Ganaxolone
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Edzel Lorraine Co, DMD, MD[2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Ganaxolone is a neuroactive steroid gamma-aminobutyric acid (GABA) A receptor positive modulator that is FDA approved for the treatment of seizures associated with cyclin-dependent kinase-like 5 (CDKL5) deficiency disorder (CDD) in patients 2 years of age and older. Common adverse reactions include somnolence, pyrexia, salivary hypersecretion, and seasonal allergy.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
ZTALMY is administered by mouth three times daily and must be taken with food.
The recommended titration schedule and maintenance dosage are based on body weight for patients weighing 28 kg or less. Dosage should be increased based on tolerability no more frequently than every 7 days
Off-Label Use and Dosage (Adult)
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Ganaxolone FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Contraindications
None.
Warnings
- Somnolence and Sedation
- ZTALMY can cause somnolence and sedation. In Study 1 , the incidence of somnolence and sedation was 44% in patients treated with ZTALMY, compared with 24% in patients receiving placebo. Somnolence and sedation appeared early during treatment and were generally dose-related.
- Other central nervous system (CNS) depressants, including opioids, antidepressants, and alcohol, could potentiate somnolence and sedation in patients receiving ZTALMY [see Clinical Pharmacology (12.3)]. Prescribers should monitor patients for somnolence and sedation, and advise patients not to drive or operate machinery until they have gained sufficient experience on ZTALMY to gauge whether it adversely affects their ability to drive or operate machinery.
- Suicidal Behavior and Ideation
- Antiepileptic drugs (AEDs), including ZTALMY, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with an AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, or any unusual changes in mood or behavior.
- Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs, that did not include ZTALMY, showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were 4 suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
- The increased risk of suicidal thoughts or behavior with AEDs was observed as early as 1 week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
- The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5–100 years) in the clinical trials analyzed. Table 5 shows absolute and relative risk by indication for all evaluated AEDs.
- Withdrawal of Antiepileptic Drugs
- As with most AEDs, ZTALMY should be withdrawn gradually because of the risk of increased seizure frequency and status epilepticus. If withdrawal is needed because of a serious adverse event, rapid discontinuation can be considered.
Adverse Reactions
Clinical Trials Experience
- Somnolence and Sedation
- Suicidal Behavior and Ideation
- Withdrawal of Antiepileptic Drugs
Postmarketing Experience
There is limited information regarding Ganaxolone Postmarketing Experience in the drug label.
Drug Interactions
- Effect of Strong or Moderate Cytochrome P450 Inducers on ZTALMY
- Co-administration of ZTALMY with CYP450 inducers, such as strong or moderate CYP3A4 inducers, will decrease ganaxolone exposure, which can lower the efficacy of ZTALMY.
- It is recommended to avoid concomitant use of strong or moderate CYP3A4 inducers with ZTALMY. When concomitant use of strong or moderate CYP3A4 inducers is unavoidable, consider an increase in the dosage of ZTALMY; however, do not exceed the maximum daily dosage of ZTALMY.
- In patients on a stable ZTALMY dosage who are initiating or increasing the dosages of enzyme-inducing antiepileptic drugs (e.g., carbamazepine, phenytoin, phenobarbital, and primidone), the ZTALMY dosage may need to be increased; however, do not exceed the maximum daily dosage of ZTALMY.
- Concomitant Use of ZTALMY with CNS Depressants and Alcohol
- Concomitant use of ZTALMY with CNS depressants, including alcohol, may increase the risk of somnolence and sedation.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA):
There is no FDA guidance on usage of Ganaxolone in women who are pregnant.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Ganaxolone in women who are pregnant.
Labor and Delivery
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to antiepileptic drugs (AEDs), such as ZTALMY, during pregnancy. Encourage women who are taking ZTALMY during pregnancy to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry by calling the toll free number 1-888-233-2334 or visiting http://www.aedpregnancyregistry.org/.
Risk Summary
There are no available data on ZTALMY use in pregnant women to inform a drug-associated risk of adverse developmental outcomes. In animal studies, adverse effects on development were observed in mice (fetal malformations) and rats (neurobehavioral and growth impairment) following exposure during organogenesis (mouse) or throughout gestation and lactation (rat) at maternal exposures lower than that in human adults at the maximum recommended human dose (MRHD) of 1800 mg. In addition, neuronal death was observed in rats exposed to ganaxolone during a period of brain development that begins during the third trimester of pregnancy in humans and continues during the first few years after birth.
