" between atria and ventricles. Junctional rhythm can be classified into junction escape rhythm, accelerated junctional rhythm, junctional bradycardia, and junctional tachycardia. The junctional rhythm can be originated by many medications that affect the sinoatrial node and make the atrioventricular node an ectopic impulses foci. Many conditions as well causes junctional rhythm by creating new pacemaker instead of the sinoatrial node. In junctional rhythm, the heart beats rate are not controlled by the sinoatrial node. The new pacemaker in the junctional rhythm is the atrioventricular node. Common causes of junctional rhythm include acute MI, Acute rheumatic fever, antiarrhythmic agents, beta-blockers, calcium channel blockers, Complete heart block, Conduction system disease, Digitalis toxicity, Diphtheria, Healthy response during sleep in patients with heightened vagal tone, Heart surgery particularly valve replacement or surgery for congenital heart disease, Ischemic heart disease, Lyme disease, NSTEMI, Sick sinus syndrome, Sinus arrest, Chest trauma, Radiation therapy, Collagen vascular disease, Myocarditis, Clonidine, Reserpine, Adenosine, and Cimetidine. In the United States, the prevalence of junctional rhythm is 166 in 100,000 individuals with sinus node dysfunction. If left untreated, junctional rhythm can lead to syncope and other severe complications. Patients presenting with juncitonal rhythm disease should be asked properly for history of other cardiac conditions as heart failure and sick sinus syndrome. Symptoms of junctional rhythm can be non specific and includes syncope, dizziness, and faitgue. Physical examination findings of junctional rhythm include pulsating veins and canon a waves in case the right atrium contracting against a closed tricuspid valve. Electrocardiogram may show QRS complexes are narrow as conduction down the His bundle is normal. The junctional rate may be slow (40-60 beats per minute) in which case the rhythm is referred to as junctional bradycardia. The junctional rate may be rapid in which case the rhythm is referred to as a junctional tachycardia. Asymptomatic patients with only juncitonal rhythm and no other cardiac conditions do not require further management. The rhythm here is due to increased vagal tone only. Patients with sinus node dysfunction should be managed cautiously as the pulse originating from other foci keeps the heart rate. Patients with junctional rhythm due to digoxin toxicity are given atropine and digoxin specific antibody. In children, symptomatic patients can undergo percutaneous radiofrequency ablation. Pacemaker is indicated for patients with sick sinus syndrome and complete AV block.
Classification
- Junctional rhythm can be classified according to the rate of the heart rate as the following:[1][2][3]
Junctional Rhythm
- The junctional rate is normal.
Junction escape rhythm:
- The junctional rate is about 40-60 beats per minute.
Accelerated junctional rhythm:
- The juncitonal rate can be accelerated (60-100 beats per minute).
Junctional Bradycardia
- The junctional rate may be slow (40-60 beats per minute) in which case the rhythm is referred to as junctional bradycardia.
Junctional Tachycardia
- The junctional rate may be rapid in which case the rhythm is referred to as a junctional tachycardia.
Pathophysiology
Physiology
- The sinoatrial node in the heart is the pacemaker that determine the rate of the heart beats. The electrical impulse starts from the sinoatrial node then travels through the atria. It continues through the bundle of his, Purkinje fibers, and the ventricles ending one heart beat.[4][5]
- This sinus rhythm indicates the atria normally contracts before the ventricles.
Pathogenesis
- The junctional rhythm can be originated by many medications that affect the sinoatrial node and make the atrioventricular node an ectopic impulses foci. Many conditions as well causes junctional rhythm by creating new pacemaker instead of the sinoatrial node.[6]
- In junctional rhythm, the heart beats rate are not controlled by the sinoatrial node. The new pacemaker in the junctional rhythm is the atrioventricular node.[7]
- The atria contracts before the ventricles but from a different signal. The impulse contracting the atria comes from the ventricles not the normal impulse coming from the sinoatrial node.[8][9]
- Junctional tacycardia:[10][11]
- Occurs when the atrioventricular node becomes the pacemaker and spreads impulse in a rapid pattern.
- It takes place when the myocardial tissue is inflammed and ischemic as in patients undergo a heart surgery.
