Etoposide (injection)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Kiran Singh, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Etoposide (injection) is an antineoplastic agent that is FDA approved for the treatment of refractory testicular tumors, small cell lung cancer. Common adverse reactions include nausea, vomiting,hypotension,alopecia, chills, fever, tachycardia, bronchospasm, dyspnea.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
Refractory Testicular Tumors
- Etoposide Injection USP in combination therapy with other approved chemotherapeutic agents in patients with refractory testicular tumors who have already received appropriate surgical, chemotherapeutic, and radiotherapeutic therapy.
Small Cell Lung Cancer
- Etoposide Injection USP in combination with other approved chemotherapeutic agents as first line treatment in patients with small cell lung cancer.
Dosage
Note: Plastic devices made of acrylic or ABS (a polymer composed of acrylonitrile, butadiene, and styrene) have been reported to crack and leak when used with undiluted Etoposide Injection USP.
- The usual dose of Etoposide Injection USP in testicular cancer in combination with other approved chemotherapeutic agents ranges from 50 to 100 mg/m2/day on days 1 through 5 to 100 mg/m2/day on days 1, 3, and 5.
- In small cell lung cancer, the Etoposide Injection USP dose in combination with other approved chemotherapeutic drugs ranges from 35 mg/m2/day for 4 days to 50 mg/m2/day for 5 days.
- For recommended dosing adjustments in patients with renal impairment.
- Chemotherapy courses are repeated at 3- to 4-week intervals after adequate recovery from any toxicity.
- The dosage should be modified to take into account the myelosuppressive effects of other drugs in the combination or the effects of prior X-ray therapy or chemotherapy which may have compromised bone marrow reserve.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Etoposide (injection) in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Etoposide (injection) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Etoposide (injection) in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Etoposide (injection) in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Etoposide (injection) in pediatric patients.
Contraindications
- Etoposide Injection USP is contraindicated in patients who have demonstrated a previous hypersensitivity to etoposide or any component of the formulation.
Warnings
- Patients being treated with etoposide Injection USP must be frequently observed for myelosuppression both during and after therapy. Myelosuppression resulting in death has been reported. Dose-limiting bone marrow suppression is the most significant toxicity associated with etoposide Injection USP therapy. Therefore, the following studies should be obtained at the start of therapy and prior to each subsequent cycle of etoposide Injection USP: platelet count, hemoglobin, white blood cell count, and differential. The occurrence of a platelet count below 50,000/mm3 or an absolute neutrophil count below 500/mm3 is an indication to withhold further therapy until the blood counts have sufficiently recovered.
- Physicians should be aware of the possible occurrence of an anaphylactic reaction manifested by chills, fever, tachycardia, bronchospasm, dyspnea, and hypotension. Higher rates of anaphylactic-like reactions have been reported in children who received infusions at concentrations higher than those recommended. The role that concentration of infusion (or rate of infusion) plays in the development of anaphylactic-like reactions is uncertain.Treatment is symptomatic. The infusion should be terminated immediately, followed by the administration of pressor agents, corticosteroids, antihistamines, or volume expanders at the discretion of the physician. For parenteral administration, etoposide Injection USP should be given only by slow intravenous infusion (usually over a 30- to 60-minute period), since hypotension has been reported as a possible side effect of rapid intravenous injection.
Adverse Reactions
Clinical Trials Experience
The following data on adverse reactions are based on intravenous administration of etoposide Injection USP as a single agent, using several different dose schedules for treatment of a wide variety of malignancies.
Hematologic Toxicity
- Myelosuppression is dose-related and dose-limiting, with granulocyte nadirs occurring 7 to 14 days after drug administration and platelet nadirs occurring 9 to 16 days after drug administration. Bone marrow recovery is usually complete by day 20, and no cumulative toxicity has been reported. Fever and infection have also been reported in patients with neutropenia. Death associated with myelosuppression has been reported.
- The occurrence of acute leukemia with or without a preleukemic phase has been reported rarely in patients treated with etoposide Injection USP in association with other antineoplastic agents.
Gastrointestinal Toxicity
- Nausea and vomiting are the major gastrointestinal toxicities. The severity of such nausea and vomiting is generally mild to moderate with treatment discontinuation required in 1% of patients. Nausea and vomiting can usually be controlled with standard antiemetic therapy. Mild to severe mucositis/esophagitis may occur. Gastrointestinal toxicities are slightly more frequent after oral administration than after intravenous infusion.