In the US general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. The background risks of major birth defects and miscarriage for the indicated populations are unknown.
Data
Animal Data
In an embryofetal development study in mice, oral administration of ganaxolone (0, 50, 175, or 300 mg/kg/day) throughout the period of organogenesis resulted in increased incidences of fetal malformations (external and/or visceral) at all doses in the absence of maternal toxicity. Maternal plasma drug exposures (AUC) at the low-effect dose (50 mg/kg/day) for embryofetal developmental toxicity in the mouse were approximately 10-fold lower than that in humans at the MRHD.
In a combined embryofetal development and pre- and postnatal development study in rats, ganaxolone (0, 10, 20, or 40 mg/kg/day) was administered orally to females throughout gestation and lactation. There were no effects on embryofetal growth, survival, or morphology; however, adverse effects on offspring growth (delayed reflex development, decreased body weight gain) were observed during the postnatal period (prior to and after weaning) at the high dose, and neurobehavioral impairment (decreased locomotor activity) was observed in the offspring at the two highest doses. The no-effect dose (10 mg/kg/day) for pre- and postnatal developmental toxicity in rats was associated with maternal drug exposures less than that in humans at the MRHD.
Oral administration of ganaxolone (0, 20, 45, or 90 mg/kg/day) to rats on postnatal day (PND) 7 resulted in widespread apoptotic neurodegeneration in the brain (cortex, thalamus, and hippocampus) at all doses; a no-effect dose was not identified. Brain development on PND 7 in rat corresponds to that beginning in humans during the third trimester of pregnancy and continuing for the first several months to years after birth.
Nursing Mothers
Risk Summary
Ganaxolone is excreted in human milk. Following a single oral dose of ganaxolone (300 mg), ganaxolone exposures (AUC(0-24 h)) in human milk were approximately 4 times higher than those in maternal plasma, resulting in an estimated daily dose in the infant of less than 1% of the maternal dose (see Data). The effects of ganaxolone on milk production and the breastfed infant are unknown.
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for ZTALMY, and any potential adverse effects on the breastfed child from ZTALMY, or from the underlying maternal condition.
Data
A study was conducted in 5 healthy adult lactating women treated with a 300 mg oral dose of ganaxolone. Ganaxolone exposures in breast milk were approximately 4 times those in maternal plasma. The calculated maximum relative infant dose for ganaxolone is approximately 0.157 mg/kg/day based on an average milk intake of 150 mL/kg/day, which is less than 1% of the maternal dose, and approximately 0.24% the labeled pediatric dose of 63 mg/kg/day.
Pediatric Use
The safety and effectiveness of ZTALMY for the treatment of seizures associated with CDD have been established in pediatric patients 2 years of age and older.
The use of ZTALMY for the treatment of seizures associated with CDD in patients 2 years of age and older is supported by a randomized, double-blind, placebo-controlled trial that included 99 pediatric patients 2 to less than 18 years of age.
Safety and effectiveness of ZTALMY in pediatric patients below 2 years of age have not been established.
Juvenile Animal Data
Oral administration of ganaxolone (0, 20, 45, 90/150/250/500 mg/kg/day) to juvenile rats from postnatal day (PND) 7 through PND 91 resulted in deaths associated with sedation and decreased male reproductive organ weights at the mid and high doses, and delayed female sexual maturation and decreased brain weights at all doses. There were no adverse effects on neurobehavioral (locomotor activity, auditory startle response, learning and memory) or reproductive function. A no-effect dose was not established. The lowest dose producing developmental toxicity in juvenile rats (20 mg/kg/day) was associated with plasma drug exposures (AUC) less than that in pediatric patients at the maximum recommended human dose (MRHD) of 1800 mg.
Oral administration of ganaxolone (0, 10, 45, or 90 mg/kg/day) to rats on postnatal day (PND) 7 resulted in widespread neuronal death in multiple brain regions, including cortex, thalamus, and hippocampus, at all doses. The pattern and extent of neuronal death was similar to that produced by intraperitoneal injection of the positive control, the NMDA receptor antagonist MK-801 (1 mg/kg). The hippocampus, in particular, is recognized to have an important role in learning and memory. Effects of ganaxolone and MK-801 on neurobehavioral function were not assessed in this study. Brain development on PND 7 in rat corresponds to that beginning in humans during the third trimester of pregnancy and continuing for the first several months to years after birth. At the lowest-effect dose for neuronal death, plasma drug exposure in the neonatal rat was less than that in pediatric patients at the MRHD.