Causes
- Common causes of junctional rhythm include the following diseases and medications:[12]
- Acute MI
- Acute rheumatic fever
- Antiarrhythmic agents
- Beta-blockers
- Calcium channel blockers
- Complete heart block
- Conduction system disease
- Digitalis toxicity
- Diphtheria
- Healthy response during sleep in patients with heightened vagal tone
- Heart surgery particularly valve replacement or surgery for congenital heart disease
- Ischemic heart disease
- Lyme disease
- NSTEMI
- Sick sinus syndrome
- Sinus arrest
- Sinus bradycardia
- STEMI particularly inferior MI involving the posterior descending artery causing ischemia of the AV node due to poor perfusion in the AV nodal artery
- Chest trauma
- Radiation therapy
- Collagen vascular disease
- Myocarditis
- Clonidine
- Reserpine
- Adenosine
- Cimetidine
- Antiarrhythmics class I to IV
- Lithium
- Amitriptyline
- Neuromuscular disorder
- X-linked muscular dystrophy
- Familial disorder
- Vasovagal simulation (endotracheal suctioning)
- Carotid sinus hypersensitivity
- Opioids
- Cannabinoids
- Isoproterenol infusion
- Hypothyroidism
- Sleep apnea
- Hypoxia
- Intracranial hypertension
- Hyperkalemia
- Anorexia nervosa
- Amyloidosis
- Pericarditis
- Rheumatic fever
- Repair of congenital heart disease
- Inherited channelopathy
Differentiating Junctional Rhythm from other diseases
- Junctional rhythm must be differentiated from other diseases that cause abnormal cardiac electrical conduction.
| Arrhythmia | Rhythm | Rate | P wave | PR Interval | QRS Complex | Response to Maneuvers | Epidemiology | Co-existing Conditions | |
|---|---|---|---|---|---|---|---|---|---|
| Junctional rhythm[13][12] |
|
|
|
|
|||||
| Atrioventricular block[14] | First degree [15][16] |
|
|
|
|
|
|
| |
| Second degree[17][18] |
|
|
|
QRS is normal but dropped as the following:
|
|
| |||
| Third degree[19][20] |
|
|
|
|
|
| |||
| Atrial Fibrillation (AFib)[21][22] |
|
|
|
|
|
|
|
| |
| Atrial Flutter[23] |
|
|
|
|
|
|
|
||
| Atrioventricular nodal reentry tachycardia (AVNRT)[24][25][26][27] |
|
|
|
|
|
|
|
||
| Multifocal Atrial Tachycardia[28][29] |
|
|
|
|
|
|
|
||
| Paroxysmal Supraventricular Tachycardia |
|
|
|
|
|
|
|
||
| Premature Atrial Contractrions (PAC)[30][31] |
|
|
|
|
|
|
|||
| Wolff-Parkinson-White Syndrome[32][33] |
|
|
|
|
|
|
|
| |
Epidemiology and Demographics
Prevalence
- In the United States, the prevalence of junctional rhythm is 166 in 100,000 individuals with sinus node dysfunction.[13]
Age
- The prevalence of junctional rhythm increases with age.
Gender
- Men and women are affected equally by juntional rhythm.
Natural History, Complications and Prognosis
Natural History
- If left untreated, junctional rhythm can lead to syncope and other severe complications.[34]
Complications
- Complications of junctional rhythm include the following:[34]
- Syncope
- Dizziness
- Fatigue
Prognosis
- Prognosis of junctional rhythm is good with the proper treatment.
History and Symptoms
History
- Patients presenting with juncitonal rhythm disease should be asked properly for history of other cardiac conditions.
- Other cardiac conditions can affect the presentation of the patients. These cardiac conditions include:
- Heart failure
- Sick sinus syndrome
Symptoms
- Patients with juncitonal rhythm disease can be asymptomatic.
- Symptoms of junctional rhythm can be non specific and includes the following:
- Dizziness
- Fatigue
- Syncope
- Palpitaions
- Symptoms vary according to the underlying cause of junctional rhythm as the following:[35][36][37]
- Heart failure:
- Shortness of breath
- Lower extremities edema
- Valve dysfunction due to rheumatic fever:
- Fever
- Arthritis
- Skin rash
- Heart failure:
Physical Examination
- Common physical examination findings of junctional rhythm include the following:
- Pulsating veins
- Canon a waves in case the right atrium contracting against a closed tricuspid valve
- Regular heart rate in most of cases ranging from 40 to 60 beat per minute
Diagnosis
Electrocardiogram
- The QRS complexes are narrow in so far as conduction down the His bundle is normal
- The junctional rate may be slow (40-60 beats per minute) in which case the rhythm is referred to as junctional bradycardia
- The junctional rate may be normal as shown in the tracing below
- The junctional rate may be rapid in which case the rhythm is referred to as a junctional tachycardia
- There is dissociation of the narrow complex QRS from an upright atrial p wave or the p wave is missing, or the p wave is retrograde (a retrograde p wave) due to retrograde conduction from the AV node back into the atrium.
