Helicobacter
| Helicobacter | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
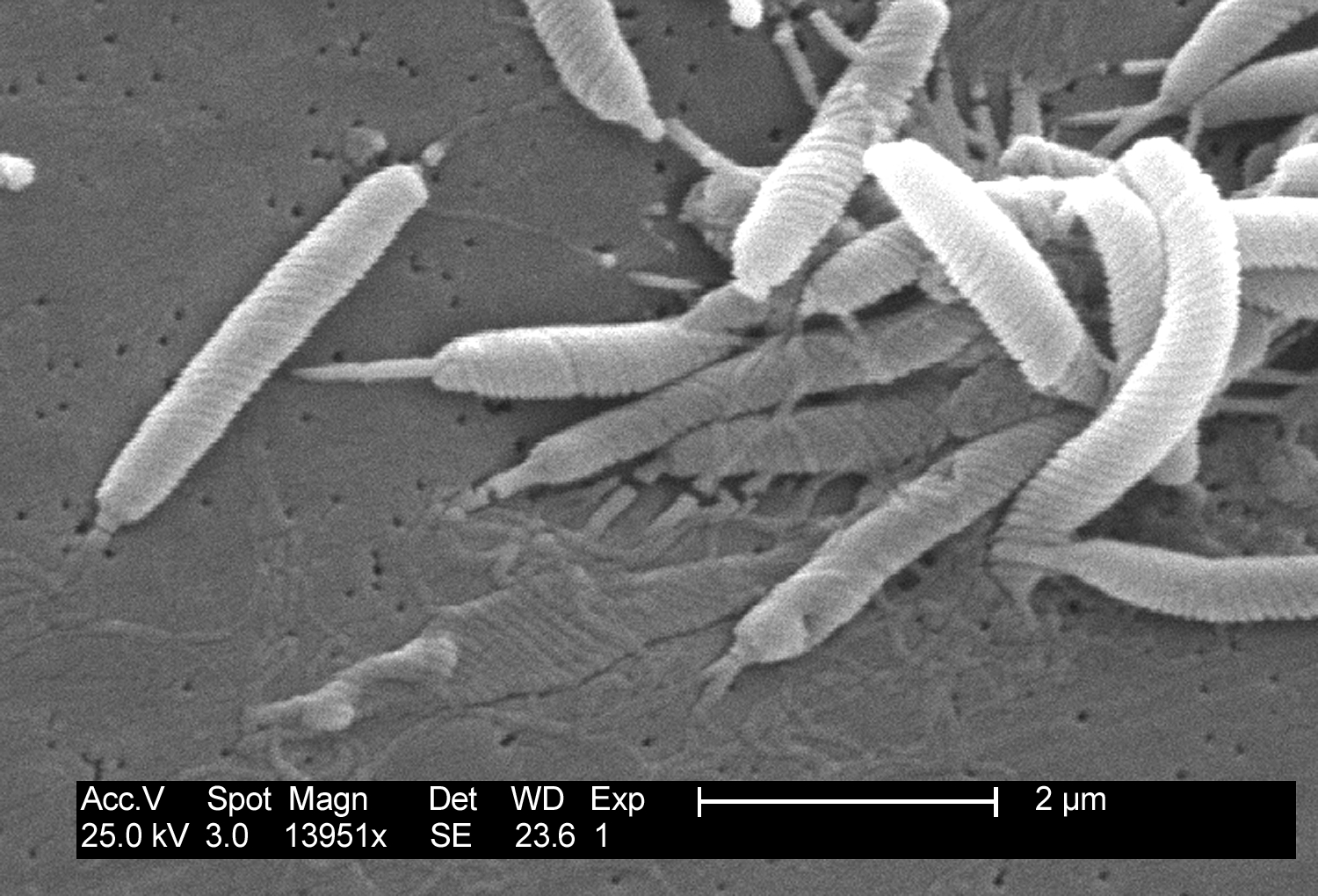 Scanning electron micrograph of Helicobacter bacteria.
| ||||||||||||
| Scientific classification | ||||||||||||
| ||||||||||||
| Species | ||||||||||||
|
H. acinonychis |
|
WikiDoc Resources for Helicobacter |
|
Articles |
|---|
|
Most recent articles on Helicobacter Most cited articles on Helicobacter |
|
Media |
|
Powerpoint slides on Helicobacter |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Helicobacter at Clinical Trials.gov Clinical Trials on Helicobacter at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Helicobacter
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Helicobacter Discussion groups on Helicobacter Patient Handouts on Helicobacter Directions to Hospitals Treating Helicobacter Risk calculators and risk factors for Helicobacter
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Helicobacter |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Overview
Helicobacter is a genus of Gram-negative bacteria possessing a characteristic helix shape. They were initially considered to be members of the Campylobacter genus, but since 1989 they have been grouped in their own genus.[1][2][3]
Some species have been found living in the lining of the upper gastrointestinal tract, as well as the liver of mammals and some birds.[4]. The most widely known species of the genus is H. pylori which infects up to 50% of the human population.[3] Some strains of this bacterium are pathogenic to humans as it is strongly associated with peptic ulcers, chronic gastritis, duodenitis, and stomach cancer. It also serves as the type species of the genus.