Geriatic Use
CDD is largely a disease of pediatric and young adult patients. Clinical studies of ZTALMY did not include patients 65 years of age and older.
Gender
There is no FDA guidance on the use of Ganaxolone with respect to specific gender populations.
Race
There is no FDA guidance on the use of Ganaxolone with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Ganaxolone in patients with renal impairment.
Hepatic Impairment
Administration of ZTALMY in patients with severe hepatic impairment (Child-Pugh class C) results in elevated ganaxolone plasma concentrations [see Clinical Pharmacology (12.3)]. Therefore, dosage adjustment in these patients during titration and maintenance is required.
No dosage adjustment is necessary in patients with mild (Child-Pugh class A) or moderate (Child-Pugh class B) hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Ganaxolone in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Ganaxolone in patients who are immunocompromised.
Administration and Monitoring
Administration
There is limited information regarding Ganaxolone Administration in the drug label.
Monitoring
There is limited information regarding Ganaxolone Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Ganaxolone and IV administrations.
Overdosage
There is limited clinical trial experience regarding overdose with ZTALMY. Unintentional overdose has been reported in 1 pediatric patient. This patient received ten times the prescribed dose. The patient was hospitalized for evaluation, including an electrocardiogram (ECG) and blood tests, and recovered.
Patients who overdose should be closely monitored and receive standard supportive care. No specific information is available regarding treatment of overdose. In the event of overdose, a certified poison control center should be contacted for updated information on the management of overdose with ZTALMY.
Pharmacology
Mechanism of Action
The precise mechanism by which ganaxolone exerts its therapeutic effects in the treatment of seizures associated with CDD is unknown, but its anticonvulsant effects are thought to result from positive allosteric modulation of the gamma-aminobutyric acid type A (GABAA) receptor in the CNS.
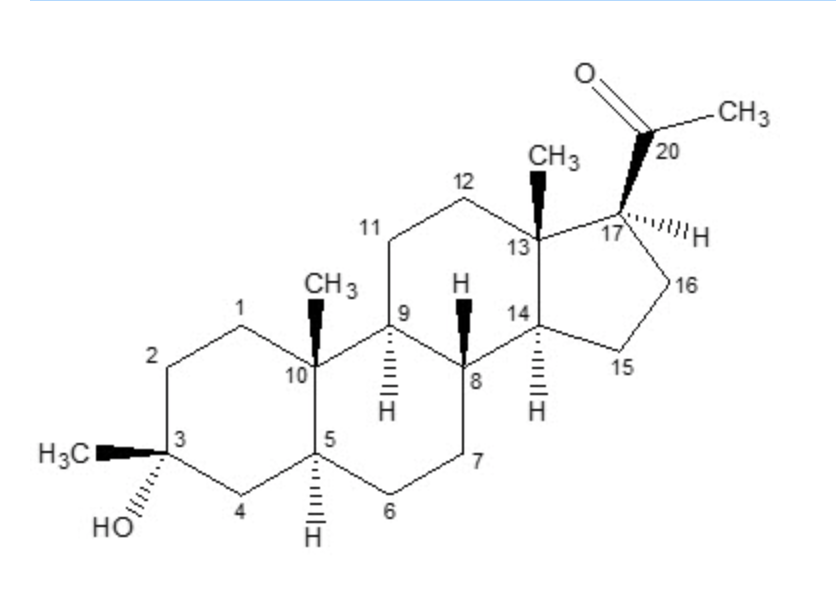
Structure
ZTALMY (ganaxolone) oral suspension contains ganaxolone, a neuroactive steroid gamma-aminobutyric acid A (GABAA) receptor positive modulator. Ganaxolone is a methyl-substituted (at the 3β position) analog of the endogenous neurosteroid allopregnanolone, a derivative of progesterone. Its empirical formula is C22H36O2, and the molecular weight is 332.53 g/mol.
Ganaxolone is a white to off-white crystalline powder that only exists in one crystal form and has low aqueous solubility.
ZTALMY is an oral suspension of ganaxolone. Each mL of oral suspension contains 50 mg of ganaxolone. Inactive ingredients include artificial cherry flavor, citric acid, hypromellose, methylparaben, polyvinyl alcohol, propylparaben, purified water, simethicone emulsion, sodium benzoate, sodium citrate, sodium lauryl sulfate, and sucralose.
