Human papillomavirus causes
Jump to navigation
Jump to search
|
Human papillomavirus Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Human papillomavirus causes On the Web |
|
American Roentgen Ray Society Images of Human papillomavirus causes |
|
Risk calculators and risk factors for Human papillomavirus causes |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Seyedmahdi Pahlavani, M.D. [2]
Overview
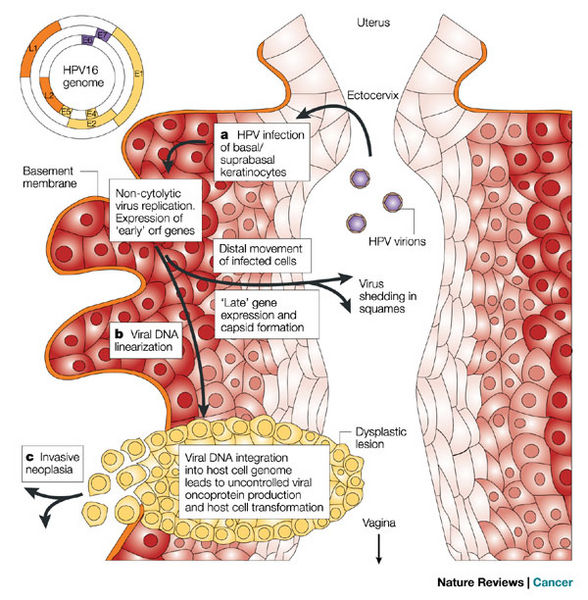
HPV is a double-stranded DNA, non-enveloped capsid virus. Currently, 210 subtypes of this virus have been recognized. It may cause cutaneous or mucosal lesions. Some types have strong relation to cervical cancer and some types are found in benign skin lesion.
Causes
- Human papillomavirus (HPV) is a DNA virus belonging to its own family, papillomaviridae. There are 210 types of HPV and as reflected in its name, species specific for humans. It is a double-stranded DNA, non-enveloped capsid virus that has 7900 base pairs which have 90% homology between the types.
- The base pairs are arranged in a circle which includes the codes for two key proteins known as L1 and L2.
- These two proteins act as the “immunogene” which is required for self-assembly and the infectivity protein, respectively.[1][2]
-
HPV invasion cycle
- Some types of HPV cause local self-limited infections while others can be differentiated by their predilection towards the development of human cancers. For example, HPV 16 and 18 are most frequently associated with cervical cancer.
- HPV 16 accounts for up to 50% of HPV causing cervical and anal cancers worldwide.[3] In addition to those viruses associated with penile cancer, 70% are of the HPV 16 phenotype and occurs 6 times higher in males with histories of venereal warts or condylomata acuminata.
References
- ↑ Roden RB, Yutzy WH, Fallon R, Inglis S, Lowy DR, Schiller JT (2000). "Minor capsid protein of human genital papillomaviruses contains subdominant, cross-neutralizing epitopes". Virology. 270 (2): 254–7. doi:10.1006/viro.2000.0272. PMID 10792983.
- ↑ Doorbar J (2005). "The papillomavirus life cycle". J. Clin. Virol. 32 Suppl 1: S7–15. doi:10.1016/j.jcv.2004.12.006. PMID 15753007.
- ↑ Zaki SR, Judd R, Coffield LM, Greer P, Rolston F, Evatt BL (1992). "Human papillomavirus infection and anal carcinoma. Retrospective analysis by in situ hybridization and the polymerase chain reaction". Am. J. Pathol. 140 (6): 1345–55. PMC 1886536. PMID 1318640.