Doravirine
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Zach Leibowitz [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
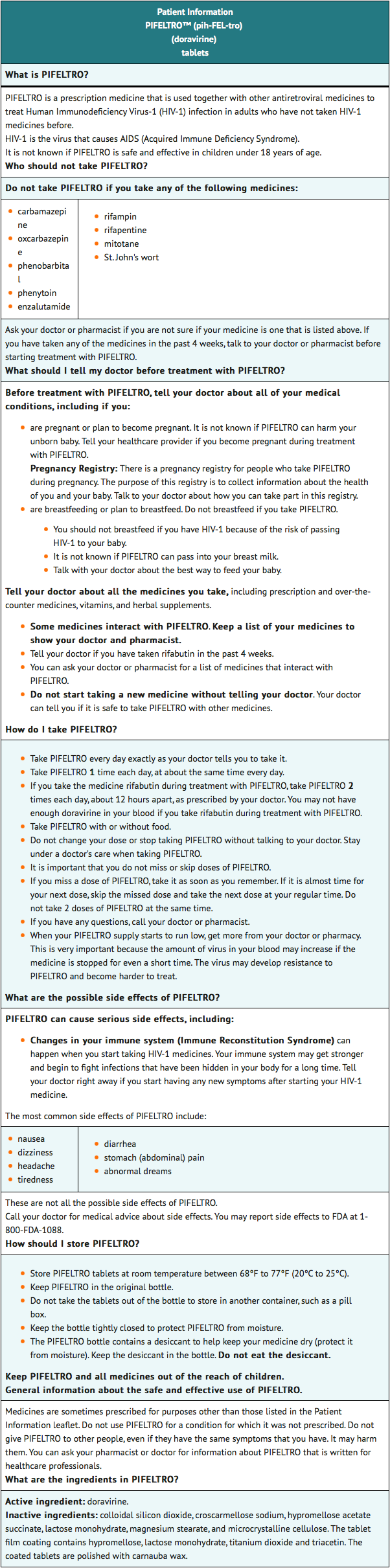
Doravirine is a non-nucleoside reverse transcriptase inhibitor (NNRTI) that is FDA approved for the treatment of HIV-1 infection in adult patients with no prior antiretroviral treatment history, in combination with other antiretroviral agents. Common adverse reactions include nausea, dizziness, headache, fatigue, diarrhea, abdominal pain, and abnormal dreams.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indication
- Doravirine is indicated in combination with other antiretroviral agents for the treatment of HIV-1 infection in adult patients with no prior antiretroviral treatment history.
Dosage
- One tablet taken orally once daily with or without food in adult patients.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding doravirine Off-Label Guideline-Supported Use and Dosage (Adult) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding doravirine Off-Label Non-Guideline-Supported Use and Dosage (Adult) in the drug label.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Safety and efficacy of doravirine have not been established in pediatric patients less than 18 years of age.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding doravirine Off-Label Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding doravirine Off-Label Non-Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Contraindications
- Doravirine is contraindicated when co-administered with drugs that are strong cytochrome P450 (CYP)3A enzyme inducers as significant decreases in doravirine plasma concentrations may occur, which may decrease the effectiveness of doravirine. These drugs include, but are not limited to, the following:
- the anticonvulsants carbamazepine, oxcarbazepine, phenobarbital, phenytoin
- the androgen receptor inhibitor enzalutamide
- the antimycobacterials rifampin, rifapentine
- the cytotoxic agent mitotane
- St. John's wort (Hypericum perforatum)
Warnings
Risk of Adverse Reactions or Loss of Virologic Response Due to Drug Interactions
- The concomitant use of doravirine and certain other drugs may result in known or potentially significant drug interactions, some of which may lead to loss of therapeutic effect of doravirine and possible development of resistance.
- See TABLE 5 for steps to prevent or manage these possible and known significant drug interactions, including dosing recommendations. Consider the potential for drug interactions prior to and during doravirine therapy, review concomitant medications during doravirine therapy, and monitor for adverse reactions.
Immune Reconstitution Syndrome
- Immune reconstitution syndrome has been reported in patients treated with combination antiretroviral therapy. During the initial phase of combination antiretroviral treatment, patients whose immune system responds may develop an inflammatory response to indolent or residual opportunistic infections (such as Mycobacterium avium infection, cytomegalovirus, Pneumocystis jirovecii pneumonia (PCP), or tuberculosis), which may necessitate further evaluation and treatment.
- Autoimmune disorders (such as Graves' disease, polymyositis, and Guillain-Barré syndrome) have also been reported to occur in the setting of immune reconstitution; however, the time to onset is more variable and can occur many months after initiation of treatment.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adverse Reactions in Adults with No Prior Antiretroviral Treatment History
- The safety assessment of doravirine used in combination with other antiretroviral agents is based on Week 48 data from two Phase 3, randomized, international, multicenter, double-blind, active-controlled trials (DRIVE-FORWARD (Protocol 018) and DRIVE-AHEAD (Protocol 021)).
