Esomeprazole sodium
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2]; Ammu Susheela, M.D. [3]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Esomeprazole sodium is a proton pump inhibitor that is FDA approved for the treatment of gastroesophageal reflux disease (GERD) with erosive esophagitis and risk reduction of rebleeding of gastric or duodenal ulcers following therapeutic endoscopy in adults. Common adverse reactions include injection site reaction, abdominal pain, constipation, diarrhea, flatulence, indigestion, nausea, xerostomia, dizziness, headache.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
General Information
- Esomeprazole sodium for Injection should not be administered concomitantly with any other medications through the same intravenous site and/or tubing. The intravenous line should always be flushed with either 0.9% Sodium Chloride Injection, USP, Lactated Ringer’s Injection, USP or 5% Dextrose Injection, USP both prior to and after administration of esomeprazole sodium for Injection.
- The admixture should be stored at room temperature up to 30°C (86°F) and should be administered within the designated time period as listed in Table 1 below. No refrigeration is required.

- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
- As soon as oral therapy is possible or appropriate, intravenous therapy with esomeprazole sodium for Injection should be discontinued and the therapy should be continued orally.
GERD with Erosive Esophagitis
- Dosing information
- Recommended adult dosage: 20 mg or 40 mg IV injection qd (no less than 3 minutes) or IV infusion (10 minutes to 30 minutes). Safety and efficacy of esomeprazole sodium for injection as a treatment of GERD patients with erosive esophagitis for more than 10 days have not been demonstrated.
- Dosage adjustment is not required in patients with mild to moderate liver impairment (child Pugh Classes A and B). For patients with severe liver impairment (child Pugh Class C),
- Maximum dosage: 20 mg IV qd
Risk Reduction of Rebleeding of Gastric or Duodenal Ulcer following Therapeutic Endoscopy in Adults
- Dosing information
- 80 mg administered as an intravenous infusion over 30 minutes followed by a continuous infusion of 8 mg/h for a total treatment duration of 72 hours (i.e., includes initial 30-minute dose plus 71.5 hours of continuous infusion).
- Intravenous therapy is aimed solely at the acute initial management of bleeding gastric or duodenal ulcers and does not constitute full treatment. Intravenous therapy should be followed by oral acid-suppressive therapy.
- For patients with liver impairment
- No dosage adjustment of the initial esomeprazole 80 mg infusion is necessary.
- For patients with mild to moderate liver impairment (Child Pugh Classes A and B), a maximum continuous infusion of esomeprazole 6 mg/h should not be exceeded.
- For patients with severe liver impairment (Child Pugh Class C), a maximum continuous infusion of 4 mg/h should not be exceeded.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Esomeprazole sodium in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Esomeprazole sodium in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
GERD with Erosive Esophagitis
- Dose should be infused over 10 minutes to 30 minutes.
- 1 year to 17 years:
- Body weight less than 55 kg: 10 mg
- Body weight 55 kg or greater: 20 mg
- 1 month to less than 1 year of age: 0.5 mg/kg
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Esomeprazole sodium in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Esomeprazole sodium in pediatric patients.
Contraindications
Patients with known hypersensitivity to any component of the formulation or to substituted benzimidazoles (angioedema and anaphylaxis have occurred).
Warnings
Risk of Concomitant Gastric Malignancy
- Symptomatic response to therapy with esomeprazole sodium does not preclude the presence of gastric malignancy.
Atrophic Gastritis
- Atrophic gastritis has been noted occasionally in gastric corpus biopsies from patients treated long-term with omeprazole, of which esomeprazole is an enantiomer.
Clostridium difficile Associated Diarrhea
- Published observational studies suggest that PPI therapy like esomeprazole sodium may be associated with an increased risk of Clostridium difficile associated diarrhea, especially in hospitalized patients. This diagnosis should be considered for diarrhea that does not improve.
- Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated.
Interaction with Clopidogrel
- Avoid concomitant use of esomeprazole sodium with clopidogrel. clopidogrel is a prodrug. Inhibition of platelet aggregation by clopidogrel is entirely due to an active metabolite. The metabolism of clopidogrel to its active metabolite can be impaired by use with concomitant medications, such as esomeprazole, that inhibit CYP2C19 activity. Concomitant use of clopidogrel with 40 mg esomeprazole reduces the pharmacological activity of clopidogrel. When using esomeprazole sodium consider alternative anti-platelet therapy.
Bone Fracture
- Several published observational studies suggest that proton pump inhibitor (PPI) therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist, or spine. The risk of fracture was increased in patients who received high-dose, defined as multiple daily doses, and long-term PPI therapy (a year or longer). Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated. Patients at risk for osteoporosis-related fractures should be managed according to established treatment guidelines.
Hypomagnesemia
- Hypomagnesemia, symptomatic and asymptomatic, has been reported rarely in patients treated with PPIs for at least three months, in most cases after a year of therapy. Serious adverse events include tetany, arrhythmias, and seizures. In most patients, treatment of hypomagnesemia required magnesium replacement and discontinuation of the PPI.
- For patients expected to be on prolonged treatment or who take PPIs with medications such as digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), health care professionals may consider monitoring magnesium levels prior to initiation of PPI treatment and periodically.
Concomitant use of NEXIUM with St. John’s Wort or Rifampin
- Drugs which induce CYP2C19 or CYP3A4 (such as St. John’s Wort or rifampin) can substantially decrease esomeprazole concentrations. Avoid concomitant use of NEXIUM with St. John’s Wort or rifampin.
Interactions with Investigations for Neuroendocrine Tumors
- Serum chromogranin A (CgA) levels increase secondary to drug-induced decreases in gastric acidity. The increased CgA level may cause false positive results in diagnostic investigations for neuroendocrine tumors. Healthcare providers should temporarily stop esomeprazole treatment at least 14 days before assessing CgA levels and consider repeating the test if initial CgA levels are high. If serial tests are performed (e.g. for monitoring), the same commercial laboratory should be used for testing, as reference ranges between tests may vary.
Concomitant use of NEXIUM with Methotrexate
- Literature suggests that concomitant use of PPIs with methotrexate may elevate and prolong serum levels of methotrexate and/or its metabolite, possibly leading to methotrexate toxicities. In high-dose methotrexate administration a temporary withdrawal of the PPI may be considered in some patients.