Helicobacter spp. are able to thrive in the very acidic mammalian stomach by producing large quantities of the enzyme urease, which locally raises the pH from ~2 to a more biocompatible range of 6 to 7.[5] Bacteria belonging to this genus are usually susceptible to antibiotics such as penicillin, are microaerophilic (require small amounts of oxygen), and are fast-moving with their flagella.[6][7]
Helicobacter Facts.[8]
Curved cells discovered in 1979 in stomach biopsied specimens.
Causes 90% of stomach & duodenal ulcers.
People with type O blood have a 1.5-2X higher rate of ulcers.
Produces large amounts of urease.
Infection common especially in lower socioeconomic class/developing nations.
Humans primary reservoir.
Person-to-person spread via fecal-oral route.
Ubiquitous, no seasonal incidence.
Diseases
In 1994, the World Health Organization’s International Agency for Research on Cancer (IARC) classified H. pylori as a Group 1 carcinogen. This decision was based on the results of numerous studies that confirmed the association between H. pylori infection and gastric adenocarcinoma. H. pylori infection also significantly increases the risk of gastric lymphoma of mucosa-associated lymphoid tissue (MALT) (Suerbaum, 2002).
While H. pylori remains the most medically important bacterial inhabitant of the human stomach, other species of the genus Helicobacter have been identified in other mammals and some birds, and some of these can infect humans.[9] Helicobacter species have also been found to infect the livers of certain mammals and to cause liver disease.[10]
Diagnosis
H. pylori infection can be confirmed by invasive or noninvasive methods. Invasive tests require upper esophagogastroduodenal (EGD) endoscopy, which is considered the reference method of diagnosis. During endoscopy, biopsy specimens of the stomach and duodenum are obtained, and the diagnosis of H. pylori can be made by urease testing, histology and/or culture. If possible, noninvasive testing is done before tissue testing.
H. pylori stool antigen (HpSA) testing is based on monoclonal antibody immunochromatography of stool samples. This testing method identifies active infection and can be used to detect eradication after treatment. A sensitivity and specificity range of 92–98% is reported in the literature for stool antigen testing.
Serological assays (blood serum) measure specific H. pylori immunoglobulin G (IgG) antibodies that can determine if an individual has been infected. The sensitivity and specificity of these assays range from 80–95%, depending on the assay used. Serological testing has been the mainstay of H. pylori diagnosis, particularly in primary care, due to the accessibility, rapid results and low cost of this testing method.
Urease test, Urease Breath Test (UBT) (positive in as little as 2 hours) [11]
Treatment
Therapy with tetracycline, metronidazole, bismuth (Peptobismol)
References
- ↑ Goodwin CS, Armstrong JA, Chilvers T; et al. (1989). "Transfer of Campylobacter pylori and Campylobacter mustelae to Helicobacter gen. nov. as Helicobacter pylori comb. nov. and Helicobacter mustelae comb. nov., respectively". Int. J. Syst. Bacteriol. 39: 397&ndash, 405.
- ↑ Vandamme P, Falsen E, Rossaq R; et al. (1991). "Revision of Campylobacter, Helicobacter, and Wolinella taxonomy: emendation of generic descriptions and proposal of Arcobacter gen. nov". Int. J. Syst. Bacteriol. 41: 88&ndash, 103.
- ↑ 3.0 3.1 Yamaoka Y (editor). (2008). Helicobacter pylori: Molecular Genetics and Cellular Biology. Caister Academic Press. ISBN 978-1-904455-31-8 .
- ↑ Ryan KJ, Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed. ed.). McGraw Hill. ISBN 0-8385-8529-9.
- ↑ Dunn BE, Cohen H, Blaser MJ (1997). "Helicobacter pylori". Clin Microbiol Rev. 10: 720&ndash, 741.
- ↑ Hua JS, Zheng PY, Ho B (1999). "Species differentiation and identification in the genus of Helicobacter" (PDF). World Journal of Gastroenterology. 5 (1): 7&ndash, 9.
- ↑ Rust; et al. (2008). "Helicobacter Flagella, Motility and Chemotaxis". Helicobacter pylori: Molecular Genetics and Cellular Biology (Yamaoka Y, ed.). Caister Academic Press. ISBN 978-1-904455-31-8 .
- ↑ Kathleen Park Talaro (2006). Foundations in Microbiology (6th ed. ed.). McGraw Hill. ISBN 0072994959.
- ↑ Stuart L. Hazell; Mobley, Harry L. T.; George L. Mendz (2001). Helicobacter pylori: Physiology and Genetics. American Society Microbiology. ISBN 1-55581-213-9.
- ↑ Starzyñska T, Malfertheiner P (2006). "Helicobacter and digestive malignancies". Helicobacter. 11 Suppl 1: 32–5. doi:10.1111/j.1478-405X.2006.00431.x. PMID 16925609. Unknown parameter
|month=ignored (help) - ↑ Robert P H Logan, Marjorie M Walker (2001). "Epidemiology and diagnosis of Helicobacter pylori infection ". BMJ 2001;323:920-922 ( 20 October ). 323: &ndash, 741. doi:10.1136/bmj.323.7318.920. PMID 11668141.