Pharmacodynamics
Cardiac Electrophysiology
At therapeutic exposures, ZTALMY does not prolong the QTc interval. QT effects of ZTALMY at high clinical exposure scenarios have not been evaluated.
Pharmacokinetics
Absorption
Following oral administration of ZTALMY, ganaxolone is absorbed with a time to maximum plasma concentration (Tmax) of 2 to 3 hours.
Effect of Food
When ZTALMY was administered with a high-fat meal, the Cmax and AUC increased by 3- and 2-fold, respectively, when compared to administration under fasted conditions. ZTALMY was administered with food in the clinical efficacy study, Study 1 [see Dosage and Administration (2.1)]. The efficacy of ZTALMY when administered in the fasted state is unknown.
Distribution
Ganaxolone is approximately 99% protein-bound in serum.
Elimination
The terminal half-life for ganaxolone is 34 hours.
Metabolism
Ganaxolone is metabolized by CYP3A4/5, CYP2B6, CYP2C19, and CYP2D6.
Excretion
Following a single oral dose of 300 mg [14C]-ganaxolone to healthy male subjects, 55% of the total radioactivity was recovered in feces (2% as unchanged ganaxolone) and 18% of the total radioactivity dose was recovered in urine (undetected as unchanged ganaxolone).
Specific Populations
Age, sex, and race are not expected to have a clinically-relevant effect on ganaxolone pharmacokinetics, after accounting for body weight.
Pediatric Patients
After accounting for body weight, the observed pharmacokinetic exposures in patients in Study 1 [see Clinical Studies (14)] were comparable across the age groups 2 to less than 6 years of age (n=45), 6 to less than 12 years of age (n=28), and 12 to less than 18 years of age (n=16).
Patients with Renal Impairment
Following oral administration of a single 300 mg dose of ZTALMY in subjects with severe renal impairment (creatine clearance between 15 and 30 mL/min as estimated by Cockcroft-Gault formula), the AUC0-INF of ganaxolone decreased 8% and Cmax decreased 11% as compared to that in subjects with normal renal function (creatinine clearance ≥ 90 mL/min as estimated by Cockcroft-Gault formula). The changes in ganaxolone exposures when administered in patients with impaired renal function (creatinine clearance <90 mL/min) are not expected to be clinically significant.
Patients with Hepatic Impairment
The influence of hepatic impairment on the pharmacokinetics of ganaxolone was studied following a single oral dose of ZTALMY 300 mg. In subjects with mild hepatic impairment (Child-Pugh class A), Cmax and AUClast increased by 38% and 8%, respectively, compared to subjects with normal hepatic function. In subjects with moderate hepatic impairment (Child-Pugh class B), Cmax and AUClast increased by 45% and 50%, respectively, compared to subjects with normal hepatic function. In subjects with severe hepatic impairment (Child-Pugh class C), Cmax and AUClast increased by 148% and 269%, respectively, compared to subjects with normal hepatic function [see Dosage and Administration (2.3) and Use in Specific Populations (8.6)].
Drug Interaction Studies
In Vitro Studies
Enzymes
Ganaxolone is not an inhibitor of CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, or CYP3A4/5 at clinically relevant concentrations. Ganaxolone is not an inducer of CYP1A2, CYP2B6, or CYP3A4/5 at clinically relevant concentrations.
Transporters
Ganaxolone does not inhibit BCRP, P-gp, MATE1, MATE2-K, OAT1, OAT3, OCT1, OCT2, OATP1B1, OATP1B3, or BSEP at clinically relevant concentrations. Ganaxolone is not a substrate of BCRP, P-gp, OCT1, OCT2, OATP1B1, or OATP1B3 at clinically relevant concentrations.
In Vivo Studies
CYP3A4 Inducers
Coadministration of ZTALMY with rifampin, a strong inducer of CYP2C19 and CYP3A4, and a moderate inducer of CYP2B6, decreased the ganaxolone Cmax and AUC by 57% and 68%, respectively, in healthy subjects [see Drug Interactions (7.1)]. No dedicated drug-interaction studies were conducted with moderate or weak CYP3A4 inducers.