Adverse Reactions
Clinical Trials Experience
Clinical Trials Experience with Intravenous Esomeprazole sodium
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adults
- The safety of intravenous esomeprazole is based on results from clinical trials conducted in four different populations including patients having symptomatic GERD with or without a history of erosive esophagitis (n=199), patients with erosive esophagitis (n=160), healthy subjects (n=204) and patients with bleeding gastric or duodenal ulcers (n=375).
Symptomatic GERD and Erosive Esophagitis Trials
- The data described below reflect exposure to esomeprazole sodium for Injection in 359 patients. Esomeprazole sodium for Injection was studied only in actively-controlled trials. The population was 18 to 77 years of age; 45% Male, 52% Caucasian, 17% Black, 3% Asian, 28% Other, and had either erosive reflux esophagitis (44%) or GERD (56%). Most patients received doses of either 20 or 40 mg either as an infusion or an injection. Adverse reactions occurring in ≥1% of patients treated with intravenous esomeprazole (n=359) in clinical trials are listed below:

- Intravenous treatment with esomeprazole 20 and 40 mg administered as an injection or as an infusion was found to have a safety profile similar to that of oral administration of esomeprazole.
Pediatric
- A randomized, open-label, multi-national study to evaluate the pharmacokinetics of repeated intravenous doses of once daily esomeprazole in pediatric patients 1 month to 17 years old, inclusive was performed. The safety results are consistent with the known safety profile of esomeprazole and no unexpected safety signals were identified.
Risk Reduction of Rebleeding of Gastric or Duodenal Ulcers in Adults
- The data described below reflect exposure to esomeprazole sodium for Injection in 375 patients. Esomeprazole sodium for Injection was studied in a placebo-controlled trial. Patients were randomized to receive esomeprazole sodium for Injection (n=375) or placebo (n=389). The population was 18 to 98 years old; 68% Male, 87% Caucasian, 1% Black, 7% Asian, 4% other, who presented with endoscopically confirmed gastric or duodenal ulcer bleeding. Following endoscopic hemostasis, patients received either 80 mg esomeprazole as an intravenous infusion over 30 minutes followed by a continuous infusion of 8 mg per hour or placebo for a total treatment duration of 72 hours. After the initial 72-hour period, all patients received oral proton pump inhibitor (PPI) for 27 days.

- With the exception of injection site reactions described above, intravenous treatment with esomeprazole administered as an injection or as an infusion was found to have a safety profile similar to that of oral administration of esomeprazole.
Postmarketing Experience
- The following adverse reactions have been identified during post-approval use of esomeprazole sodium. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Postmarketing Reports - There have been spontaneous reports of adverse events with postmarketing use of esomeprazole. These reports occurred rarely and are listed below by body system:
- Blood And Lymphatic System Disorders: agranulocytosis, pancytopenia;
- Eye Disorders: blurred vision;
- Gastrointestinal Disorders: pancreatitis; stomatitis; microscopic colitis;
- Hepatobiliary Disorders: hepatic failure, hepatitis with or without jaundice;
- Immune System Disorders: anaphylactic reaction/shock;
- Infections and Infestations: GI candidiasis;
- Metabolism and nutritional disorders: hypomagnesemia with or without hypocalcemia and/or hypokalemia;
- Musculoskeletal And Connective Tissue Disorders: muscular weakness, myalgia, bone fracture;
- Nervous System Disorders: hepatic encephalopathy, taste disturbance;
- Psychiatric Disorders: aggression, agitation, depression, hallucination;
- Renal and Urinary Disorders: interstitial nephritis;
- Reproductive System and Breast Disorders: gynecomastia;
- Respiratory, Thoracic and Mediastinal Disorders: bronchospasm;
- Skin and Subcutaneous Tissue Disorders: alopecia, erythema multiforme, hyperhidrosis, photosensitivity, Stevens-Johnson syndrome, toxic epidermal necrolysis (TEN, some fatal).
- Other adverse events not observed with NEXIUM, but occurring with omeprazole can be found in the omeprazole package insert.
Drug Interactions
- Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4.
- In vitro and in vivo studies have shown that esomeprazole is not likely to inhibit CYPs 1A2, 2A6, 2C9, 2D6, 2E1 and 3A4. No clinically relevant interactions with drugs metabolized by these CYP enzymes would be expected. Drug interaction studies have shown that esomeprazole does not have any clinically significant interactions with phenytoin, warfarin, quinidine, clarithromycin or amoxicillin.
- Post-marketing reports of changes in prothrombin measures have been received among patients on concomitant warfarin and esomeprazole therapy. Increases in INR and prothrombin time may lead to abnormal bleeding and even death. Patients treated with proton pump inhibitors and warfarin concomitantly may need to be monitored for increases in INR and prothrombin time.
- Esomeprazole may potentially interfere with CYP2C19, the major esomeprazole metabolizing enzyme. Co-administration of esomeprazole 30 mg and diazepam, a CYP2C19 substrate, resulted in a 45% decrease in clearance of diazepam. Increased plasma levels of diazepam were observed 12 hours after dosing and onwards. However, at that time, the plasma levels of diazepam were below the therapeutic interval, and thus this interaction is unlikely to be of clinical relevance.
- Clopidogrel is metabolized to its active metabolite in part by CYP2C19.
- Concomitant use of esomeprazole 40 mg results in reduced plasma concentrations of the active metabolite of clopidogrel and a reduction in platelet inhibition.
- Avoid concomitant administration of esomeprazole sodium with clopidogrel. When using esomeprazole sodium, consider use of alternative anti-platelet therapy.
- Omeprazole acts as an inhibitor of CYP2C19. Omeprazole, given in doses of 40 mg daily for one week to 20 healthy subjects in cross-over study, increased Cmax and AUC of cilostazol by 18% and 26%, respectively. Cmax and AUC of one of its active metabolites, 3,4-dihydro-cilostazol, which has 4-7 times the activity of cilostazol, were increased by 29% and 69%, respectively. Co-administration of cilostazol with esomeprazole is expected to increase concentrations of cilostazol and its above mentioned active metabolite. Therefore, a dose reduction of cilostazol from 100 mg twice daily to 50 mg twice daily should be considered.