- In DRIVE-FORWARD, 766 adult subjects received either doravirine 100 mg (n=383) or darunavir 800 mg + ritonavir 100 mg (DRV+r) (n=383) once daily, each in combination with emtricitabine/tenofovir disoproxil fumarate (FTC/TDF) or abacavir/lamivudine (ABC/3TC). By Week 48, 2% in the doravirine group and 3% in the DRV+r group had adverse events leading to discontinuation of study medication.
- In DRIVE-AHEAD, 728 adult subjects received either DELSTRIGO [doravirine (DOR)/3TC/TDF] (n=364) or efavirenz (EFV)/FTC/TDF once daily (n=364). By Week 48, 3% in the DELSTRIGO group and 6% in the EFV/FTC/TDF group had adverse events leading to discontinuation of study medication.
- Adverse reactions reported in greater than or equal to 5% of subjects in any treatment group in DRIVE-FORWARD and DRIVE-AHEAD are presented in Table 1.
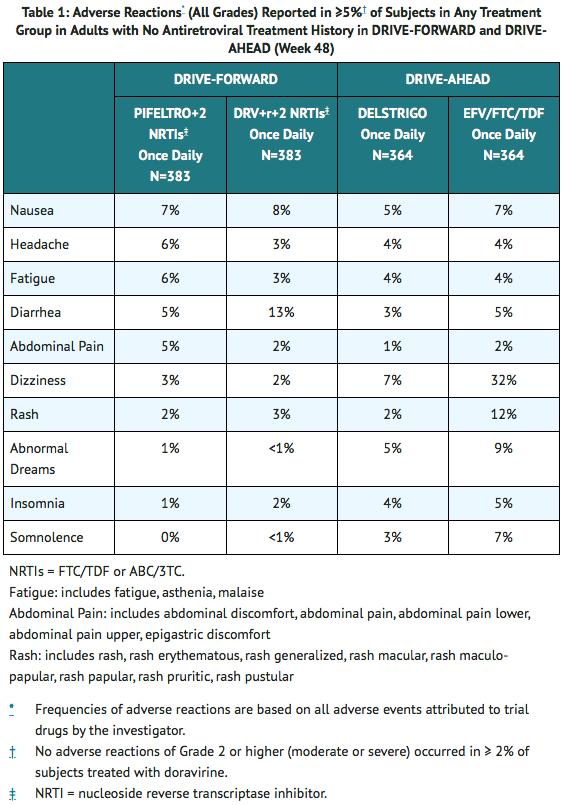
- The majority (72%) of adverse reactions associated with doravirine occurred at severity Grade 1 (mild).
Neuropsychiatric Adverse Events
- For DRIVE-AHEAD, the analysis of subjects with neuropsychiatric adverse events by Week 48 is presented in Table 2. The proportion of subjects who reported one or more neuropsychiatric adverse events was 24% and 57% in the DELSTRIGO and EFV/FTC/TDF groups, respectively.
- A statistically significantly lower proportion of DELSTRIGO-treated subjects compared to EFV/FTC/TDF-treated subjects reported neuropsychiatric adverse events by Week 48 in the three pre-specified categories of dizziness, sleep disorders and disturbances, and altered sensorium.
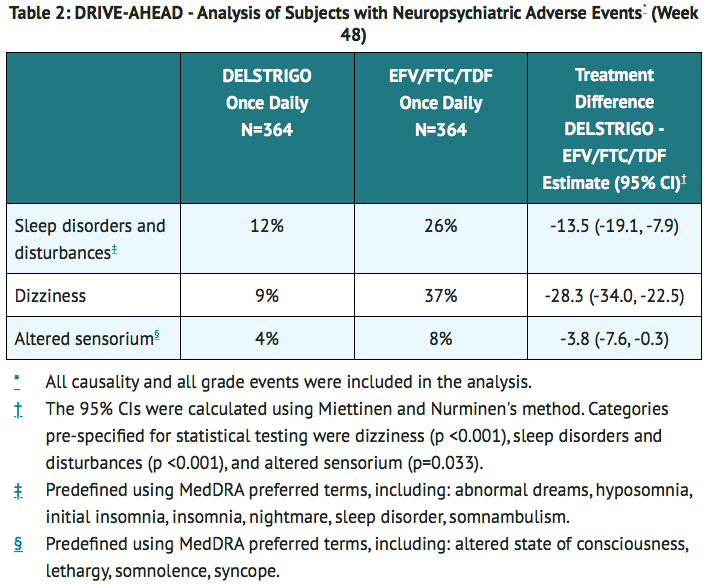
- Neuropsychiatric adverse events in the pre-defined category of depression and suicide/self-injury were reported in 4% and 7% of subjects, in the DELSTRIGO and EFV/FTC/TDF groups, respectively.
- In DRIVE-AHEAD through 48 weeks of treatment, the majority of subjects who reported neuropsychiatric adverse events reported events that were mild to moderate in severity (97% [83/86] and 96% [198/207], in the DELSTRIGO and EFV/FTC/TDF groups, respectively) and the majority of subjects reported these events in the first 4 weeks of treatment (72% [62/86] in the DELSTRIGO group and 86% [177/207] in the EFV/FTC/TDF group).