EKG Examples
Shown below is an EKG depicting AV dissociation with variable timing of the p wave in relation to the QRS. A narrow complex junctional escape rhythm at 75 beats per minute is present.
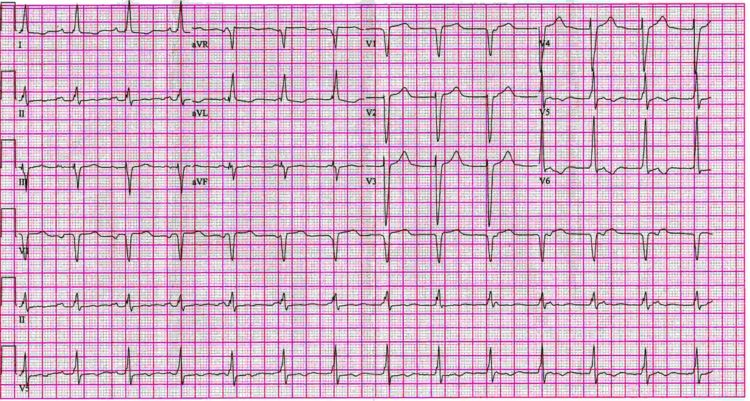
Shown below is an EKG with a a regular rhythm at a rate of about 43/minute. There are no P waves to be seen and the QRS duration is about 80 ms. This is a nodal rhythm.

Copyleft images obtained courtesy of ECGpedia, http://en.ecgpedia.org.
Treatment
Medical therapy
- The underlying cause of junctional rhythm should be defined first before attempting treatment.
- Asymptomatic patients with only juncitonal rhythm and no other cardiac conditions do not require further management. The rhythm here is due to increased vagal tone only.
- Patients with sinus node dysfunction should be managed cautiously as the pulse originating from other foci keeps the heart rate.
- Patients with junctional rhythm due to digoxin toxicity are given atropine and digoxin specific antibody.[38][39]
- Patients who do not respond to the usual medical therapy can be administered phenytoin.
Surgery
- In children, symptomatic patients can undergo percutaneous radiofrequency ablation. [40]
- Pacemaker:[41]
- Indicated for patients with sick sinus syndrome and complete AV block.
Related Chapters
References
- ↑ Spodick DH (1992). "Normal sinus heart rate: sinus tachycardia and sinus bradycardia redefined". Am Heart J. 124 (4): 1119–21. doi:10.1016/0002-8703(92)91012-p. PMID 1529897.
- ↑ Thery C, Gosselin B, Lekieffre J, Warembourg H (1977). "Pathology of sinoatrial node. Correlations with electrocardiographic findings in 111 patients". Am Heart J. 93 (6): 735–40. doi:10.1016/s0002-8703(77)80070-7. PMID 871100.
- ↑ Dobrzynski H, Anderson RH, Atkinson A, Borbas Z, D'Souza A, Fraser JF; et al. (2013). "Structure, function and clinical relevance of the cardiac conduction system, including the atrioventricular ring and outflow tract tissues". Pharmacol Ther. 139 (2): 260–88. doi:10.1016/j.pharmthera.2013.04.010. PMID 23612425.
- ↑ Merriam-Webster dictionary > Junctional rhythm Retrieved September 2010
- ↑ Kim D, Shinohara T, Joung B, Maruyama M, Choi EK, On YK; et al. (2010). "Calcium dynamics and the mechanisms of atrioventricular junctional rhythm". J Am Coll Cardiol. 56 (10): 805–12. doi:10.1016/j.jacc.2010.03.070. PMC 3050609. PMID 20797495.
- ↑ Silvestri NJ, Ismail H, Zimetbaum P, Raynor EM (2018). "Cardiac involvement in the muscular dystrophies". Muscle Nerve. 57 (5): 707–715. doi:10.1002/mus.26014. PMID 29130502.
- ↑ eMedicine:"Junctional Rhythms" http://www.emedicine.com/MED/topic1212.htm
- ↑ medical dictionary http://medical-dictionary.thefreedictionary.com/retrograde+conduction
- ↑ Dobrzynski H, Anderson RH, Atkinson A, Borbas Z, D'Souza A, Fraser JF; et al. (2013). "Structure, function and clinical relevance of the cardiac conduction system, including the atrioventricular ring and outflow tract tissues". Pharmacol Ther. 139 (2): 260–88. doi:10.1016/j.pharmthera.2013.04.010. PMID 23612425.
- ↑ Liu CF, Ip JE, Lin AC, Lerman BB (2013). "Mechanistic heterogeneity of junctional ectopic tachycardia in adults". Pacing Clin Electrophysiol. 36 (1): e7–10. doi:10.1111/j.1540-8159.2011.03214.x. PMID 21954877.