Hypotension
- Transient hypotension following rapid intravenous administration has been reported in 1% to 2% of patients. It has not been associated with cardiac toxicity or electrocardiographic changes. No delayed hypotension has been noted. To prevent this rare occurrence, it is recommended that etoposide Injection USP be administered by slow intravenous infusion over a 30 to 60 minute period. If hypotension occurs, it usually responds to cessation of the infusion administration of fluids or other supportive therapy as appropriate. When restarting the infusion, a slower administration rate should be used.
Allergic Reactions
- Anaphylactic-like reactions characterized by chills, fever, tachycardia, bronchospasm, dyspnea, and/or hypotension have been reported to occur in 0.7% to 2% of patients receiving intravenous etoposide Injection USP and in less than 1% of the patients treated with oral capsules. These reactions have usually responded promptly to the cessation of the infusion and administration of pressor agents, corticosteroids, antihistamines, or volume expanders as appropriate; however, the reactions can be fatal. Hypertension and/or flushing have also been reported. Blood pressure usually normalizes within a few hours after cessation of the infusion. Anaphylactic-like reactions have occurred during the initial infusion of etoposide Injection USP.
- Facial/tongue swelling, coughing, diaphoresis, cyanosis, tightness in throat, laryngospasm, back pain, and/or loss of consciousness have sometimes occurred in association with the above reactions. In addition, an apparent hypersensitivity-associated apnea has been reported rarely.
- Rash, urticaria, and/or pruritus have infrequently been reported at recommended doses. At investigational doses, a generalized pruritic erythematous maculopapular rash, consistent with perivasculitis, has been reported.
Alopecia
- Reversible alopecia, sometimes progressing to total baldness was observed in up to 66% of patients.
Other Toxicities
- The following adverse reactions have been infrequently reported: abdominal pain, aftertaste, constipation, dysphagia, asthenia, fatigue, malaise, somnolence, transient cortical blindness, optic neuritis, interstitial pneumonitis/pulmonary fibrosis, fever, seizure (occasionally associated with allergic reactions), Stevens-Johnson syndrome, and toxic epidermal necrolysis, pigmentation, and a single report of radiation recall dermatitis.
- Hepatic toxicity, generally in patients receiving higher doses of the drug than those recommended, has been reported with etoposide Injection USP. Metabolic acidosis has also been reported in patients receiving higher doses.
- Reports of extravasation with swelling have been received postmarketing. Rarely extravasation has been associated with necrosis and venous induration.
- The incidences of adverse reactions in the table that follows are derived from multiple databases from studies in 2,081 patients when etoposide was used either orally or by injection as a single agent.

Postmarketing Experience
There is limited information regarding Postmarketing Experience of Etoposide (injection) in the drug label.
Drug Interactions
There is limited information regarding Etoposide (injection) Drug Interactions in the drug label.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): Teratogenic Effects: Pregnancy Category D
- Etoposide Injection USP can cause fetal harm when administered to a pregnant woman. Etoposide has been shown to be teratogenic in mice and rats.
- In rats, an intravenous etoposide dose of 0.4 mg/kg/day (about 1/20th of the human dose on a mg/m2 basis) during organogenesis caused maternal toxicity, embryotoxicity, and teratogenicity (skeletal abnormalities, exencephaly, encephalocele, and anophthalmia); higher doses of 1.2 and 3.6 mg/kg/day (about 1/7th and 1/2 of human dose on a mg/m2 basis) resulted in 90 and 100% embryonic resorptions. In mice, a single 1 mg/kg (1/16th of human dose on a mg/m2 basis) dose of etoposide administered intraperitoneally on days 6, 7, or 8 of gestation caused embryotoxicity, cranial abnormalities, and major skeletal malformations. An IP dose of 1.5 mg/kg (about 1/10th of human dose on a mg/m2 basis) on day 7 of gestation caused an increase in the incidence of intrauterine death and fetal malformations and a significant decrease in the average fetal body weight.
- Women of childbearing potential should be advised to avoid becoming pregnant. If this drug is used during pregnancy, or if the patient becomes pregnant while receiving this drug, the patient should be apprised of the potential hazard to the fetus.