- Neuropsychiatric adverse events led to treatment discontinuation in 1% (2/364) and 1% (5/364) of subjects in the DELSTRIGO and EFV/FTC/TDF groups, respectively. The proportion of subjects who reported neuropsychiatric adverse events through Week 4 was 17% (62/364) in the DELSTRIGO group and 49% (177/364) in the EFV/FTC/TDF group. At Week 48, the prevalence of neuropsychiatric adverse events was 12% (44/364) in the DELSTRIGO group and 22% (81/364) in the EFV/FTC/TDF group.
Laboratory Abnormalities
- The percentages of subjects with selected laboratory abnormalities (that represent a worsening from baseline) who were treated with doravirine or DRV+r in DRIVE-FORWARD, or DELSTRIGO or EFV/FTC/TDF in DRIVE-AHEAD are presented in Table 3.

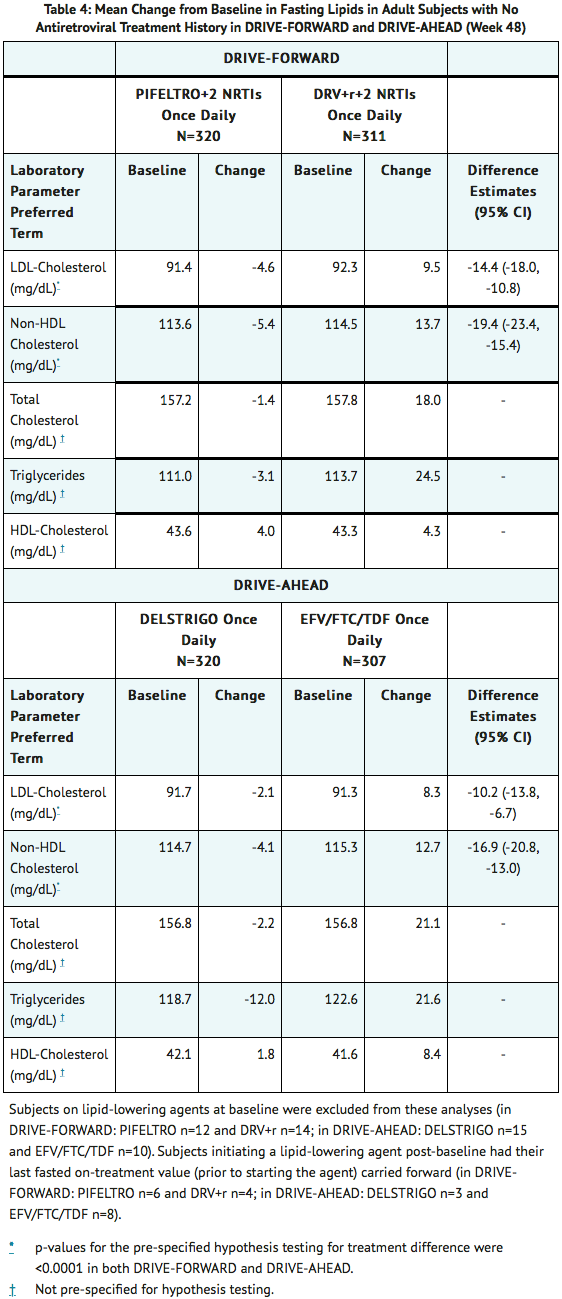
Change in Lipids from Baseline
- For DRIVE-FORWARD and DRIVE-AHEAD, changes from baseline at Week 48 in LDL-cholesterol, non-HDL-cholesterol, total cholesterol, triglycerides, and HDL-cholesterol are shown in Table 4.
- The LDL and non-HDL comparisons were pre-specified and are summarized in Table 4. The differences were statistically significant, showing superiority for doravirine for both parameters. The clinical benefit of these findings has not been demonstrated.
Postmarketing Experience
There is limited information regarding Doravirine Postmarketing Experience in the drug label.
Drug Interactions
Effect of Other Drugs on Doravirine
- Co-administration of doravirine with a CYP3A inducer decreases doravirine plasma concentrations, which may reduce doravirine efficacy. Co-administration of doravirine and drugs that are inhibitors of CYP3A may result in increased plasma concentrations of doravirine.
- Table 5 shows significant drug interactions with doravirine.