CYP3A4 Inhibitors
Coadministration of ZTALMY with itraconazole, a strong CYP3A4 inhibitor, increased the ganaxolone AUC by 17% in healthy subjects (the Cmax was unchanged). The changes in ganaxolone exposures when coadministered with strong, moderate, or weak CYP3A4 inhibitors are not expected to be clinically significant.
CYP3A4 substrates
Coadministration of ganaxolone at steady state (400 mg twice daily; 0.44 times the maximum recommended dosage) with midazolam, a sensitive CYP3A4 substrate, did not result in clinically relevant changes in exposures of the substrate in healthy subjects.
Nonclinical Toxicology
Carcinogenesis
No carcinogenicity studies have been conducted with ganaxolone.
Mutagenesis
Ganaxolone was negative for genotoxicity in in vitro (Ames and mouse lymphoma) and in vivo (rat bone marrow micronucleus) assays. The major circulating human metabolite, oxy-dehydro-ganaxolone, was negative for mutagenicity in the in vitro Ames assay but positive for clastogenicity in an in vitro mammalian chromosomal aberration test in human peripheral blood lymphocytes.
Impairment of Fertility
Oral administration of ganaxolone (0, 10, 20 or 40 mg/kg/day) to male and female rats prior to and throughout mating and continuing in females during early gestation resulted in alterations in estrous cyclicity at the high dose. There were no effects on spermatogenesis, reproductive performance and fertility, or early embryonic development. The highest dose tested (40 mg/kg/day) was associated with plasma exposures (AUC) less than that in adult humans at the maximum recommended human dose of 1800 mg.
Clinical Studies
The effectiveness of ZTALMY for the treatment of seizures associated with CDD in patients 2 years of age and older was established in a single, double-blind, randomized, placebo-controlled study in patients 2 to 19 years of age (Study 1, NCT03572933).
Patients enrolled in Study 1 (N=50 for ZTALMY; N=51 for placebo) had molecular confirmation of a pathogenic or likely pathogenic mutation in the CDKL5 gene, seizures inadequately controlled by at least 2 previous treatment regimens, and a minimum of 16 major motor seizures (i.e., bilateral tonic, generalized tonic-clonic, bilateral clonic, atonic, focal to bilateral tonic-clonic) per 28 days during a retrospective 2-month period prior to screening.
Patients were randomized in a 1:1 ratio to receive either ZTALMY or placebo. Following a 21-day titration period, patients in the ZTALMY arm weighing 28 kg or less received a maintenance dosage of 21 mg/kg three times daily (with a maximum daily dose of 1800 mg) while patients in the ZTALMY arm weighing more than 28 kg received a maintenance dosage of 600 mg three times daily.
Ninety-six percent of patients were taking between 1 to 4 concomitant AEDs. The most frequently used concomitant AEDs (in at least 20% of patients) were valproate (34%), levetiracetam (26%), clobazam (25%), and vigabatrin (22%).
The primary efficacy endpoint was the percentage change in the 28-day frequency of major motor seizures (defined similarly as in the 2-month period prior to screening) from a 6-week prospective baseline phase during the 17-week double-blind phase. Patients treated with ZTALMY had a significantly greater reduction in the 28-day frequency of major motor seizures compared to patients receiving placebo.