- Etoposide Injection USP should be considered a potential carcinogen in humans. The occurrence of acute leukemia with or without a preleukemic phase has been reported in rare instances in patients treated with etoposide alone or in association with other neoplastic agents. The risk of development of a preleukemic or leukemic syndrome is unclear. Carcinogenicity tests with etoposide Injection USP have not been conducted in laboratory animals.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Etoposide (injection) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Etoposide (injection) during labor and delivery.
Nursing Mothers
- It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from etoposide Injection USP, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
- Safety and effectiveness in pediatric patients have not been established.
- Etoposide Injection USP contains polysorbate 80. In premature infants, a life-threatening syndrome consisting of liver and renal failure, pulmonary deterioration, thrombocytopenia, and ascites has been associated with an injectable vitamin E product containing polysorbate 80. Anaphylactic reactions have been reported in pediatric patients
Geriatic Use
- Clinical studies of etoposide Injection USP did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Gender
There is no FDA guidance on the use of Etoposide (injection) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Etoposide (injection) with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Etoposide (injection) in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Etoposide (injection) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Etoposide (injection) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Etoposide (injection) in patients who are immunocompromised.
Administration and Monitoring
Administration
- Intravenous
Administration Precautions
As with other potentially toxic compounds, caution should be exercised in handling and preparing the solution of etoposide. Skin reactions associated with accidental exposure to Etoposide Injection USP may occur. The use of gloves is recommended. If etoposide solution contacts the skin or mucosa, immediately and thoroughly wash the skin with soap and water and flush the mucosa with water.
Preparation for Intravenous Administration
Etoposide Injection USP must be diluted prior to use with either 5% Dextrose Injection, or 0.9% Sodium Chloride Injection, to give a final concentration of 0.2 to 0.4 mg/mL. If solutions are prepared at concentrations above 0.4 mg/mL, precipitation may occur. Hypotension following rapid intravenous administration has been reported; hence, it is recommended that the etoposide Injection USP solution be administered over a 30- to 60-minute period. A longer duration of administration may be used if the volume of fluid to be infused is a concern.
Etoposide Injection USP should not be given by rapid intravenous injection.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit.
Stability
Unopened vials of Etoposide Injection USP are stable for 24 months at room temperature (25°C). Vials diluted as recommended to a concentration of 0.2 or 0.4 mg/mL are stable for 96 and 24 hours, respectively, at room temperature (25°C) under normal room fluorescent light in both glass and plastic containers.
Procedures for proper handling and disposal of anticancer drugs should be considered. Several guidelines on this subject have been published.1–7 There is no general agreement that all of the procedures recommended in the guidelines are necessary or appropriate.
Monitoring
There is limited information regarding Monitoring of Etoposide (injection) in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Etoposide (injection) in the drug label.
Overdosage
There is limited information regarding Chronic Overdose of Etoposide (injection) in the drug label.
Pharmacology
Mechanism of Action
There is limited information regarding Mechanism of Action of Etoposide (injection) in the drug label.