- Concomitant administration of esomeprazole and a combined inhibitor of CYP2C19 and CYP3A4, such as voriconazole, may result in more than doubling of the esomeprazole exposure. Dose adjustment of esomeprazole is not normally required for the recommended doses. However, in patients who may require higher doses, dose adjustment may be considered.
- Drugs known to induce CYP2C19 or CYP3A4 (such as rifampin) may lead to decreased esomeprazole serum levels. Omeprazole, of which esomeprazole is an enantiomer, has been reported to interact with St. John’s Wort, an inducer of CYP3A4. In a cross-over study in 12 healthy male subjects, St. John’s Wort (300 mg three times daily for 14 days) significantly decreased the systemic exposure of omeprazole in CYP2C19 poor metabolizers (Cmax and AUC decreased by 37.5% and 37.9%, respectively) and extensive metabolizers (Cmax and AUC decreased by 49.6% and 43.9%, respectively). Avoid concomitant use of St. John’s Wort or rifampin with NEXIUM.
- Co-administration of oral contraceptives, diazepam, phenytoin, or quinidine did not seem to change the pharmacokinetic profile of esomeprazole.
- Concomitant use of atazanavir and proton pump inhibitors is not recommended. * Co-administration of atazanavir with proton pump inhibitors is expected to substantially decrease atazanavir plasma concentrations and thereby reduce its therapeutic effect.
- Omeprazole has been reported to interact with some antiretroviral drugs. The clinical importance and the mechanisms behind these interactions are not always known. Increased gastric pH during omeprazole treatment may change the absorption of the antiretroviral drug. Other possible interaction mechanisms are via CYP2C19.
- For some antiretroviral drugs, such as atazanavir and nelfinavir, decreased serum levels have been reported when given together with omeprazole. Following multiple doses of nelfinavir (1250 mg, twice daily) and omeprazole (40 mg daily), AUC was decreased by 36% and 92%, Cmax by 37% and 89% and Cmin by 39% and 75%, respectively, for nelfinavir and M8. Following multiple doses of atazanavir (400 mg daily) and omeprazole (40 mg daily, 2 hr before atazanavir), AUC was decreased by 94%, Cmax by 96%, and Cmin by 95%. Concomitant administration with omeprazole and drugs such as atazanavir and nelfinavir is therefore not recommended. For other antiretroviral drugs, such as saquinavir, elevated serum levels have been reported with an increase in AUC by 82%, in Cmax by 75% and in Cmin by 106% following multiple dosing of saquinavir/ritonavir (1000/100 mg) twice daily for 15 days with omeprazole 40 mg daily co-administered days 11 to 15. Dose reduction of saquinavir should be considered from the safety perspective for individual patients. There are also some antiretroviral drugs of which unchanged serum levels have been reported when given with omeprazole.
- Studies evaluating concomitant administration of esomeprazole and either naproxen (non-selective NSAID) or rofecoxib (COX-2 selective NSAID) did not identify any clinically relevant changes in the pharmacokinetic profiles of esomeprazole or these NSAIDs.
- Esomeprazole inhibits gastric acid secretion. Therefore, esomeprazole may interfere with the absorption of drugs where gastric pH is an important determinant of bioavailability. Like with other drugs that decrease the intragastric acidity, the absorption of drugs such as ketoconazole, atazanavir, iron salts, and erlotinib can decrease, while the absorption of drugs such as digoxin can increase during treatment with esomeprazole. Concomitant treatment with omeprazole (20 mg daily) and digoxin in healthy subjects increased the bioavailability of digoxin by 10% (30% in two subjects). Esomeprazole is an enantiomer of omeprazole. Coadministration of digoxin with esomeprazole is expected to increase the systemic exposure of digoxin.
- Therefore, patients may need to be monitored when digoxin is taken concomitantly with esomeprazole.
Interactions with Investigations of Neuroendocrine Tumors
- Drug-induced decrease in gastric acidity results in enterochromaffin-like cell hyperplasia and increased Chromogranin A levels which may interfere with investigations for neuroendocrine tumors.
Tacrolimus
- Concomitant administration of esomeprazole and tacrolimus may increase the serum levels of tacrolimus.
Methotrexate
- Case reports, published population pharmacokinetic studies, and retrospective analyses suggest that concomitant administration of PPIs and methotrexate (primarily at high dose; see methotrexate prescribing information) may elevate and prolong serum levels of methotrexate and/or its metabolite hydroxymethotrexate.
- However, no formal drug interaction studies of methotrexate with PPIs have been conducted.
Use in Specific Populations
Pregnancy
Risk Summary
- There are no adequate and well-controlled studies with NEXIUM in pregnant women. Esomeprazole is the s-isomer of omeprazole. Available epidemiologic data fail to demonstrate an increased risk of major congenital malformations or other adverse pregnancy outcomes with first trimester omeprazole use. Teratogenicity was not observed in animal reproduction studies with administration of oral esomeprazole magnesium in rats and rabbits with doses about 57 times and 35 times, respectively, an oral human dose of 40 mg. However, changes in bone morphology were observed in offspring of rats dosed through most of pregnancy and lactation at doses equal to or greater than approximately 33.6 times an oral human dose of 40 mg. Because of the observed effect at high doses of esomeprazole magnesium on developing bone in rat studies, NEXIUM should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Human Data
- Esomeprazole is the S-isomer of omeprazole. Four epidemiological studies compared the frequency of congenital abnormalities among infants born to women who used omeprazole during pregnancy with the frequency of abnormalities among infants of women exposed to H2 receptor antagonists or other controls.
- A population based retrospective cohort epidemiological study from the Swedish Medical Birth Registry, covering approximately 99% of pregnancies, from 1995-99, reported on 955 infants (824 exposed during the first trimester with 39 of these exposed beyond first trimester, and 131 exposed after the first trimester) whose mothers used omeprazole during pregnancy. The number of infants exposed in utero to omeprazole that had any malformation, low birth weight, low Apgar score, or hospitalization was similar to the number observed in this population. The number of infants born with ventricular septal defects and the number of stillborn infants was slightly higher in the omeprazole-exposed infants than the expected number in this population.