- ↑ Di Biase L, Gianni C, Bagliani G, Padeletti L (2017). "Arrhythmias Involving the Atrioventricular Junction". Card Electrophysiol Clin. 9 (3): 435–452. doi:10.1016/j.ccep.2017.05.004. PMID 28838549.
- ↑ 12.0 12.1 Trappe HJ (2010). "Tachyarrhythmias, bradyarrhythmias and acute coronary syndromes". J Emerg Trauma Shock. 3 (2): 137–42. doi:10.4103/0974-2700.62112. PMC 2884444. PMID 20606790.
- ↑ 13.0 13.1 Romhilt DW, Doyle M, Sagar KB, Hastillo A, Wolfgang TC, Lower RR; et al. (1982). "Prevalence and significance of arrhythmias in long-term survivors of cardiac transplantation". Circulation. 66 (2 Pt 2): I219–22. PMID 6177443.
- ↑ Kerola T, Eranti A, Aro AL, Haukilahti MA, Holkeri A, Junttila MJ; et al. (2019). "Risk Factors Associated With Atrioventricular Block". JAMA Netw Open. 2 (5): e194176. doi:10.1001/jamanetworkopen.2019.4176. PMC 6632153 Check
|pmc=value (help). PMID 31125096. - ↑ Barold SS (1996). "Indications for permanent cardiac pacing in first-degree AV block: class I, II, or III?". Pacing Clin Electrophysiol. 19 (5): 747–51. doi:10.1111/j.1540-8159.1996.tb03355.x. PMID 8734740.
- ↑ Upshaw CB (2004). "Comparison of the prevalence of first-degree atrioventricular block in African-American and in Caucasian patients: an electrocardiographic study III". J Natl Med Assoc. 96 (6): 756–60. PMC 2568382. PMID 15233485.
- ↑ Zehender M, Meinertz T, Keul J, Just H (1990). "ECG variants and cardiac arrhythmias in athletes: clinical relevance and prognostic importance". Am Heart J. 119 (6): 1378–91. doi:10.1016/s0002-8703(05)80189-9. PMID 2191578.
- ↑ Friedman HS, Gomes JA, Haft JI (1975). "An analysis of Wenckebach periodicity". J Electrocardiol. 8 (4): 307–15. doi:10.1016/s0022-0736(75)80003-3. PMID 1176840.
- ↑ OSTRANDER LD, BRANDT RL, KJELSBERG MO, EPSTEIN FH (June 1965). "ELECTROCARDIOGRAPHIC FINDINGS AMONG THE ADULT POPULATION OF A TOTAL NATURAL COMMUNITY, TECUMSEH, MICHIGAN". Circulation. 31: 888–98. doi:10.1161/01.cir.31.6.888. PMID 14297523.
- ↑ Movahed MR, Hashemzadeh M, Jamal MM (October 2005). "Increased prevalence of third-degree atrioventricular block in patients with type II diabetes mellitus". Chest. 128 (4): 2611–4. doi:10.1378/chest.128.4.2611. PMID 16236932.
- ↑ Lankveld TA, Zeemering S, Crijns HJ, Schotten U (July 2014). "The ECG as a tool to determine atrial fibrillation complexity". Heart. 100 (14): 1077–84. doi:10.1136/heartjnl-2013-305149. PMID 24837984.
- ↑ Harris K, Edwards D, Mant J (2012). "How can we best detect atrial fibrillation?". J R Coll Physicians Edinb. 42 Suppl 18: 5–22. doi:10.4997/JRCPE.2012.S02. PMID 22518390.
- ↑ Cosío FG (June 2017). "Atrial Flutter, Typical and Atypical: A Review". Arrhythm Electrophysiol Rev. 6 (2): 55–62. doi:10.15420/aer.2017.5.2. PMC 5522718. PMID 28835836.
- ↑ Katritsis DG, Josephson ME (August 2016). "Classification, Electrophysiological Features and Therapy of Atrioventricular Nodal Reentrant Tachycardia". Arrhythm Electrophysiol Rev. 5 (2): 130–5. doi:10.15420/AER.2016.18.2. PMC 5013176. PMID 27617092.
- ↑ Letsas KP, Weber R, Siklody CH, Mihas CC, Stockinger J, Blum T, Kalusche D, Arentz T (April 2010). "Electrocardiographic differentiation of common type atrioventricular nodal reentrant tachycardia from atrioventricular reciprocating tachycardia via a concealed accessory pathway". Acta Cardiol. 65 (2): 171–6. doi:10.2143/AC.65.2.2047050. PMID 20458824.
