Fascia
Template:WikiDoc Cardiology News Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Fascia (făsh'ē-ə), pl. fas·ci·ae (făsh'ē-ē), adj. fascial (făsh'ē-əl) (from latin: a band) is the soft tissue component of the connective tissue system that permeates the human body. It interpenetrates and surrounds muscles, bones, organs, nerves, blood vessels and other structures. Fascia is an uninterrupted, three-dimensional web of tissue that extends from head to toe, from front to back, from interior to exterior. It is responsible for maintaining structural integrity; for providing support and protection; and acts as a shock absorber. Fascia has an essential role in hemodynamic and biochemical processes, and provides the matrix that allows for intercellular communication. Fascia functions as the body's first line of defense against pathogenic agents and infections. After injury, it is the fascia that creates an environment for tissue repair. [1]
Three layers of the fascia
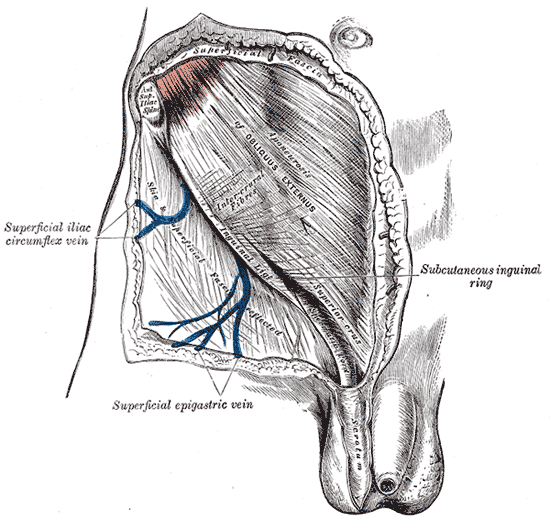
- Superficial fascia is found in the subcutis in most regions of the body, blending with the reticular layer of the dermis. [2] It is present on the face, over the upper portion of the sternocleidomastoid, at the nape of the neck, and overlying the sternum. [3] It is comprised mainly of loose areolar connective tissue and adipose and is the layer that primarily determines the shape of a body. In addition to its subcutaneous presence, this type of fascia surrounds organs and glands, neurovascular bundles, and is found at many other locations where it fills otherwise unoccupied space. It serves as a storage medium of fat and water; as a passageway for lymph, nerve and blood vessels; and as a protective padding to cushion and insulate. [4]
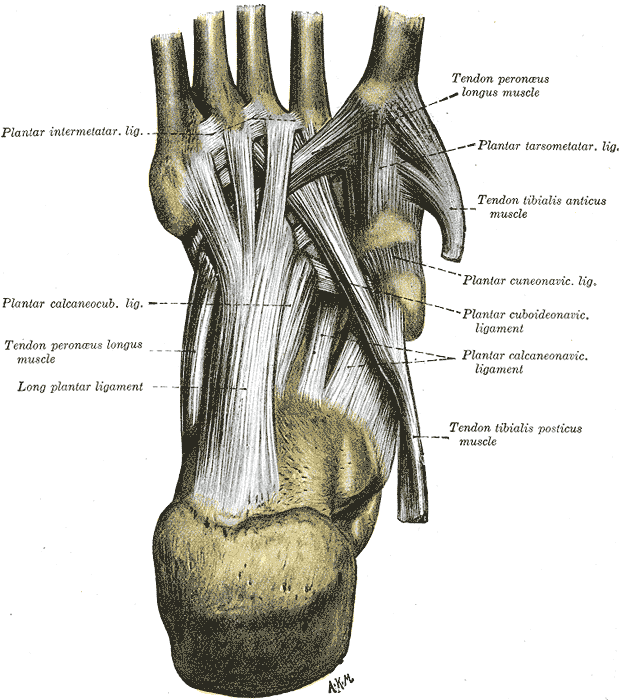
- Deep fascia is the dense fibrous connective tissue that interpenetrates and surrounds the muscles, bones, nerves and blood vessels of the body. It provides connection and communication in the form of aponeuroses, ligaments, tendons, retinacula, joint capsules, and septa. The deep fasciae envelop all bone (periosteum and endosteum); cartilage (perichondrium), and blood vessels (tunica externa) and become specialized in muscles (epimysium, perimysium, and endomysium) and nerves (epineurium, perineurium, and endoneurium). The high density of collagen fibers is what gives the deep fascia its strength and integrity. The amount of elastin fibers determines how much extensibility and resiliancy it will have. [5]
-
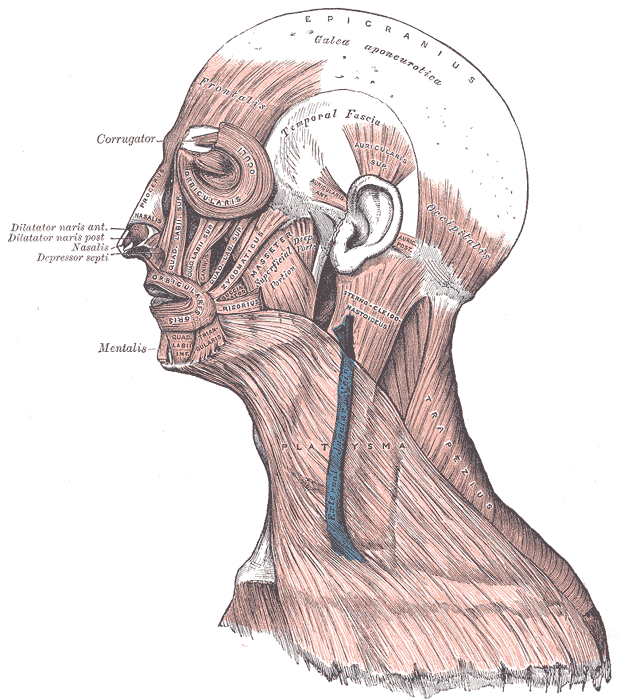