- A population-based retrospective cohort study covering all live births in Denmark from 1996-2009, reported on 1,800 live births whose mothers used omeprazole during the first trimester of pregnancy and 837, 317 live births whose mothers did not use any proton pump inhibitor. The overall rate of birth defects in infants born to mothers with first trimester exposure to omeprazole was 2.9% and 2.6% in infants born to mothers not exposed to any proton pump inhibitor during the first trimester.
- A retrospective cohort study reported on 689 pregnant women exposed to either H2 blockers or omeprazole in the first trimester (134 exposed to omeprazole) and 1,572 pregnant women unexposed to either during the first trimester. The overall malformation rate in offspring born to mothers with first trimester exposure to omeprazole, an H2-blocker, or were unexposed was 3.6%, 5.5%, and 4.1% respectively.
- A small prospective observational cohort study followed 113 women exposed to omeprazole during pregnancy (89% first trimester exposures). The reported rate of major congenital malformations was 4% in the omeprazole group, 2% in controls exposed to non-teratogens, and 2.8% in disease paired controls. Rates of spontaneous and elective abortions, preterm deliveries, gestational age at delivery, and mean birth weight were similar among the groups.
- Several studies have reported no apparent adverse short-term effects on the infant when single dose oral or intravenous omeprazole was administered to over 200 pregnant women as premedication for cesarean section under general anesthesia.
Animal Data
- Reproduction studies have been performed with esomeprazole magnesium in rats at oral doses up to 280 mg/kg/day (about 57 times an oral human dose of 40 mg on a body surface area basis) and in rabbits at oral doses up to 86 mg/kg/day (about 35 times the human dose on a body surface area basis) and have revealed no evidence of impaired fertility or harm to the fetus due to esomeprazole magnesium.
- A pre- and postnatal developmental toxicity study in rats with additional endpoints to evaluate bone development was performed with esomeprazole magnesium at oral doses of 14 to 280 mg/kg/day (about 3.4 to 57 times an oral human dose of 40 mg on a body surface area basis). Neonatal/early postnatal (birth to weaning) survival was decreased at doses equal to or greater than 138 mg/kg/day (about 33 times an oral human dose of 40 mg on a body surface area basis). Body weight and body weight gain were reduced and neurobehavioral or general developmental delays in the immediate post-weaning timeframe were evident at doses equal to or greater than 69 mg/kg/day (about 16.8 times an oral human dose of 40 mg on a body surface area basis). In addition, decreased femur length, width and thickness of cortical bone, decreased thickness of the tibial growth plate and minimal to mild bone marrow hypocellularity were noted at doses equal to or greater than 14 mg/kg/day (about 3.4 times an oral human dose of 40 mg on a body surface area basis). Physeal dysplasia in the femur was observed in offspring of rats treated with oral doses of esomeprazole magnesium at doses equal to or greater than 138 mg/kg/day (about 33.6 times an oral human dose of 40 mg on a body surface area basis).
- Effects on maternal bone were observed in pregnant and lactating rats in a pre- and postnatal toxicity study when esomeprazole magnesium was administered at oral doses of 14 to 280 mg/kg/day (about 3.4 to 57 times an oral human dose of 40 mg on a body surface area basis). When rats were dosed from gestational day 7 through weaning on postnatal day 21, a statistically significant decrease in maternal femur weight of up to 14% (as compared to placebo treatment) was observed at doses equal to or greater than 138 mg/kg/day (about 33.6 times an oral human dose of 40 mg on a body surface area basis).
- A pre- and postnatal development study in rats with esomeprazole strontium (using equimolar doses compared to esomeprazole magnesium study) produced similar results in dams and pups as described above.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Esomeprazole sodium in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Esomeprazole sodium during labor and delivery.
Nursing Mothers
- Esomeprazole is likely present in human milk. Esomeprazole is the S-isomer of omeprazole and limited data indicate that maternal doses of omeprazole 20 mg daily produce low levels in human milk. Caution should be exercised when esomeprazole sodium is administered to a nursing woman.
Pediatric Use
- The safety and effectiveness of esomeprazole sodium for Injection have been established in pediatric patients 1 month to 17 years of age for short-term treatment of GERD with erosive esophagitis. However, effectiveness has not been established in patients less than 1 month of age.
1 month to 17 years of age
- Use of esomeprazole sodium for Injection in pediatric patients 1 month to 17 years of age for short-term treatment of GERD with Erosive Esophagitis is supported by: a) results observed from a pharmacokinetic (PK) study on esomeprazole sodium for Injection performed in pediatric patients, b) predictions from a population PK model comparing I.V. PK data between adult and pediatric patients, and c) relationship between exposure and pharmacodynamic results obtained from adult I.V. and pediatric oral data and d) PK results already included in the current approved labeling and from adequate and well-controlled studies that supported the approval of esomeprazole sodium for Injection for adults.
Neonates 0 to 1 month of age
- Following administration of esomeprazole sodium in neonates the geometric mean (range) for CL was 0.17 L/h/kg (0.04 L/h/kg- 0.32 L/h/kg).
- The safety and effectiveness of esomeprazole sodium in neonates have not been established.
Juvenile Animal Data
- In a juvenile rat toxicity study, esomeprazole was administered with both magnesium and strontium salts at oral doses about 34 to 57 times a daily human dose of 40 mg based on body surface area. Increases in death were seen at the high dose, and at all doses of esomeprazole, there were decreases in body weight, body weight gain, femur weight and femur length, and decreases in overall growth.
Geriatic Use
- Of the total number of patients who received oral NEXIUM in clinical trials, 1,459 were 65 to 74 years of age and 354 patients were ≥ 75 years of age.
- No overall differences in safety and efficacy were observed between the elderly and younger individuals, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Gender
There is no FDA guidance on the use of Esomeprazole sodium with respect to specific gender populations.
Race
There is no FDA guidance on the use of Esomeprazole sodium with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Esomeprazole sodium in patients with renal impairment.
Hepatic Impairment
- For adult patients with GERD, no dosage adjustment is necessary in patients with mild to moderate hepatic insufficiency (Child Pugh Classes A and B). For patients with severe hepatic insufficiency (Child Pugh Class C) a dose of 20 mg once daily should not be exceeded .