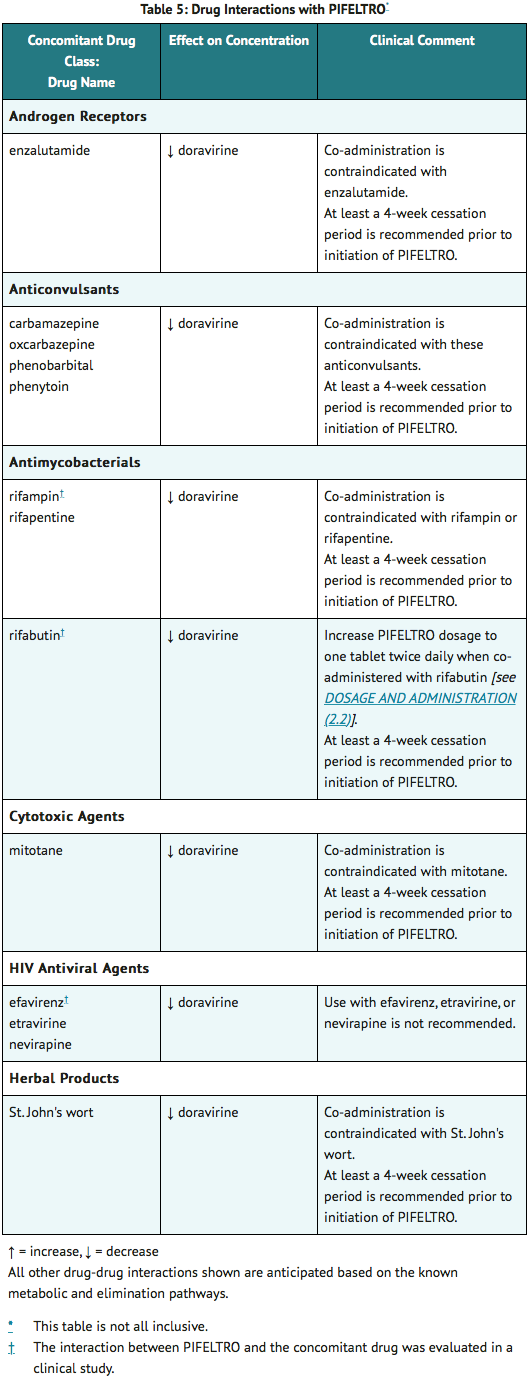
- No clinically significant changes in concentration were observed for doravirine when co-administered with the following agents: dolutegravir, TDF, lamivudine, elbasvir and grazoprevir, ledipasvir and sofosbuvir, ritonavir, ketoconazole, aluminum hydroxide/magnesium hydroxide/simethicone containing antacid, pantoprazole, and methadone.
Effect of Doravirine on Other Drugs
- No clinically significant changes in concentration were observed for the following agents when co-administered with doravirine: dolutegravir, lamivudine, TDF, elbasvir and grazoprevir, ledipasvir and sofosbuvir, atorvastatin, an oral contraceptive containing ethinyl estradiol and levonorgestrel, metformin, methadone, and midazolam.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): Pregnancy Exposure Registry
- There is a pregnancy exposure registry that monitors pregnancy outcomes in individuals exposed to doravirine during pregnancy. Healthcare providers are encouraged to register patients by calling the Antiretroviral Pregnancy Registry (APR) at 1-800-258-4263.
Risk Summary
- No adequate human data are available to establish whether or not doravirine poses a risk to pregnancy outcomes. In animal reproduction studies, no adverse developmental effects were observed when doravirine was administered at exposures ≥8 times the exposure in humans at the recommended human dose (RHD) of doravirine.
- The background rate of major birth defects is 2.7% in a U.S. reference population of the Metropolitan Atlanta Congenital Defects Program (MACDP). The rate of miscarriage is not reported in the APR. The estimated background rate of miscarriage in the clinically recognized pregnancies in the U.S. general population is 15-20%. Methodological limitations of the APR include the use of MACDP as the external comparator group. The MACDP population is not disease-specific, evaluates individuals and infants from the limited geographic area, and does not include outcomes for births that occurred at less than 20 weeks gestation.
Animal Data
- Doravirine was administered orally to pregnant rabbits (up to 300 mg/kg/day on gestation days (GD) 7 to 20) and rats (up to 450 mg/kg/day on GD 6 to 20 and separately from GD 6 to lactation/postpartum day 20). No significant toxicological effects on embryo-fetal (rats and rabbits) or pre/post-natal (rats) development were observed at exposures (AUC) approximately 9 times (rats) and 8 times (rabbits) the exposure in humans at the RHD. Doravirine was transferred to the fetus through the placenta in embryo-fetal studies, with fetal plasma concentrations of up to 40% (rabbits) and 52% (rats) that of maternal concentrations observed on gestation day 20.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Doravirine in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Doravirine during labor and delivery.
Nursing Mothers
Risk Summary
- The Centers for Disease Control and Prevention recommend that HIV-1-infected mothers in the United States not breastfeed their infants to avoid risking potential transmission of HIV-1 infection.
- It is unknown whether doravirine is present in human milk, affects human milk production, or has effects on the breastfed infant. Doravirine is present in the milk of lactating rats (see DATA). Because of the potential for (1) HIV-1 transmission (in HIV-negative infants), (2) developing viral resistance (in HIV-positive infants), and (3) serious adverse reactions in a breastfed infant, instruct mothers not to breastfeed if they are receiving doravirine.
Data
- Doravirine was excreted into the milk of lactating rats following oral administration (450 mg/kg/day) from gestation day 6 to lactation day 14, with milk concentrations approximately 1.5 times that of maternal plasma concentrations observed 2 hours post dose on lactation day 14.