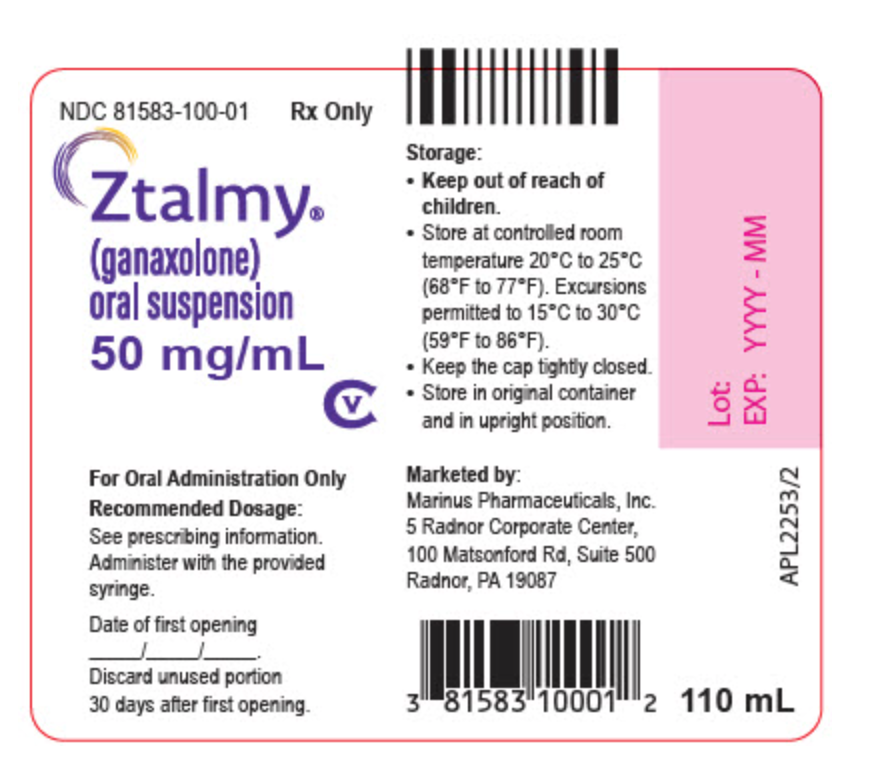
How Supplied
ZTALMY (ganaxolone) oral suspension (50 mg/mL) is a cherry flavored white to off-white suspension supplied in a 4 fl. oz (135 mL) round natural high density polyethylene (HDPE) bottle with a propylene child-resistant cap containing 110 mL of ZTALMY oral suspension.
Storage
Store ZTALMY in its original bottle in an upright position at 20°C to 25°C (68°F to 77°F); excursions permitted from 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature]. Keep the cap tightly closed. Use within 30 days of first opening the bottle, then discard any remainder.
Images
Drug Images
{{#ask: Page Name::Ganaxolone |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
RINCIPAL DISPLAY PANEL - 50 mg/mL Bottle Label NDC 81583-100-01 Rx Only
Ztalmy® (ganaxolone) oral suspension 50 mg/mL
CV
For Oral Administration Only
Recommended Dosage: See prescribing information. Administer with the provided syringe.
Date of first opening _____/_____/_____. Discard unused portion 30 days after first opening.
PRINCIPAL DISPLAY PANEL - 50 mg/mL Bottle Carton - 100-01
Rx Only
NDC 81583-100-01
Ztalmy® (ganaxolone) oral suspension
50 mg/mL
CV
For Oral Administration Only
Read enclosed instructions before using this product. Pharmacist: Dispense the enclosed Medication guide to each patient.
110 mL
{{#ask: Label Page::Ganaxolone |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling.
Somnolence and Sedation
Caution patients about operating hazardous machinery, including motor vehicles, until they are reasonably certain that ZTALMY does not affect them adversely (e.g., impair judgment, thinking, or motor skills).
Suicidal Thinking and Behavior
Counsel patients, their caregivers, and their families that antiepileptic drugs, including ZTALMY, may increase the risk of suicidal thoughts and behavior and advise them to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts of self-harm. Instruct patients, caregivers, and families to report behaviors of concern immediately to healthcare providers.
Withdrawal of Antiepileptic Drugs (AEDs)
Advise patients not to discontinue use of ZTALMY without consulting with their healthcare provider. ZTALMY should normally be gradually withdrawn to reduce the potential for increased seizure frequency and status epilepticus.
Administration information
Advise patients who are prescribed ZTALMY to use the adapter and oral dosing syringes provided by their pharmacist.
Instruct patients to take ZTALMY with food.
Instruct patients to shake ZTALMY thoroughly for at least 1 minute and then wait for 1 minute before measuring and administering each dose.
Instruct patients to discard any unused ZTALMY oral suspension after 30 days of first opening the bottle.
Pregnancy Registry
Advise patients to notify their healthcare provider if they become pregnant or intend to become pregnant during ZTALMY therapy. Encourage women who are taking ZTALMY to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry if they become pregnant. This registry is collecting information about the safety of antiepileptic drugs during pregnancy.
Potential for Abuse
Advise patients that ZTALMY can be abused or lead to dependence.