- For adult patients with bleeding gastric or duodenal ulcers and liver impairment, no dosage adjustment of the initial esomeprazole 80 mg infusion is necessary. For adult patients with mild to moderate liver impairment (Child Pugh Classes A and B), a maximum continuous infusion of esomeprazole 6 mg/h should not be exceeded. For adult patients with severe liver impairment (Child Pugh Class C), a maximum continuous infusion of 4 mg/h should not be exceeded.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Esomeprazole sodium in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Esomeprazole sodium in patients who are immunocompromised.
Administration and Monitoring
Administration
Monitoring
General Information
- The reconstituted solution of esomeprazole sodium should be stored at room temperature up to 30°C (86°F) and administered within 12 hours after reconstitution. (Administer within 6 hours if 5% Dextrose Injection is used after reconstitution). No refrigeration is required
- Preparation Instructions for Adult Patients
- Intravenous Injection (20 mg or 40 mg vial) over no less than 3 minutes
- The freeze-dried powder should be reconstituted with 5 mL of 0.9% Sodium Chloride Injection, USP.
- Withdraw 5 mL of the reconstituted solution and administer as an intravenous injection over no less than 3 minutes.
- Preparation Instructions for Pediatric Patients
- Intravenous Infusion (20 mg or 40 mg) over 10 minutes to 30 minutes
- A solution for intravenous infusion is prepared by first reconstituting the contents of one vial* with 5 mL of 0.9% Sodium Chloride Injection, USP, Lactated Ringer’s Injection, USP or 5% Dextrose Injection, USP and further diluting the resulting solution to a final volume of 50 mL. The resultant concentration after diluting to a final volume of 50 mL is 0.8 mg/mL (for 40 mg vial) and 0.4 mg/mL (for 20 mg vial). The solution (admixture) should be administered as an intravenous infusion over a period of 10 minutes to 30 minutes.
- For patients 1 month to less than 1 year of age, first calculate the dose (0.5 mg/kg) to determine the vial size needed.
- Risk Reduction of Rebleeding of Gastric or Duodenal Ulcers in Adults
- Preparation Instructions for Loading dose (80 mg) to be given over 30 minutes
- The loading dose of 80 mg is prepared by reconstituting two 40 mg vials. Reconstitute each 40 mg vial with 5 mL of 0.9% Sodium Chloride Injection, USP. The contents of the two vials should be further diluted in 100 mL 0.9% * Sodium Chloride Injection, USP for intravenous use. Administer over 30 minutes.
- Preparation Instructions for Continuous Infusion to be given at 8 mg/hour for 71.5 hours
- The continuous infusion is prepared by using two 40 mg vials. Reconstitute each 40 mg vial with 5 mL each of 0.9% Sodium Chloride Injection, USP. The contents of the two vials should be further diluted in 100 mL 0.9%
- Sodium Chloride Injection, USP for intravenous use. Administer at a rate of 8 mg/hour for 71.5 hours.
IV Compatibility
There is limited information about the IV Compatibility.
Overdosage
- The minimum lethal dose of esomeprazole sodium in rats after bolus administration was 310 mg/kg (about 62 times the human dose on a body surface area basis). The major signs of acute toxicity were reduced motor activity, changes in respiratory frequency, tremor, ataxia and intermittent clonic convulsions.
- The symptoms described in connection with deliberate NEXIUM overdose (limited experience of doses in excess of 240 mg/day) are transient. Single oral doses of 80 mg and intravenous doses of 308 mg of esomeprazole over 24 hours were uneventful.
- Reports of overdosage with omeprazole in humans may also be relevant. Doses ranged up to 2,400 mg (120 times the usual recommended clinical dose). Manifestations were variable, but included confusion, drowsiness, blurred vision, tachycardia, nausea, diaphoresis, flushing, headache, dry mouth, and other adverse reactions similar to those seen in normal clinical experience. No specific antidote for esomeprazole is known. Since esomeprazole is extensively protein bound, it is not expected to be removed by dialysis. In the event of overdosage, treatment should be symptomatic and supportive.
- As with the management of any overdose, the possibility of multiple drug ingestion should be considered. For current information on treatment of any drug overdose, a certified Regional Poison Control Center should be contacted. Telephone numbers are listed in the Physicians’ Desk Reference (PDR) or local telephone book.
Pharmacology
| |
Esomeprazole sodium
| |
| Systematic (IUPAC) name | |
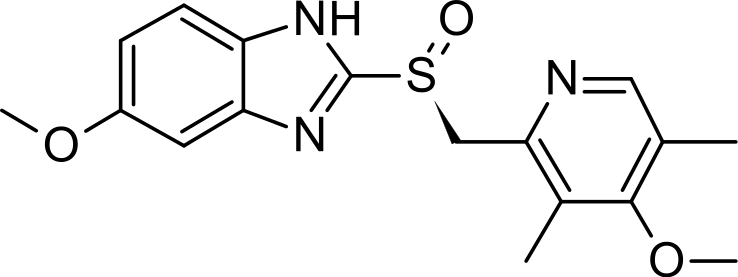
| (S)-5-methoxy-2-[(4-methoxy-3,5-dimethylpyridin-2-yl) methylsulfinyl]-3H-benzoimidazole | |
| Identifiers | |
| CAS number | |
| ATC code | A02 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 345.417 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | 50 to 90% |
| Metabolism | Hepatic (CYP2C19, CYP3A4) |
| Half life | 1–1.5 hours |
| Excretion | 80% Renal 20% Faecal |
| Therapeutic considerations | |
| Licence data |
|
| Pregnancy cat. | |
| Legal status | |
| Routes | Oral, IV |
Mechanism of Action
- Esomeprazole is a proton pump inhibitor that suppresses gastric acid secretion by specific inhibition of the H+/K+- ATPase in the gastric parietal cell. The S- and R-isomers of omeprazole are protonated and converted in the acidic compartment of the parietal cell forming the active inhibitor, the achiral sulphenamide. By acting specifically on the proton pump, esomeprazole blocks the final step in acid production, thus reducing gastric acidity. This effect is dose-related up to a daily dose of 20 to 40 mg and leads to inhibition of gastric acid secretion.