The galea aponeurotica and the temporal fascia
-
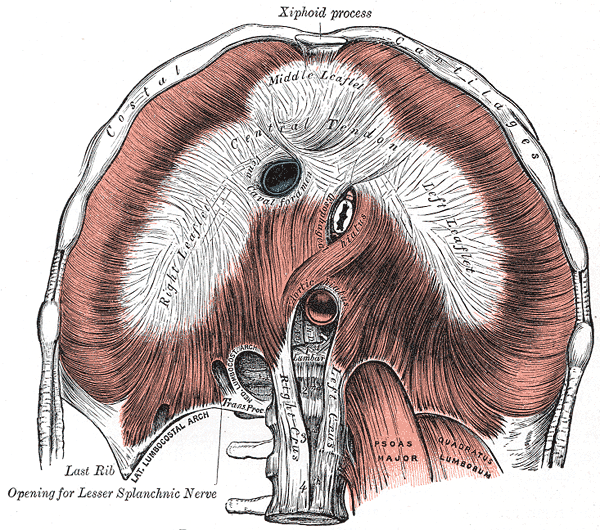
The fascia of the diaphragm
- Visceral Fascia suspends the organs within their cavities and wraps them in layers of connective tissue membranes. Each of the organs is covered in a double layer of fascia; these layers are separated by a thin serous membrane. The outermost wall of the organ is known as the parietal layer, whereas the skin of the organ is known as the visceral layer. The organs have specialized names for their visceral fasciae. In the brain, they are known as meninges; in the heart they are known as pericardia; in the lungs, they are known as pleura; and in the abdomen, they are known as peritonea. [6]
-
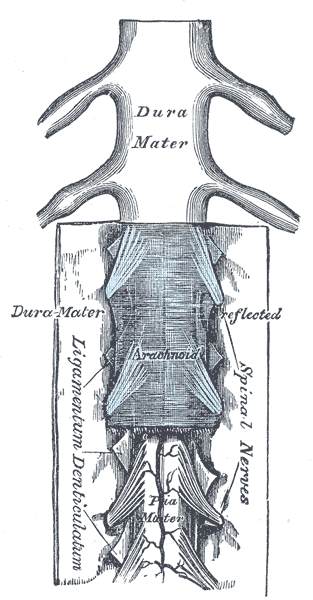
The meninges
-
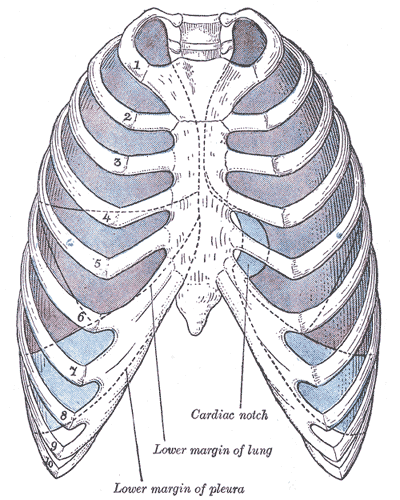
The pleurae
-
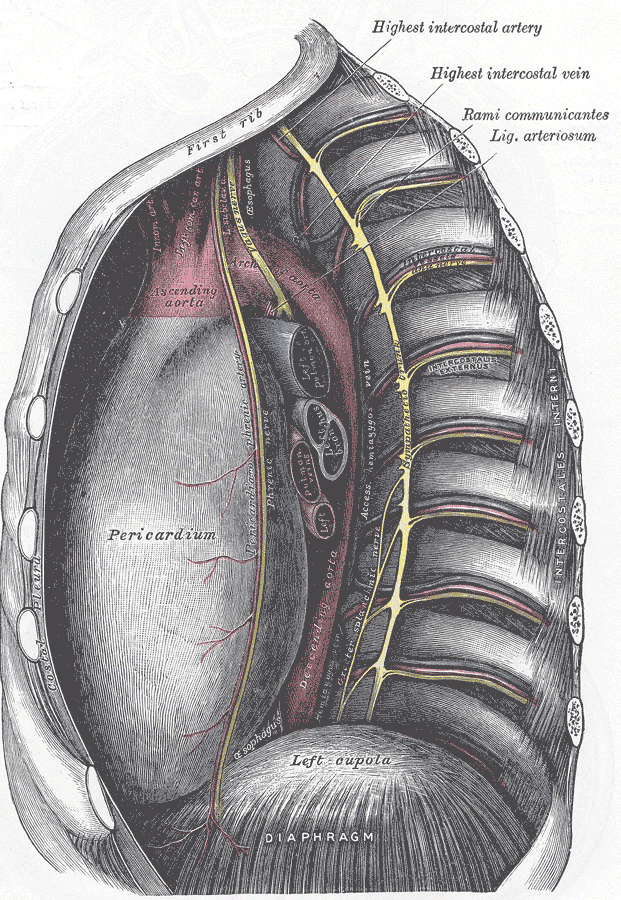
The pericardium and the left cupola of the diaphragm
-
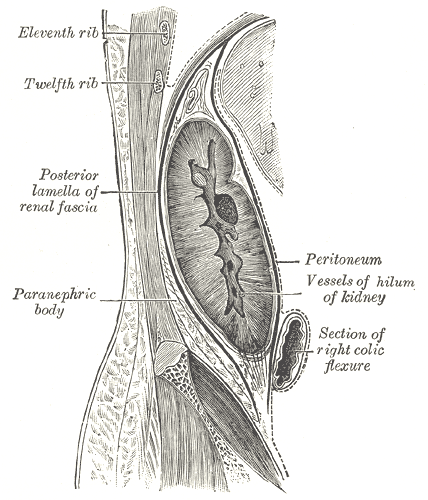
The peritoneum and renal fascia
Fascial dynamics
Fascia is a highly adaptable tissue. Due to its elastic property, superficial fascia can stretch to accommodate the deposition of adipose that accompanies both ordinary and prenatal weight gain. After pregnancy and weight loss, the superficial fascia slowly reverts to its original level of tension.
Visceral fascia is less extensible than superficial fascia. Due to its suspensory role of the organs, it needs to maintain its tone rather consistently. If it is too lax, it contributes to organ prolapse, yet if it is hypertonic, it restricts proper organ motility. [7]
Deep fascia is also less extensible than superficial fascia. It is essentially avascular [8], but is richly innervated with sensory receptors that report the presence of pain (nociceptors); change in movement (proprioceptors); change in pressure and vibration (mechanoreceptors); change in the chemical milieu (chemoreceptors); and fluctuation in temperature (thermoreceptors). [9], [10] Deep fascia is able to respond to sensory input by contracting; by relaxing; or by adding, reducing, or changing its composition through the process of fascial remodeling. [11]
Deep fascia can contract. What happens during the fight-or-flight response is an example of rapid fascial contraction . In response to a real or imagined threat to the organism, the body responds with a temporary increase in the stiffness of the fascia. Bolstered with tensioned fascia, people are able to perform extraordinary feats of strength and speed under emergency conditions. [12] How fascia