Precautions with Alcohol
Alcohol-Ganaxolone interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
ZTALMY
Look-Alike Drug Names
There is limited information regarding Ganaxolone Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Page Name=Ganaxolone
|Pill Name=Ganaloxone structure.png
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Page Name=Ganaxolone
|Pill Name=Ganaloxone bottle suspension label 50mg.png
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Page Name=Ganaxolone
|Pill Name=Ganaloxone bottle carton.png
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Page Name=Ganaxolone
|Pill Name=Ganaloxone structure.png
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Page Name=Ganaxolone
|Pill Name=Ganaloxone bottle suspension label 50mg.png
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Page Name=Ganaxolone
|Pill Name=Ganaloxone bottle carton.png
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
 | |
| Clinical data | |
|---|---|
| ATC code |
|
| Legal status | |
| Legal status |
|
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| UNII | |
| KEGG | |
| ChEMBL | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
| Formula | C22H36O2 |
| Molar mass | 332.520 g/mol |
| 3D model (JSmol) | |
| |
| | |
Ganaxolone (INN, also known as CCD-1042) is a steroid drug related to allopregnanolone that has sedative, anxiolytic, and anticonvulsant effects. It is a potent and selective positive allosteric modulator of GABAA receptors.[1] Ganaxolone protects against seizures in diverse animal models, including the 6 Hz and amygdala kindling models.[2][3][4] Unlike for benzodiazepines, there is no tolerance to the anticonvulsant effects of ganaxolone [5]
Ganaxolone is being investigated for potential medical use in the treatment of epilepsy. It is well tolerated in human trials (with exposure of >900 patients), with the main side-effects being sedation, dizziness, and headache.[6] Trials in adults with partial seizures and in infantile spasms have recently been completed.[7][8][9]
See also
References
- ↑ Carter RB, Wood PL, Wieland S, Hawkinson JE, Belelli D, Lambert JJ, White HS, Wolf HH, Mirsadeghi S, Tahir SH, Bolger MB, Lan NC, Gee KW. Characterization of the anticonvulsant properties of ganaxolone (CCD 1042; 3α-hydroxy-3β-methyl-5α-pregnan-20-one), a selective, high-affinity, steroid modulator of the γ-aminobutyric acidA receptor. Journal of Pharmacology and Experimental Therapeutics. 1997 Mar;280(3):1284-95. PMID 9067315
- ↑ Kaminski RM, Livingood MR, Rogawski MA. Allopregnanolone analogs that positively modulate GABA receptors protect against partial seizures induced by 6-Hz electrical stimulation in mice. Epilepsia. 2004 Jul;45(7):864-7. PMID 15230714.
- ↑ Reddy DS, Rogawski MA. Ganaxolone suppression of behavioral and electrographic seizures in the mouse amygdala kindling model. Epilepsy Res. 2010 May;89(2-3):254-60. PMID 20172694.
- ↑ Reddy DS, Rogawski MA. Neurosteroid replacement therapy for catamenial epilepsy. Neurotherapeutics. 2009 Apr;6(2):392-401. PMID 20172694
- ↑ Reddy DS, Rogawski MA. Chronic treatment with the neuroactive steroid ganaxolone in the rat induces anticonvulsant tolerance to diazepam but not to itself. J Pharmacol Exp Ther. 2000 Dec;295(3):1241-8. PMID 11082461
- ↑ Monaghan EP, Navalta LA, Shum L, Ashbrook DW, Lee DA. Initial human experience with ganaxolone, a neuroactive steroid with antiepileptic activity. Epilepsia. 1997 Sep;38(9):1026-31. PMID 9579942
- ↑ Nohria V, Giller E. Ganaxolone. Neurotherapeutics. 2007 Jan;4(1):102-5. PMID 17199022
- ↑ Pieribone VA, Tsai J, Soufflet C, Rey E, Shaw K, Giller E, Dulac O. Clinical evaluation of ganaxolone in pediatric and adolescent patients with refractory epilepsy. Epilepsia. 2007 Oct;48(10):1870-4. PMID 17634060
- ↑ Bialer M, Johannessen SI, Levy RH, Perucca E, Tomson T, White HS. Progress report on new antiepileptic drugs: a summary of the Tenth Eilat Conference (EILAT X). Epilepsy Res. 2010 Dec;92(2-3):89-124. PMID 20970964.
- Pages with script errors
- Pages with broken file links
- Drugs not assigned an ATC code
- Drugs with non-standard legal status
- Articles with changed EBI identifier
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Chemical pages without ChemSpiderID
- Chemical pages without DrugBank identifier
- Articles without InChI source
- Drugboxes which contain changes to verified fields
- Sedatives
- Anticonvulsants
- Neurosteroids
- Alcohols
- Ketones