Structure
- The active ingredient in NEXIUM® I.V. (esomeprazole sodium) for Injection is (S)-5-methoxy-2[ [(4-methoxy-3,5- dimethyl-2-pyridinyl)-methyl]sulfinyl]-1 H-benzimidazole sodium, a proton pump inhibitor that inhibits gastric acid secretion. Esomeprazole is the S-isomer of omeprazole, which is a mixture of the S- and R- isomers. Its empirical formula is C17H18N3O3SNa with molecular weight of 367.4 g/mol (sodium salt) and 345.4 g/mol (parent compound). Esomeprazole sodium is very soluble in water and freely soluble in ethanol (95%). The structural formula is:

- Esomeprazole sodium for Injection is supplied as a sterile, freeze-dried, white to off-white, porous cake or powder in a 5 mL vial, intended for intravenous administration after reconstitution with 0.9% Sodium Chloride Injection, USP; Lactated Ringer’s Injection, USP or 5% Dextrose Injection, USP. esomeprazole sodium for Injection contains esomeprazole sodium 21.3 mg or 42.5 mg equivalent to esomeprazole 20 mg or 40 mg, edetate disodium 1.5 mg and sodium hydroxide q.s. for pH adjustment. The pH of reconstituted solution of esomeprazole sodium for Injection depends on the reconstitution volume and is in the pH range of 9 to 11. The stability of esomeprazole sodium in aqueous solution is strongly pH dependent. The rate of degradation increases with decreasing pH.
Pharmacodynamics
Antisecretory Activity
- The effect of intravenous esomeprazole on intragastric pH was determined in two separate studies. In the first study, 20 mg of esomeprazole sodium for Injection was administered intravenously once daily at constant rate over 30 minutes for 5 days.
- Twenty-two healthy subjects were included in the study. In the second study, 40 mg of esomeprazole sodium for Injection was administered intravenously once daily at constant rate over 30 minutes for 5 days. Thirty-eight healthy subjects were included in the study.

Gastric pH was measured over a 24-hour period
- In a study in H. pylori negative healthy Caucasian volunteers (n=24), the % time over 24 hours (95 % CI) when intragastric pH was > 6 and > 7 was 52.3 % (40.3 – 64.4) and 4.8 % (1.8 – 7.8), respectively during administration of esomeprazole as an intravenous infusion of 80 mg over 30 minutes followed by a continuous infusion of 8 mg/h for 23.5 hours.
- In a study in H. pylori positive and H. pylori negative healthy Chinese subjects (overall n=19), the % time over 24 hours (95 % CI) when intragastric pH was > 6 and > 7 was 53 % (45.6 – 60.3) and 15.1 % (9.5 – 20.7) in the overall study population during administration of esomeprazole as an intravenous infusion of 80 mg over 30 minutes followed by a continuous infusion of 8 mg/h for 23.5 hours. When comparing H. pylori positive (n=8) vs. negative (n=11) subjects, the percentage of time in a 24 h period with intragastric pH > 6 [59 % vs. 47 %] and with pH > 7 [17 % vs. 11 %] tended to be larger in the H. pylori positive subjects.
Serum Gastrin Effects
- In oral studies, the effect of NEXIUM on serum gastrin concentrations was evaluated in approximately 2,700 patients in clinical trials up to 8 weeks and in over 1,300 patients for up to 6-12 months. The mean fasting gastrin level increased in a dose-related manner. This increase reached a plateau within two to three months of therapy and returned to baseline levels within four weeks after discontinuation of therapy.
- Increased gastrin causes enterochromaffin-like cell hyperplasia and increased serum Chromogranin A (CgA) levels. The increased CgA levels may cause false positive results in diagnostic investigations for neuroendocrine tumors. Healthcare providers should temporarily stop esomeprazole treatment at least 14 days before assessing CgA levels and consider repeating the test if initial CgA levels are high.
Enterochromaffin-like (ECL) Cell Effects
- There are no data available on the effects of intravenous esomeprazole on ECL cells.
- In 24-month carcinogenicity studies of oral omeprazole in rats, a dose-related significant occurrence of gastric ECL cell carcinoid tumors and ECL cell hyperplasia was observed in both male and female animals.
- Carcinoid tumors have also been observed in rats subjected to fundectomy or long-term treatment with other proton pump inhibitors or high doses of H2-receptor antagonists.
- Human gastric biopsy specimens have been obtained from more than 3,000 patients (both children and adults) treated orally with omeprazole in long-term clinical trials. The incidence of ECL cell hyperplasia in these studies increased with time; however, no case of ECL cell carcinoids, dysplasia, or neoplasia has been found in these patients.
- In over 1,000 patients treated with NEXIUM (10, 20 or 40 mg/day) up to 6-12 months, the prevalence of ECL cell hyperplasia increased with time and dose. No patient developed ECL cell carcinoids, dysplasia, or neoplasia in the gastric mucosa.
Endocrine Effects
- NEXIUM had no effect on thyroid function when given in oral doses of 20 or 40 mg for 4 weeks. Other effects of NEXIUM on the endocrine system were assessed using omeprazole studies. Omeprazole given in oral doses of 30 or 40 mg for 2 to 4 weeks had no effect on carbohydrate metabolism, circulating levels of parathyroid hormone, cortisol, estradiol, testosterone, prolactin, cholecystokinin or secretin.
Pharmacokinetics
Absorption
- The pharmacokinetic profile of esomeprazole sodium for Injection 20 mg and 40 mg was determined in 24 healthy volunteers for the 20 mg dose and 38 healthy volunteers for the 40 mg dose following once daily administration of 20 mg and 40 mg of esomeprazole sodium for Injection by constant rate over 30 minutes for five days. The results are shown in the following table:

Values represent the geometric mean (95% CI)
- During administration of esomeprazole over 24 hours as an intravenous infusion of 80 mg over 30 minutes followed by a continuous infusion of 8 mg/h for 23.5 hours (for a total of 24 hours) in healthy volunteers (n=24), esomeprazole PK parameters [geometric mean value (95% CI)] were as follows: AUCt 111.1 µmol*h/L (100.5-122.7 µmol*h/L), Cmax 15.0 µmol/L (13.5-16.6 µmol/L), and steady state plasma concentration (Css) 3.9 µmol/L (3.5-4.5 µmol/L ).