Pediatric Use
- Safety and efficacy of doravirine have not been established in pediatric patients less than 18 years of age.
Geriatic Use
- Clinical trials of doravirine did not include sufficient numbers of subjects aged 65 years and over to determine whether they respond differently from younger subjects. In general, caution should be exercised in the administration of doravirine in elderly patients, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Gender
There is no FDA guidance on the use of Doravirine with respect to specific gender populations.
Race
There is no FDA guidance on the use of Doravirine with respect to specific racial populations.
Renal Impairment
- No dosage adjustment of doravirine is required in patients with mild, moderate, or severe renal impairment. Doravirine has not been adequately studied in patients with end-stage renal disease and has not been studied in dialysis patients.
Hepatic Impairment
- No dosage adjustment of doravirine is required in patients with mild (Child-Pugh Class A) or moderate (Child-Pugh Class B) hepatic impairment. Doravirine has not been studied in patients with severe hepatic impairment (Child-Pugh Class C).
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Doravirine in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Doravirine in patients who are immunocompromised.
Administration and Monitoring
Administration
Recommended Dosage
- The recommended dosage regimen of doravirine in adults is one 100 mg tablet taken orally once daily with or without food.
Dosage Adjustment with Rifabutin
- If doravirine is co-administered with rifabutin, increase doravirine dosage to one tablet twice daily (approximately 12 hours apart) for the duration of rifabutin co-administration.
Monitoring
There is limited information regarding Doravirine Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Doravirine and IV administrations.
Overdosage
There is limited information regarding Doravirine overdosage. If you suspect drug poisoning or overdose, please contact the National Poison Help hotline (1-800-222-1222) immediately.
Pharmacology
| |
Doravirine
| |
| Systematic (IUPAC) name | |
| 3-Chloro-5-({1-[(4-methyl-5-oxo-4,5-dihydro-1H-1,2,4-triazol-3-yl)methyl]-2-oxo-4-(trifluoromethyl)-1,2-dihydro-3-pyridinyl}oxy)benzonitrile | |
| Identifiers | |
| CAS number | |
| ATC code | J05 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 425.75 g/mol |
| SMILES | & |
| Synonyms | MK-1439 |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status |
[[Prescription drug|Template:Unicode-only]](US) |
| Routes | Oral[1] |
Mechanism of Action
- Doravirine is an antiretroviral drug.
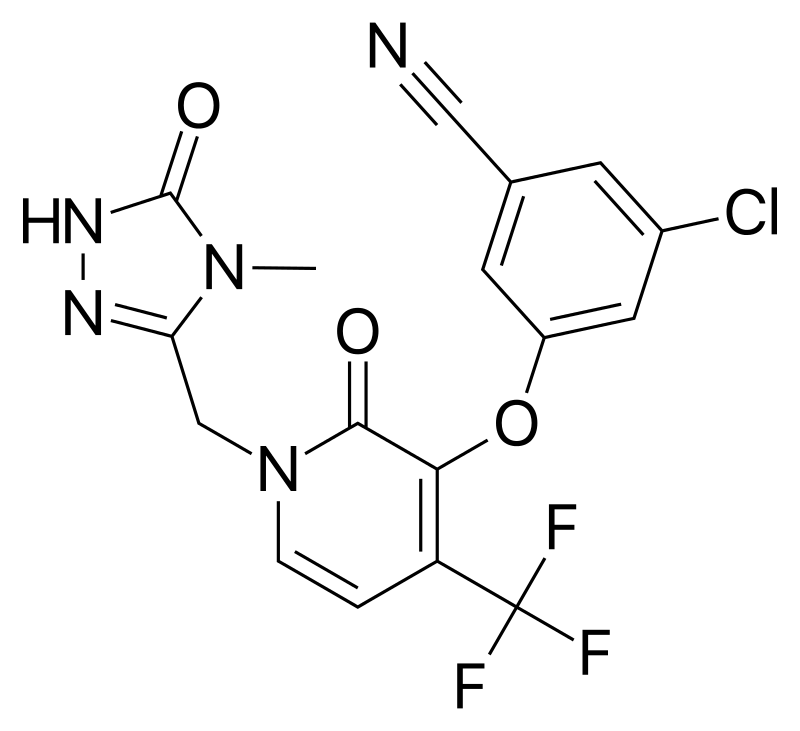
Structure
- Doravirine has a molecular formula of C17H11ClF3N5O3 and a molecular weight of 425.75.
- It has the following structural formula:
Pharmacodynamics
- In a Phase 2 trial evaluating doravirine over a dose range of 0.25 to 2 times the recommended dose of doravirine, (in combination with FTC/TDF) in HIV-1 infected subjects with no antiretroviral treatment history, no exposure-response relationship for efficacy was identified for doravirine.
Cardiac Electrophysiology
- At a doravirine dose of 1200 mg, which provides approximately 4 times the peak concentration observed following the recommended dose of doravirine, doravirine does not prolong the QT interval to any clinically relevant extent.
Pharmacokinetics
- Doravirine pharmacokinetics are similar in healthy subjects and HIV-1-infected subjects. Doravirine pharmacokinetics are provided in Table 6.