contracts is still not well understood, but appears to involve the activity of myofibroblasts. Myofibroblasts are fascial cells that are created as a response to mechanical stress. In a two step process, fibroblasts differentiate into proto-myofibroblasts that with continued mechanical stress, become differentiated myofibroblasts. [13] Fibroblasts cannot contract, but myofibroblasts are able to contract in a smooth muscle-like manner. [14]
The deep fascia can also relax. By monitoring changes in muscular tension, joint position, rate of movement, pressure, and vibration, mechanoreceptors in the deep fascia are capable of initiating relaxation. Deep fascia can relax rapidly in response to sudden muscular overload or rapid movements. Golgi tendon organs operate as a feedback mechanism by causing myofascial relaxation before muscle force becomes so great that tendons might be torn. Pacinian corpuscles sense changes in pressure and vibration to monitor the rate of acceleration of movement. They will intiate a sudden relaxatory response if movement happens too fast. [15] Deep fascia can also relax slowly as some mechanoreceptors are designed to report changes over a longer period of time. Unlike the Golgi tendon organs, Golgi receptors report joint position independent of muscle contraction. This helps the body to know where the bones are at any given moment. Ruffini endings respond to regular stretching and to slow sustained pressure. In addition to initiating fascial relaxation, they contribute to full-body relaxation by inhibiting sympathetic activity which slows down heart rate and respiration. [16] [17]
When contraction persists, fascia will respond with the addition of new material. Fibroblasts secrete collagen and other proteins into the extracellular matrix where they bind to existing proteins, making the composition thicker and less extensible. Although this potentiates the tensile strength of the fascia, it can unfortunately restrict the very structures it aims to protect. The pathologies resulting from fascial restrictions range from a mild decrease in joint range of motion to severe fascial binding of muscles, nerves and blood vessels, as in compartment syndrome of the leg. However, if fascial contraction can be interrupted long enough, a reverse form of fascial remodeling occurs. The fascia will normalize its composition and tone and the extra material that was generated by prolonged contraction will be ingested by macrophages within the extracellular matrix. [18]