- In a Caucasian healthy volunteer study evaluating esomeprazole 80 mg over 30 minutes, followed by 8 mg/h over 23.5 h, systemic esomeprazole exposures were modestly higher (~ 17%) in the CYP2C19 intermediate metabolizers (IM; n=6 ) compared to extensive metabolizers (EM; n=17) of CYP2C19. Similar PK differences were noted across these genotypes in a Chinese healthy volunteer study that included 7 EMs and 11 IMs. There is very limited PK information for poor metabolizers (PM) from these studies.
Distribution
- Esomeprazole is 97% bound to plasma proteins. Plasma protein binding is constant over the concentration range of 2- 20 μmol/L. The apparent volume of distribution at steady state in healthy volunteers is approximately 16 L.
Metabolism
- Esomeprazole is extensively metabolized in the liver by the cytochrome P450 (CYP) enzyme system. The metabolites of esomeprazole lack antisecretory activity. The major part of esomeprazole’s metabolism is dependent upon the CYP2C19 isoenzyme, which forms the hydroxy and desmethyl metabolites. The remaining amount is dependent on CYP3A4 which forms the sulphone metabolite. CYP2C19 isoenzyme exhibits polymorphism in the metabolism of esomeprazole, since some 3% of Caucasians and 15-20% of Asians lack CYP2C19 and are termed Poor Metabolizers. At steady state, the ratio of AUC in Poor Metabolizers to AUC in the rest of the population (Extensive metabolizers) is approximately 2.
- Following administration of equimolar doses, the S- and R-isomers are metabolize differently by the liver, resulting in higher plasma levels of the S- than of the R-isomer.
Excretion
- Esomeprazole is excreted as metabolites primarily in urine but also in feces. Less than 1% of parent drug is excreted in the urine. Esomeprazole is completely eliminated from plasma, and there is no accumulation during once daily administration. The plasma elimination half-life of intravenous esomeprazole is approximately 1.1 to 1.4 hours and is prolonged with increasing dose of intravenous esomeprazole. During administration of esomeprazole over 24 hours as an intravenous infusion of 80 mg over 30 minutes followed by a continuous infusion of 8 mg/h for 23.5 hours plasma clearance (CL) is approximately 5.9 to 7.2 L/h.
Concomitant Use with Clopidogrel
- Results from a crossover study in healthy subjects have shown a pharmacokinetic interaction between clopidogrel (300 mg loading dose/75 mg daily maintenance dose) and esomeprazole (40 mg p.o. once daily) when co-administered for 30 days. Exposure to the active metabolite of clopidogrel was reduced by 35% to 40% over this time period. Pharmacodynamic parameters were also measured and demonstrated that the change in inhibition of platelet aggregation was related to the change in the exposure to clopidogrel active metabolite.
Specific Populations
- Investigation of age, gender, race, renal, and hepatic impairment and metabolizer status has been made previously with oral esomeprazole. The pharmacokinetics of esomeprazole is not expected to be affected differently by intrinsic or extrinsic factors after intravenous administration compared to oral administration. The same recommendations for dose adjustment in special populations are suggested for intravenous esomeprazole as for oral esomeprazole.
Geriatric
- In oral studies, the AUC and Cmax values were slightly higher (25% and 18%, respectively) in the elderly as compared to younger subjects at steady state. Dosage adjustment based on age is not necessary.
Pediatric
- In a randomized, open-label, multi-national, repeated dose study, esomeprazole PK was evaluated following a once-daily 3-minute injection in a total of 50 pediatric patients 0 to 17 years old, inclusive. Esomeprazole plasma AUC values for 20 mg NEXIUM IV were 183% and 60% higher in pediatric patients aged 6 – 11 years and 12 –17 years respectively compared to adults given 20 mg. Subsequent pharmacokinetic analyses predicted that a dosage regimen of 0.5 mg/kg once-daily for pediatric patients 1-11 months of age, 10 mg for pediatric patients 1-17 years with body weight <55 kg, and 20 mg for pediatric patients 1-17 years with body >55 kg would achieve comparable steady-state plasma exposures (AUC0-24) to those observed in adult patients administered 20 mg of esomeprazole sodium once every 24 hours. Further, increasing the infusion duration from 3 minutes to 10 minutes or 30 minutes was predicted to produce steady-state Cmax values that were comparable to those observed in adult patients at the 40 mg and 20 mg esomeprazole sodium doses.
Gender
- In oral studies, the AUC and Cmax values were slightly higher (13%) in females than in males at steady state. Similar differences have been seen for intravenous administration of esomeprazole. Dosage adjustment based on gender is not necessary.
Hepatic Impairment
- In oral studies, the steady state pharmacokinetics of esomeprazole obtained after administration of 40 mg once daily to 4 patients each with mild (Child Pugh Class A), moderate (Child Pugh Class B), and severe (Child Pugh Class C) liver insufficiency were compared to those obtained in 36 male and female GERD patients with normal liver function. In patients with mild and moderate hepatic insufficiency, the AUCs were within the range that could be expected in patients with normal liver function. In patients with severe hepatic insufficiency the AUCs were 2 to 3 times higher than in the patients with normal liver function. No dosage adjustment is recommended for patients with mild to moderate hepatic insufficiency (Child Pugh Classes A and B).
- However, in patients with severe hepatic insufficiency (Child Pugh Class C) a maximum dose of 20 mg once daily should not be exceeded.
- There are no pharmacokinetic data available for esomeprazole administered as continuous intravenous administration in patients with liver impairment. The pharmacokinetics of omeprazole 80 mg over 30 minutes, followed by 8 mg/h over 47.5 hours in patients with mild (Child Pugh Class A; n=5), moderate (Child Pugh Class B; n=4) and severe (Child Pugh Class C; n=3) liver impairment were compared to those obtained in 24 male and female healthy volunteers. In patients with mild and moderate liver impairment, omeprazole clearance and steady state plasma concentration was approximately 35% lower and 50% higher, respectively, than in healthy volunteers. In patients with severe liver impairment, the omeprazole clearance was 50% of that in healthy volunteers and the steady state plasma concentration was double that in healthy volunteers.