Specific Populations
- No clinically significant difference on the pharmacokinetics of doravirine were observed based on age (18 to 78 years of age), sex, and race/ethnicity, mild to severe renal impairment (creatinine clearance (CLcr) >15 mL/min, estimated by Cockcroft-Gault), or moderate hepatic impairment (Child-Pugh B). The pharmacokinetics of doravirine in patients with end-stage renal disease or undergoing dialysis, severe hepatic impairment (Child-Pugh C), or <18 years of age is unknown.
Patients with Renal Impairment
- In a study comparing 8 subjects with severe renal impairment to 8 subjects without renal impairment, the single dose exposure of doravirine was 43% higher in subjects with severe renal impairment. In a population pharmacokinetic analysis, renal function did not have a clinically relevant effect on doravirine pharmacokinetics. Doravirine has not been studied in patients with end-stage renal disease or in patients undergoing dialysis.
Patients with Hepatic Impairment
- No clinically significant difference in the pharmacokinetics of doravirine was observed in subjects with moderate hepatic impairment (Child-Pugh score B) compared to subjects without hepatic impairment. Doravirine has not been studied in subjects with severe hepatic impairment (Child-Pugh score C).
Drug Interaction Studies
- Doravirine is primarily metabolized by CYP3A, and drugs that induce or inhibit CYP3A may affect the clearance of doravirine. Co-administration of doravirine and drugs that induce CYP3A may result in decreased plasma concentrations of doravirine. Co-administration of doravirine and drugs that inhibit CYP3A may result in increased plasma concentrations of doravirine.
- Doravirine is not likely to have a clinically relevant effect on the exposure of medicinal products metabolized by CYP enzymes. Doravirine did not inhibit major drug metabolizing enzymes in vitro, including CYPs 1A2, 2B6, 2C8, 2C9, 2C19, 2D6, 3A4, and UGT1A1 and is not likely to be an inducer of CYP1A2, 2B6, or 3A4. Based on in vitro assays, doravirine is not likely to be an inhibitor of OATP1B1, OATP1B3, P-glycoprotein, BSEP, OAT1, OAT3, OCT2, MATE1, and MATE2K. Drug interaction studies were performed with doravirine and other drugs likely to be co-administered or commonly used as probes for pharmacokinetic interactions. The effects of co-administration with other drugs on the exposure (Cmax, AUC, and C24) of doravirine are summarized in Table 7. A single doravirine 100 mg dose was administered in these studies unless otherwise noted.
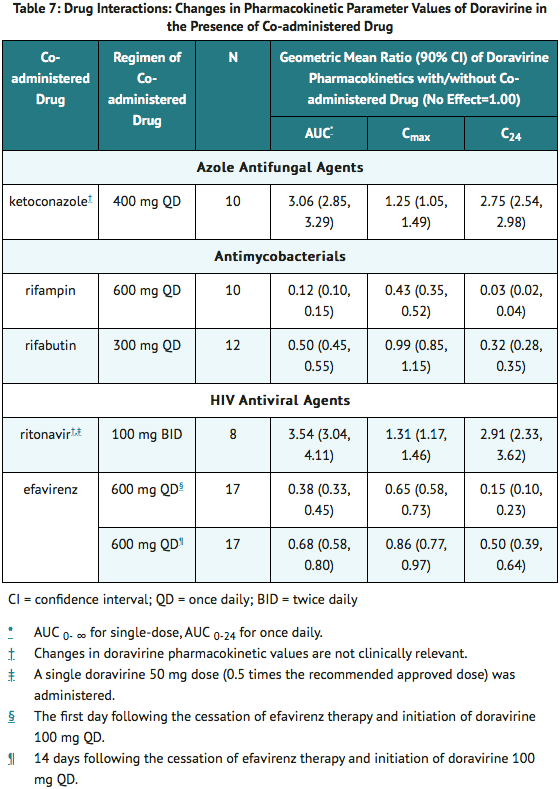
- Based on drug interaction studies conducted with doravirine, no clinically significant drug interactions have been observed following the co-administration of doravirine and the following drugs: dolutegravir, ritonavir, TDF, lamivudine, elbasvir and grazoprevir, ledipasvir and sofosbuvir, ketoconazole, aluminum hydroxide/magnesium hydroxide/simethicone containing antacid, pantoprazole, atorvastatin, an oral contraceptive containing ethinyl estradiol and levonorgestrel, metformin, methadone, and midazolam.
Microbiology
Mechanism of Action
- Doravirine is a pyridinone non-nucleoside reverse transcriptase inhibitor of HIV-1 and inhibits HIV-1 replication by non-competitive inhibition of HIV-1 reverse transcriptase (RT). Doravirine does not inhibit the human cellular DNA polymerases α, ß, and mitochondrial DNA polymerase γ.