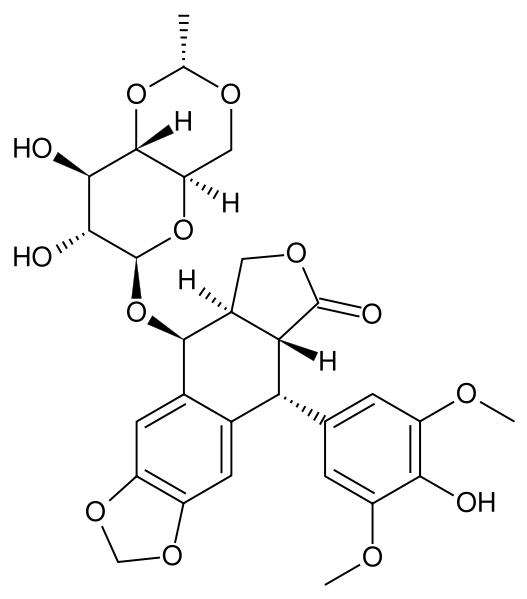
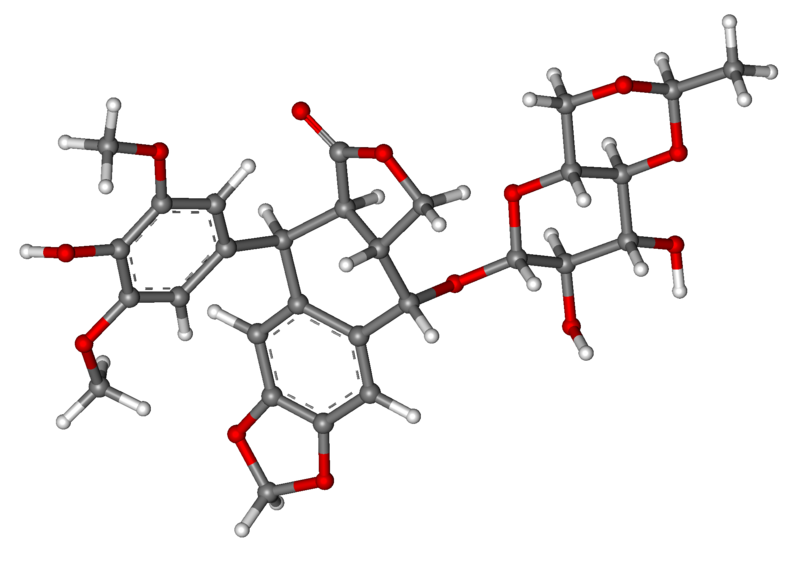
Structure
- Etoposide (also commonly known as VP-16) is a semisynthetic derivative of podophyllotoxin used in the treatment of certain neoplastic diseases. It is 4'-demethylepipodophyllotoxin 9-[4,6-O-(R)-ethylidene-β-D-glucopyranoside]. It is very soluble in methanol and chloroform, slightly soluble in ethanol and sparingly soluble in water and ether. It is made more miscible with water by means of organic solvents. It has a molecular weight of 588.58 and a molecular formula of C29H32O13.
- Etoposide Injection USP is available for intravenous use as 20 mg/mL solution in 100 mg (5 mL), 500 mg (25 mL), and 1 g (50 mL) sterile, multiple-dose vials. The pH of the clear, colorless to pale yellow liquid is 3 to 4. Each mL contains 20 mg etoposide USP, 2 mg anhydrous citric acid, 30 mg benzyl alcohol, 80 mg polysorbate 80/tween 80, 650 mg polyethylene glycol 300, and 30.5 percent (v/v) dehydrated alcohol. Vial head space contains nitrogen.
- The structural formula is:

Pharmacodynamics
There is limited information regarding Pharmacodynamics of Etoposide (injection) in the drug label.
Pharmacokinetics
- On intravenous administration, the disposition of etoposide is best described as a biphasic process with a distribution half-life of about 1.5 hours and terminal elimination half-life ranging from 4 to 11 hours. Total body clearance values range from 33 to 48 mL/min or 16 to 36 mL/min/m2 and, like the terminal elimination half-life, are independent of dose over a range of 100 to 600 mg/m2. Over the same dose range, the areas under the plasma concentration vs. time curves (AUC) and the maximum plasma concentration (Cmax) values increase linearly with dose. Etoposide does not accumulate in the plasma following daily administration of 100 mg/m2 for 4 or 5 days.
- The mean volumes of distribution at steady state fall in the range of 18 to 29 liters or 7 to 17 L/m2. Etoposide enters the CSF poorly. Although it is detectable in CSF and intracerebral tumors, the concentrations are lower than in extracerebral tumors and in plasma. Etoposide concentrations are higher in normal lung than in lung metastases and are similar in primary tumors and normal tissues of the myometrium. In vitro, etoposide is highly protein bound (97%) to human plasma proteins. An inverse relationship between plasma albumin levels and etoposide renal clearance is found in children. In a study determining the effect of other therapeutic agents on the in vitro binding of carbon-14 labeled etoposide to human serum proteins, only phenylbutazone, sodium salicylate, and aspirin displaced protein-bound etoposide at concentrations achieved in vivo.
- Etoposide binding ratio correlates directly with serum albumin in patients with cancer and in normal volunteers. The unbound fraction of etoposide significantly correlated with bilirubin in a population of cancer patients. Data have suggested a significant Inverse correlation between serum albumin concentration and free fraction of etoposide.