- For adult patients with bleeding gastric or duodenal ulcers and liver impairment, no dosage adjustment of the initial esomeprazole 80 mg infusion is necessary. For adult patients with mild to moderate liver impairment (Child Pugh Classes A and B), a maximum continuous infusion of esomeprazole 6 mg/h should not be exceeded. For adult patients with severe liver impairment (Child Pugh Class C), a maximum continuous infusion of 4 mg/h should not be exceeded.
Renal Impairment
- The pharmacokinetics of esomeprazole in patients with renal impairment are not expected to be altered relative to healthy volunteers as less than 1% of esomeprazole is excreted unchanged in urine.
Microbiology
Effects on Gastrointestinal Microbial Ecology
- Decreased gastric acidity due to any means including proton pump inhibitors, increases gastric counts of bacteria normally present in the gastrointestinal tract. Treatment with proton pump inhibitors may lead to slightly increased risk of gastrointestinal infections such as Salmonella and Campylobacter and, in hospitalized patients, possibly also Clostridium difficile.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- The carcinogenic potential of esomeprazole was assessed using omeprazole studies. In two 24-month oral carcinogenicity studies in rats, omeprazole at daily doses of 1.7, 3.4, 13.8, 44.0, and 140.8 mg/kg/day (about 0.35 to 28 times the human dose of 40 mg/day expressed on a body surface area basis) produced gastric ECL cell carcinoids in a dose-related manner in both male and female rats; the incidence of this effect was markedly higher in female rats, which had higher blood levels of omeprazole. Gastric carcinoids seldom occur in the untreated rat. In addition, ECL cell hyperplasia was present in all treated groups of both sexes. In one of these studies, female rats were treated with 13.8 mg omeprazole/kg/day (about 2.8 times the human dose of 40 mg/day on a body surface area basis) for 1 year, then followed for an additional year without the drug. No carcinoids were seen in these rats. An increased incidence of treatment-related ECL cell hyperplasia was observed at the end of 1 year (94% treated vs 10% controls). By the second year the difference between treated and control rats was much smaller (46% vs 26%) but still showed more hyperplasia in the treated group. Gastric adenocarcinoma was seen in one rat (2%). No similar tumor was seen in male or female rats treated for 2 years. For this strain of rat no similar tumor has been noted historically, but a finding involving only one tumor is difficult to interpret. A 78-week oral mouse carcinogenicity study of omeprazole did not show increased tumor occurrence, but the study was not conclusive.
- Esomeprazole was negative in the Ames mutation test, in the in vivo rat bone marrow cell chromosome aberration test, and the in vivo mouse micronucleus test.
- Esomeprazole, however, was positive in the in vitro human lymphocyte chromosome aberration test. Omeprazole was positive in the in vitro human lymphocyte chromosome aberration test, the in vivo mouse bone marrow cell chromosome aberration test, and the in vivo mouse micronucleus test.
- The potential effects of esomeprazole on fertility and reproductive performance were assessed using omeprazole studies. Omeprazole at oral doses up to 138 mg/kg/day in rats (about 28 times the human dose of 40 mg/day on a body surface area basis) was found to have no effect on reproductive performance of parental animals.
Animal Toxicology and/or Pharmacology
Reproduction Studies
- Reproduction studies have been performed in rats at oral doses up to 280 mg/kg/day (about 57 times an oral human dose of 40 mg on a body surface area basis) and in rabbits at oral doses up to 86 mg/kg/day (about 35 times an oral human dose of 40 mg on a body surface area basis) and have revealed no evidence of impaired fertility or harm to the fetus due to esomeprazole.
Juvenile Animal Study
- A 28-day toxicity study with a 14-day recovery phase was conducted in juvenile rats with esomeprazole magnesium at doses of 70 to 280 mg/kg/day (about 17 to 57 times a daily oral human dose of 40 mg on a body surface area basis). An increase in the number of deaths at the high dose of 280 mg/kg/day was observed when juvenile rats were administered esomeprazole magnesium from postnatal day 7 through postnatal day 35. In addition, doses equal to or greater than 140 mg/kg/day (about 34 times a daily oral human dose of 40 mg on a body surface area basis), produced treatment-related decreases in body weight (approximately 14%) and body weight gain, decreases in femur weight and femur length, and affected overall growth. Comparable findings described above have also been observed in this study with another esomeprazole salt, esomeprazole strontium, at equimolar doses of esomeprazole.
Clinical Studies
There is limited information regarding Esomeprazole sodium Clinical Studies in the drug label.
How Supplied
- Esomeprazole sodium for Injection is supplied as a freeze-dried powder containing 20 mg or 40 mg of esomeprazole per single-use vial.
- NDC 0186-6020-01 one carton containing 10 vials of esomeprazole sodium for Injection (each vial contains 20 mg of esomeprazole).
- NDC 0186-6040-01 one carton containing 10 vials of esomeprazole sodium for Injection (each vial contains 40 mg of esomeprazole).
Storage
- Store at 25°C (77°F); excursions permitted to 15°-30°C (59°- 86°F). Protect from light. Store in carton until time of use.
- Following reconstitution and administration, discard any unused portion of esomeprazole solution.
Images
Drug Images
{{#ask: Page Name::Esomeprazole sodium |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Esomeprazole sodium |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Advise patients to let their healthcare provider know if they are taking, or begin taking other medications, because NEXIUM can interfere with antiretroviral drugs and drugs that are affected by gastric pH changes.
- Let patients know that antacids may be used while taking NEXIUM.
- Advise patients to immediately report and seek care for diarrhea that does not improve. This may be a sign of Clostridium difficile associated diarrhea.
- Advise patients to immediately report and seek care for any cardiovascular or neurological symptoms including palpitations, dizziness, seizures, and tetany as these may be signs of hypomagnesemia.
Precautions with Alcohol
Alcohol-Esomeprazole sodium interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- NEXIUM I.V ®[1]
Look-Alike Drug Names
There is limited information about the look-alike drugs.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Esomeprazole sodium |Label Name=NEXIUM_lable_01.jpg
}}
{{#subobject:
|Label Page=Esomeprazole sodium |Label Name=NEXIUM_lable_02.jpg
}}
{{#subobject:
|Label Page=Esomeprazole sodium |Label Name=NEXIUM_panel_01.png
}}
{{#subobject:
|Label Page=Esomeprazole sodium |Label Name=NEXIUM_panel_02.png
}}