Antiviral Activity in Cell Culture
- Doravirine exhibited an EC50 value of 12.0±4.4 nM against wild-type laboratory strains of HIV-1 when tested in the presence of 100% normal human serum (NHS) using MT4-GFP reporter cells. Doravirine demonstrated antiviral activity against a broad panel of primary HIV-1 isolates (A, A1, AE, AG, B, BF, C, D, G, H) with EC50 values ranging from 0.6 nM to 10.0 nM.
Antiviral Activity in Combination with other HIV Antiviral Agents
- The antiviral activity of doravirine in cell culture was not antagonistic when combined with the NNRTIs delavirdine, efavirenz, etravirine, nevirapine, or rilpivirine; the NRTIs abacavir, didanosine, emtricitabine, lamivudine, stavudine, tenofovir DF, or zidovudine; the PIs darunavir or indinavir; the gp41 fusion inhibitor enfuvirtide; the CCR5 co-receptor antagonist maraviroc; or the integrase strand transfer inhibitor raltegravir.
Resistance
In Cell Culture
- Doravirine-resistant strains were selected in cell culture starting from wild-type HIV-1 of different origins and subtypes, as well as NNRTI-resistant HIV-1. Observed emergent amino acid substitutions in RT included: V106A, V106M, V106I, V108I, H221Y, F227C, F227I, F227L, F227V, M230I, L234I, P236L, and Y318F.
In Clinical Trials
- In the doravirine treatment arms of the DRIVE-FORWARD and DRIVE-AHEAD trials (n=747), 11 subjects showed the emergence of doravirine-associated resistance substitutions in their HIV among 28 (39%) subjects in the resistance analysis subset (subjects with HIV-1 RNA greater than 400 copies per mL at virologic failure or early study discontinuation and having resistance data). Emergent doravirine resistance-associated substitutions in RT included one or more of the following: A98G, V106I, V106A, V106M/T, V108I, E138G/K, Y188L, H221Y, P225H, F227C, F227C/R, and Y318Y/F. Seven of 11 (64%) subjects with emergent doravirine-associated resistance substitutions showed doravirine phenotypic resistance and all of them had at least a 100-fold reduction in doravirine susceptibility (range >97- to >211–fold reduction in doravirine susceptibility). The other 4 virologic failures who had only amino acid mixtures of NNRTI resistance substitutions showed doravirine phenotypic fold-changes of less than 2-fold. Of the 28 subjects in the resistance analysis subset, 8 subjects (29%) developed genotypic and/or phenotypic resistance to the other drugs (abacavir, lamivudine, emtricitabine, or TDF) in the regimens of the DRIVE-FORWARD and DRIVE-AHEAD trials. The resistance-associated substitutions that emerged were RT M41L (n=1), A62V (n=1), K65R (n=2), T69T/A (n=1), and M184V (n=5).
- In the DRV+r treatment arm of the DRIVE-FORWARD trial (n=383), no subjects showed the emergence of darunavir-associated resistance substitutions among 9 subjects with resistance data and none of the subjects had emergent resistance to lamivudine or TDF. In the EFV/FTC/TDF treatment arm of the DRIVE-AHEAD trial (n=364), 12 subjects showed the emergence of efavirenz-associated resistance substitutions among 20 (60%) subjects in the resistance analysis subset and genotypic resistance to emtricitabine or tenofovir developed in 5 evaluable subjects; emergent resistance-associated substitutions were RT K65R (n=1), D67G/K70E (n=1), L74V/V75M/V118I (n=1), and M184V/I (n=5).
Cross-Resistance
- A panel of 96 diverse clinical isolates containing NNRTI-associated substitutions was evaluated for susceptibility to doravirine. Clinical isolates containing the Y188L substitution alone or in combination with K103N or V106I, V106A in combination with G190A and F227L, or E138K in combination with Y181C and M230L showed greater than 100-fold reduced susceptibility to doravirine.
- Cross-resistance has been observed among NNRTIs. Treatment-emergent doravirine resistance-associated substitutions can confer cross resistance to efavirenz, etravirine, nevirapine, and rilpivirine. Of the 7 virologic failures who developed doravirine phenotypic resistance, all had phenotypic resistance to nevirapine, 6 had phenotypic resistance to efavirenz, 4 had phenotypic resistance to rilpivirine, and 3 had partial resistance to etravirine based on the Monogram PhenoSense assay.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
- Doravirine was not carcinogenic in long-term oral carcinogenicity studies in mice and rats at exposures up to 6 and 7 times, respectively, the human exposures at the RHD. A statistically significant incidence of thyroid parafollicular cell adenoma and carcinoma seen only in female rats at the high dose was within the range observed in historical controls.
Mutagenesis
- Doravirine was not genotoxic in a battery of in vitro or in vivo assays, including microbial mutagenesis, chromosomal aberration in Chinese hamster ovary cells, and in in vivo rat micronucleus assays.
Impairment of fertility
- There were no effects on fertility, mating performance or early embryonic development when doravirine was administered to rats at systemic exposures (AUC) approximately 7 times the exposure in humans at the RHD.
