Hospital-acquired pneumonia natural history, complications, and prognosis
|
Hospital-acquired pneumonia Microchapters |
|
Differentiating Hospital-Acquired Pneumonia from other Diseases |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Hospital-acquired pneumonia natural history, complications, and prognosis On the Web |
|
American Roentgen Ray Society Images of Hospital-acquired pneumonia natural history, complications, and prognosis |
|
FDA on Hospital-acquired pneumonia natural history, complications, and prognosis |
|
CDC onHospital-acquired pneumonia natural history, complications, and prognosis |
|
Hospital-acquired pneumonia natural history, complications, and prognosis in the news |
|
Blogs on Hospital-acquired pneumonia natural history, complications, and prognosis |
|
Directions to Hospitals Treating Hospital-acquired pneumonia |
Editor(s)-in-Chief: C. Michael Gibson, M.S., M.D. ; Philip Marcus, M.D., M.P.H.
Overview
The natural history of HAP depends on many factors and occurs 48 hours or more after hospitalization. Complications include sepsis, respiratory failure, pleural effusion, empyema, and lung abscess. Healthcare-associated pneumonia seems to have fatality rates similar to hospital-acquired pneumonia, worse than community-acquired pneumonia but less severe than pneumonia in ventilated patients. Besides clinical markers like tachypnea (fast breathing) or a high white cell count (leukocytosis), the prognosis seems to be influenced by the underlying associated diseases (comorbidities) and functional capacities.[1][2][3] Many patients have a decreased health condition after the episode.[4]
Natural History
- The natural course of hospital-acquired pneumonia will depend on several factors, such as the causative pathogen, the host immune status and the choice of antibiotic therapy.
- By definition, hospital-acquired pneumonia occurs 48 hours or more since hospital admission; and ventilator-associated pneumonia occurs 48 to 72 hours after the patient was intubated. [5]
- Physicians should suspect of hospital-acquired pneumonia in hospitalized patients that develop fever (> 38° C), productive cough and/or leukocytosis associated with a new chest X-ray infiltration.
- Empirical antibiotic therapy should be started in case of high suspicion, as it has shown improvement of patient survival.
Complications
Despite appropriate antibiotic therapy, severe complications can result from HAP, including:
Sepsis
- Sepsis can occur when microorganisms enter the blood stream and the immune system responds.
- Sepsis most often occurs with bacterial pneumonia
- Streptococcus pneumoniae is the most common cause.
- Individuals with sepsis require hospitalization in an intensive care unit. They often require medications and intravenous fluids to keep their blood pressure from going too low. Sepsis can cause liver, kidney, and heart damage among other things.
Respiratory Failure
- If enough of the lung is involved, it may not be possible for a person to breathe enough to live without support.
- Non-invasive machines such as a bilevel positive airway pressure machine may be used.
- Otherwise, placement of a breathing tube into the mouth may be necessary and a ventilator may be used to help the person breathe.
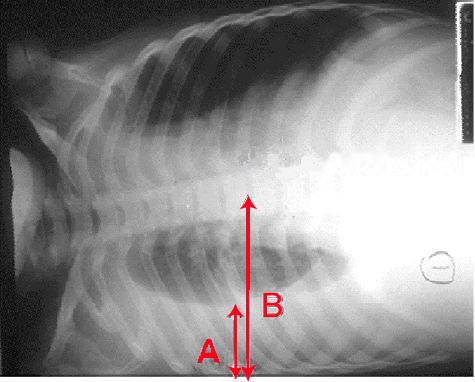
Pleural Effusion and Empyema
- Occasionally, microorganisms from the lung will cause fluid to form in the space surrounding the lung, called the pleural cavity.
- If the microorganisms themselves are present, the fluid collection is often called an empyema.
- If pleural fluid is present in a person with CAP, the fluid should be collected with a needle (thoracentesis) and examined.
- Depending on the result of the examination, complete drainage of the fluid may be necessary, often with a chest tube. If the fluid is not drained, bacteria can continue to cause illness because antibiotics do not penetrate well into the pleural cavity.