- ↑ "Atrioventricular Nodal Reentry Tachycardia (AVNRT) - StatPearls - NCBI Bookshelf".
- ↑ Schernthaner C, Danmayr F, Strohmer B (2014). "Coexistence of atrioventricular nodal reentrant tachycardia with other forms of arrhythmias". Med Princ Pract. 23 (6): 543–50. doi:10.1159/000365418. PMC 5586929. PMID 25196716.
- ↑ Scher DL, Arsura EL (September 1989). "Multifocal atrial tachycardia: mechanisms, clinical correlates, and treatment". Am. Heart J. 118 (3): 574–80. doi:10.1016/0002-8703(89)90275-5. PMID 2570520.
- ↑ Goodacre S, Irons R (March 2002). "ABC of clinical electrocardiography: Atrial arrhythmias". BMJ. 324 (7337): 594–7. doi:10.1136/bmj.324.7337.594. PMC 1122515. PMID 11884328.
- ↑ Lin CY, Lin YJ, Chen YY, Chang SL, Lo LW, Chao TF, Chung FP, Hu YF, Chong E, Cheng HM, Tuan TC, Liao JN, Chiou CW, Huang JL, Chen SA (August 2015). "Prognostic Significance of Premature Atrial Complexes Burden in Prediction of Long-Term Outcome". J Am Heart Assoc. 4 (9): e002192. doi:10.1161/JAHA.115.002192. PMC 4599506. PMID 26316525.
- ↑ Strasburger JF, Cheulkar B, Wichman HJ (December 2007). "Perinatal arrhythmias: diagnosis and management". Clin Perinatol. 34 (4): 627–52, vii–viii. doi:10.1016/j.clp.2007.10.002. PMC 3310372. PMID 18063110.
- ↑ Rao AL, Salerno JC, Asif IM, Drezner JA (July 2014). "Evaluation and management of wolff-Parkinson-white in athletes". Sports Health. 6 (4): 326–32. doi:10.1177/1941738113509059. PMC 4065555. PMID 24982705.
- ↑ Rosner MH, Brady WJ, Kefer MP, Martin ML (November 1999). "Electrocardiography in the patient with the Wolff-Parkinson-White syndrome: diagnostic and initial therapeutic issues". Am J Emerg Med. 17 (7): 705–14. doi:10.1016/s0735-6757(99)90167-5. PMID 10597097.
- ↑ 34.0 34.1 Di Biase L, Gianni C, Bagliani G, Padeletti L (2017). "Arrhythmias Involving the Atrioventricular Junction". Card Electrophysiol Clin. 9 (3): 435–452. doi:10.1016/j.ccep.2017.05.004. PMID 28838549.
- ↑ Cools E, Missant C (2014). "Junctional ectopic tachycardia after congenital heart surgery". Acta Anaesthesiol Belg. 65 (1): 1–8. PMID 24988822.
- ↑ Di Biase L, Gianni C, Bagliani G, Padeletti L (2017). "Arrhythmias Involving the Atrioventricular Junction". Card Electrophysiol Clin. 9 (3): 435–452. doi:10.1016/j.ccep.2017.05.004. PMID 28838549.
- ↑ Trappe HJ (2010). "Tachyarrhythmias, bradyarrhythmias and acute coronary syndromes". J Emerg Trauma Shock. 3 (2): 137–42. doi:10.4103/0974-2700.62112. PMC 2884444. PMID 20606790.
- ↑ Antman EM, Wenger TL, Butler VP, Haber E, Smith TW (1990). "Treatment of 150 cases of life-threatening digitalis intoxication with digoxin-specific Fab antibody fragments. Final report of a multicenter study". Circulation. 81 (6): 1744–52. doi:10.1161/01.cir.81.6.1744. PMID 2188752.
- ↑ Kelly RA, Smith TW (1992). "Recognition and management of digitalis toxicity". Am J Cardiol. 69 (18): 108G–118G, disc. 118G-119G. doi:10.1016/0002-9149(92)91259-7. PMID 1626485.
- ↑ Tuohy S, Saliba W, Pai M, Tchou P (2018). "Catheter ablation as a treatment of atrioventricular block". Heart Rhythm. 15 (1): 90–96. doi:10.1016/j.hrthm.2017.08.015. PMID 28823599.
- ↑ Dobrzynski H, Boyett MR, Anderson RH (2007). "New insights into pacemaker activity: promoting understanding of sick sinus syndrome". Circulation. 115 (14): 1921–32. doi:10.1161/CIRCULATIONAHA.106.616011. PMID 17420362.