Clinical Studies
Adult Subjects with No Antiretroviral Treatment History
- The efficacy of doravirine is based on the analyses of 48-week data from two randomized, multicenter, double-blind, active controlled Phase 3 trials (DRIVE-FORWARD, NCT02275780 and DRIVE-AHEAD, NCT02403674) in HIV-1 infected subjects with no antiretroviral treatment history (n=1494).
- In DRIVE-FORWARD, 766 subjects were randomized and received at least 1 dose of either doravirine once daily or darunavir 800 mg + ritonavir 100 mg (DRV+r) once daily each in combination with emtricitabine/tenofovir DF (FTC/TDF) or abacavir/lamivudine (ABC/3TC) selected by the investigator. At baseline, the median age of subjects was 33 years, 16% were female, 27% were non-white, 4% had hepatitis B and/or C virus co-infection, 10% had a history of AIDS, 20% had HIV-1 RNA greater than 100,000 copies/mL, 86% had CD4+ T-cell count greater than 200 cells/mm3, 13% received ABC/3TC, and 87% received FTC/TDF; these characteristics were similar between treatment groups.
- In DRIVE-AHEAD, 728 subjects were randomized and received at least 1 dose of either DELSTRIGO (DOR/3TC/TDF) or EFV 600 mg/FTC 200 mg/TDF 300 mg once daily. At baseline, the median age of subjects was 31 years, 15% were female, 52% were non-white, 3% had hepatitis B or C co-infection, 14% had a history of AIDS, 21% had HIV-1 RNA greater than 100,000 copies/mL, and 88% had CD4+ T-cell count greater than 200 cells/mm3; these characteristics were similar between treatment groups.
- Week 48 outcomes for DRIVE-FORWARD and DRIVE-AHEAD are provided in Table 8. Side-by-side tabulation is to simplify presentation; direct comparisons across trials should not be made due to differing trial designs.
- In DRIVE-FORWARD, the mean CD4+ T-cell counts in the doravirine and DRV+r groups increased from baseline by 193 and 186 cells/mm3, respectively.
- In DRIVE-AHEAD, the mean CD4+ T-cell counts in the DELSTRIGO and EFV/FTC/TDF groups increased from baseline by 198 and 188 cells/mm3, respectively.

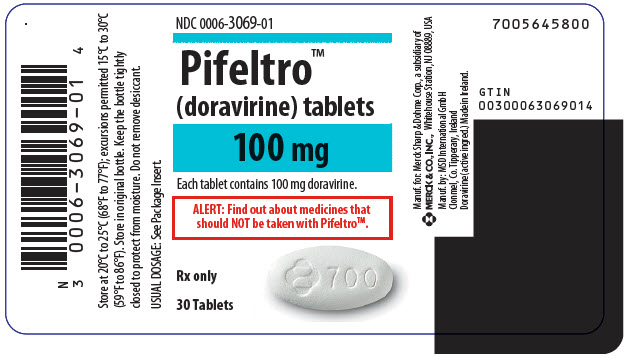
How Supplied
- Each doravirine tablet contains 100 mg of doravirine, is white, oval-shaped and film-coated, and is debossed with the corporate logo and 700 on one side and plain on the other side. Each bottle contains 30 tablets (NDC 0006-3069-01) with silica gel desiccant and is closed with a child-resistant closure.
Storage
- Store doravirine in the original bottle. Keep the bottle tightly closed to protect from moisture. Do not remove the desiccant.
- Store doravirine at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Images
Drug Images
{{#ask: Page Name::Doravirine |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Doravirine |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Drug Interactions
- Inform patients that doravirine may interact with certain other drugs; therefore, advise patients to report to their healthcare provider the use of any other prescription or nonprescription medication or herbal products, including St. John's wort.
- For patients concomitantly receiving rifabutin, take one tablet of doravirine twice daily (approximately 12 hours apart).
Immune Reconstitution Syndrome
- Inform patients that in some patients with advanced HIV infection (AIDS), signs and symptoms of inflammation from previous infections may occur soon after anti-HIV treatment is started. It is believed that these symptoms are due to an improvement in the body's immune response, enabling the body to fight infections that may have been present with no obvious symptoms. Advise patients to inform their healthcare provider immediately of any symptoms of infection.
Dosing Instructions
- Advise patients to take doravirine every day at a regularly scheduled time with or without food. Inform patients that it is important not to miss or skip doses as it can result in development of resistance. If a patient forgets to take doravirine, tell the patient to take the missed dose right away, unless it is almost time for the next dose. Advise the patient not to take 2 doses at one time and to take the next dose at the regularly scheduled time.
Pregnancy Registry
- Inform patients that there is an antiretroviral pregnancy registry to monitor fetal outcomes in pregnant individuals exposed to doravirine.
Lactation
- Instruct mothers with HIV-1 infection not to breastfeed because HIV-1 can be passed to the baby in breast milk.
Patient Package Insert
Precautions with Alcohol
Alcohol-Doravirine interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
Look-Alike Drug Names
There is limited information regarding Doravirine Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Collins, Simon; Horn, Tim. "The Antiretroviral Pipeline" (PDF). Pipeline Report. p. 10. Archived from the original (PDF) on 11 March 2016. Retrieved 6 December 2015.