- After intravenous administration of 14C-etoposide (100 to 124 mg/m2), mean recovery of radioactivity in the urine was 56% of the dose at 120 hours, 45% of which was excreted as etoposide: fecal recovery of radioactivity was 44% of the dose at 120 hours.
- In children, approximately 55% of the dose is excreted in the urine as etoposide in 24 hours. The mean renal clearance of etoposide is 7 to 10 mL/min/m2 or about 35% of the total body clearance over a dose range of 80 to 600 mg/m2. Etoposide, therefore, is cleared by both renal and nonrenal processes, i.e., metabolism and biliary excretion. The effect of renal disease on plasma etoposide clearance is not known.
- Biliary excretion of unchanged drug and/or metabolites is an important route of etoposide elimination as fecal recovery of radioactivity is 44% of the intravenous dose. The hydroxy acid metabolite [4’-demethylepipodophyllic acid-9-(4,6-O-(R)-ethylidene-β-D-glucopyranoside)], formed by opening of the lactone ring, is found in the urine of adults and children. It is also present in human plasma, presumably as the trans isomer. Glucuronide and/or sulfate conjugates of etoposide are also excreted in human urine. Only 8% or less of an intravenous dose is excreted in the urine as radiolabeled metabolites of 14C-etoposide. In addition, O-demethylation of the dimethoxyphenol ring occurs through the CYP450 3A4 isoenzyme pathway to produce the corresponding catechol.
- After intravenous infusion, the Cmax and AUC values exhibit marked intra- and inter-subject variability.
- There is no evidence of a first-pass effect for etoposide. For example, no correlation exists between the absolute oral bioavailability of etoposide capsules and nonrenal clearance. No evidence exists for any other differences in etoposide metabolism and excretion after administration of oral capsules as compared to intravenous infusion.
- In adults, the total body clearance of etoposide is correlated with creatinine clearance, serum albumin concentration, and nonrenal clearance. Patients with impaired renal function receiving etoposide have exhibited reduced total body clearance, increased AUC and a lower volume of distribution at steady state. Use of cisplatin therapy is associated with reduced total body clearance. In children, elevated serum SGPT levels are associated with reduced drug total body clearance. Prior use of cisplatin may also result in a decrease of etoposide total body clearance in children.
- Although some minor differences in pharmacokinetic parameters between age and gender have been observed, these differences were not considered clinically significant.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Etoposide has been shown to be mutagenic in Ames assay.
- Treatment of Swiss-Albino mice with 1.5 mg/kg IP of etoposide Injection USP on day 7 of gestation increased the incidence of intrauterine death and fetal malformations, as well as significantly decreased the average fetal body weight. Maternal weight gain was not affected.
- Irreversible testicular atrophy was present in rats treated with etoposide intravenously for 30 days at 0.5 mg/kg/day (about 1/16th of the human dose on a mg/m2 basis).
Clinical Studies
There is limited information regarding Clinical Studies of Etoposide (injection) in the drug label.
How Supplied
- Etoposide Injection USP, 20 mg/mL, is supplied as follows:

- 5 mL vials are packed individually per shelf pack with NDC 68001-265-25.
- 25 mL vials are packed individually per shelf pack with NDC 68001-265-26.
- 50 mL vials are packed individually per shelf pack with NDC 68001-265-27.
Storage
Store at 20° to 25°C (68° to 77°F). See USP controlled room temperature.
Images
Drug Images
{{#ask: Page Name::Etoposide (injection) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel



{{#ask: Label Page::Etoposide (injection) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Patient Counseling Information of Etoposide (injection) in the drug label.
Precautions with Alcohol
- Alcohol-Etoposide (injection) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- ETOPOSIDE ®[1]
Look-Alike Drug Names
There is limited information regarding Etoposide (injection) Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Page Name=Etoposide (injection)
|Pill Name=No image.jpg
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Label Page=Etoposide (injection) |Label Name=Etoposide ingredients and appearance.png
}}
{{#subobject:
|Label Page=Etoposide (injection) |Label Name=Etoposide fig02.jpg
}}
{{#subobject:
|Label Page=Etoposide (injection) |Label Name=Etoposide fig01.jpg
}}