Abscess
- Rarely, microorganisms in the lung will form a pocket of fluid and bacteria called an abscess.
- Abscesses can be seen on an x-ray as a cavity within the lung. Abscesses typically occur in aspiration pneumonia and most often contain a mixture of anaerobic bacteria.
- Usually antibiotics are able to fully treat abscesses, but sometimes they must be drained by a surgeon or radiologist.
Prognosis
With treatment, most types of bacterial pneumonia can be cured within one to two weeks. Viral pneumonia may last longer, and mycoplasmal pneumonia may take four to six weeks to resolve completely. The eventual outcome of an episode of pneumonia depends on how ill the person is when he or she is first diagnosed.
In the United States, about one of every twenty people with pneumococcal pneumonia will die.[6] In cases where the pneumonia progresses to blood poisoning (bacteremia), one of every five will die. The death rate (or mortality) also depends on the underlying cause of the pneumonia. Pneumonia caused by Mycoplasma, for instance, is associated with little mortality. However, about half of the people who develop methicillin-resistantStaphylococcus aureus (MRSA) pneumonia while on a ventilator will die.[7] In regions of the world without advanced health care systems, pneumonia is even deadlier.
- Fever typically responds in the first two days of therapy and other symptoms resolve in the first week.
- The x-ray, however, may remain abnormal for at least a month, even when HAP has been successfully treated.
- When HAP does not respond as expected, there are several possible causes.
- A complication of HAP may have occurred or a previously unknown health problem may be playing a role.
- Additional causes include inappropriate antibiotics for the causative organism (ie DRSP), a previously unsuspected microorganism (such as tuberculosis), or a condition which mimics HAP (such as Wegener's granulomatosis).
- Additional testing may be performed and may include additional radiologic imaging (such as a computed tomography scan) or a procedure such as a bronchoscopy or lung biopsy.
Clinical Prediction Rules
Clinical prediction rules have been developed to more objectively prognosticate outcomes in Hospital-acquired pneumonia. Pneumonia severity index[8] -online calculator
- CURB-65 score, which takes into account the severity of symptoms, any underlying diseases, and age[9] -online calculator
References
- ↑ Mehr DR, Zweig SC, Kruse RL; et al. (October 1998). "Mortality from lower respiratory infection in nursing home residents. A pilot prospective community-based study". J Fam Pract. 47 (4): 298–304. PMID 9789516.
- ↑ Mehr DR, Binder EF, Kruse RL; et al. (November 2001). "Predicting mortality in nursing home residents with lower respiratory tract infection: The Missouri LRI Study". JAMA. 286 (19): 2427–36. doi:10.1001/jama.286.19.2427. PMID 11712938.
- ↑ Naughton BJ, Mylotte JM, Tayara A (October 2000). "Outcome of nursing home-acquired pneumonia: derivation and application of a practical model to predict 30 day mortality". J Am Geriatr Soc. 48 (10): 1292–9. PMID 11037018.
- ↑ Fried TR, Gillick MR, Lipsitz LA (March 1997). "Short-term functional outcomes of long-term care residents with pneumonia treated with and without hospital transfer". J Am Geriatr Soc. 45 (3): 302–6. PMID 9063275.
- ↑ "http://www.idsociety.org/uploadedFiles/IDSA/Guidelines-Patient_Care/PDF_Library/HAP.pdf" (PDF). External link in
|title=(help) - ↑ http://www.kidshealth.org/parent/infections/bacterial_viral/pneumonia.html
- ↑ Combes A, Luyt CE, Fagon JY, Wollf M, Trouillet JL, Gibert C, Chastre J; PNEUMA Trial Group. Impact of methicillin resistance on outcome of Staphylococcus aureus ventilator-associated pneumonia. Am J Respir Crit Care Med. 2004 Oct 1;170(7):786-92. PMID 15242840
- ↑ Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, Coley CM, Marrie TJ, Kapoor WN. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997 Jan 23;336(4):243–250. PMID 8995086
- ↑ Lim WS, van der Eerden MM, Laing R; et al. (2003). "Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study". Thorax. 58 (5): 377–82. PMID 12728155.