Like mechanoreceptors, chemoreceptors in deep fascia also have the ability to promote fascial relaxation. We tend to think of relaxation as a good thing, however fascia needs to maintain some degree of tension. This is especially true of ligaments. To maintain joint integrity, they need to provide adequate tension between bony surfaces. If a ligament is too lax, injury becomes more likely. Certain chemicals, including hormones, can influence the composition of the ligaments. An example of this is seen in the menstrual cycle, where hormones are secreted to create changes in the uterine and pelvic floor fascia. The hormones are not site-specific, however, and chemoreceptors in other ligaments of the body can be receptive to them as well. The ligaments of the knee may be one of the areas where this happens, as a significant association between the ovulatory phase of the menstrual cycle and an increased likelihood for an anterior cruciate ligament injury has been demonstrated. [19] [20]
It has been suggested that manipulation of the fascia by acupuncture needles is responsible for the physical sensation of qi flowing along meridians in the body.[21]
Fascial pathology
- Adhesions
- Adhesive capsulitis
- Benign joint hypermobility syndrome
- Calcific tendinitis
- Cardiac tamponade
- Carpal Tunnel Syndrome
- Cellulitis
- Compartment syndrome
- Constrictive pericarditis
- Dermatomyositis
- Dupuytren's contracture
- Ehlers-Danlos syndrome
- Eosinophilic fasciitis
- Fibromyalgia
- Hemopneumothorax
- Hemothorax
- Hernia
- Marfan's syndrome
- Meningitis
- Mixed connective tissue disease
- Myofascial pain syndrome
- Necrotizing fasciitis
- Pericardial effusion
- Pericarditis
- Peritonitis
- Plantar fasciitis
- Pleural effusion
- Pleurisy
- Pneumoperitoneum
- Pneumothorax
- Polyarteritis nodosa
- Rheumatoid arthritis
- Scars
- Scleroderma
- Scoliosis
- Sprain
- Systemic lupus erythematosus
- Tendinitis
- Wegener's granulomatosis
Classification by region
[22], [23], [24], [25], [26], [27], [28], [29]
References
- ↑ Paoletti, Serge (2006). The Fasciae: Anatomy, Dysfunction & Treatment. Seattle, WA: Eastland Press. pp. 151–161. ISBN 0-939616-53-X.
- ↑ Skandalakis, John E. (2002). Surgical Anatomy and Technique, 2nd Ed. Atlanta, GA: Springer. pp. 1–2. ISBN 0-38798-752-5. Unknown parameter
|coauthors=ignored (help) - ↑ Paoletti, Serge (2006). The Fasciae: Anatomy, Dysfunction & Treatment. Seattle, WA: Eastland Press. pp. 23–24. ISBN 0-939616-53-X.
- ↑ Hedley, Gil (2005). The Integral Anatomy Series Vol. 1: Skin and Superficial fascia (DVD). Integral Anatomy Productions.
- ↑ Hedley, Gil (2005). The Integral Anatomy Series Vol. 2: Deep Fascia and Muscle (DVD). Integral Anatomy Productions.
- ↑ Hedley, Gil (2005). The Integral Anatomy Series Vol. 3: Cranial and Visceral Fasciae (DVD). Integral Anatomy Productions.
- ↑ Paoletti, Serge (2006). The Fasciae: Anatomy, Dysfunction & Treatment. Seattle, WA: Eastland Press. pp. 146–147. ISBN 0-939616-53-X.
- ↑ Rolf, Ida P. (1989). Rolfing. Rochester, VT: Healing Arts Press. p. 38. ISBN 0-89281-335-0.
- ↑ Chaitow, Leon (1988). Soft Tissue Manipulation. Rochester, VT: Healing Arts Press. pp. 26–28. ISBN 0-89281-276-1.
- ↑ Schleip, R. (2003). "Fascial plasticity – a new neurobiological explanation: Part 1". Journal of Bodywork and Movement Therapies. Elsevier. 7 (1): 15–19.
- ↑ Myers, Thomas W. (2002). Anatomy Trains. London, UK: Churchill Livingstone. p. 15. ISBN 0-443-06351-6.
- ↑ Schleip, R. (2005). "Active fascial contractility: Fascia may be able to contract in a smooth muscle-like manner and thereby influence musculoskeletal dynamics". Medical Hypotheses. Elsevier. 65: 274. Unknown parameter
|coauthors=ignored (help) - ↑ Tomasek, J. (2002). "Myofibroblasts and Mechanoregulation of Connective Tissue Remodelling". Molecular Cell Biology. Nature Publishing Group. 3: 350–352. Unknown parameter
|coauthors=ignored (help) - ↑ Schleip, R. (2005). "Active fascial contractility: Fascia may be able to contract in a smooth muscle-like manner and thereby influence musculoskeletal dynamics". Medical Hypotheses. Elsevier. 65: 273–277. Unknown parameter
|coauthors=ignored (help) - ↑ Chaitow, Leon (1988). Soft Tissue Manipulation. Rochester, VT: Healing Arts Press. pp. 26–27. ISBN 0-89281-276-1.
- ↑ Schleip, R. (2003). "Fascial plasticity – a new neurobiological explanation: Part 1". Journal of Bodywork and Movement Therapies. Elsevier. 7 (1): 11–19.
- ↑ Schleip, R. (2003). "Fascial plasticity – a new neurobiological explanation: Part 2". Journal of Bodywork and Movement Therapies. Elsevier. 7 (2): 104–116.
- ↑ Paoletti, Serge (2006). The Fasciae: Anatomy, Dysfunction & Treatment. Seattle, WA: Eastland Press. pp. 138, 147–149. ISBN 0-939616-53-X.
- ↑ Wojtys, E. (1998). "Association Between the Menstrual Cycle and Anterior Cruciate Ligament Injuries in Female Athletes". American Journal of Sports Medicine. American Orthopaedic Society for Sports Medicine. 26: 614–619. Unknown parameter
|coauthors=ignored (help) - ↑ Heitz, N. (1999). "Hormonal Changes Throughout the Menstrual Cycle and Increased Anterior Cruciate Ligament Laxity in Females". Journal of Athletic Training. National Athletic Trainers Association. 32 (2): 144–149. Unknown parameter
|coauthors=ignored (help) - ↑ Kimura M, Tohya K, Kuroiwa K, Oda H, Gorawski EC, Hua ZX, Toda S, Ohnishi M, Noguchi E. “Electron microscopical and immunohistochemical studies on the induction of "Qi" employing needling manipulation.” Am J Chin Med. 1992;20(1):25-35.
- ↑ "Dorlands Medical Dictionary - aponeuroses". Merck Source.
- ↑ "Dorlands Medical Dictionary - fasciae". Merck Source.
- ↑ "Dorlands Medical Dictionary - ligaments". Merck Source.
- ↑ "Dorlands Medical Dictionary - membranes". Merck Source.
- ↑ "Dorlands Medical Dictionary - tendons". Merck Source.
- ↑ "Fasciae and Aponeuroses - Organized by Region". Department of Anatomy, University of Arkansas for Medical Sciences.
- ↑ "Fascia of the Head and Neck". Department of Gross Anatomy at Tufts University.
- ↑ "Viscera and Fascia Tables". The University of Michigan - Medical Gross Anatomy.
See also
External links
de:Faszie
nl:Fascie (bindweefsel)
sv:Fascia
tl:Fascia