Burosumab
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Yashasvi Aryaputra[2], Anmol Pitliya, M.B.B.S. M.D.[3]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Burosumab is a fibroblast growth factor 23 (FGF23) blocking antibody that is FDA approved for the treatment of X-linked hypophosphatemia (XLH) in adult and pediatric patients 1 year of age and older. Common adverse reactions include headache, injection site reaction, vomiting, pyrexia, pain in extremity, vitamin D decreased.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications:
- Burosumab is indicated for the treatment of X-linked hypophosphatemia (XLH) in adult and pediatric patients 1 year of age and older.
Adult Patients with X-linked Hypophosphatemia (18 years of age and older)
- The recommended dose regimen in adults is 1 mg/kg body weight, rounded to the nearest 10 mg up to a maximum dose of 90 mg, administered every four weeks.
- After initiation of treatment with burosumab, assess fasting serum phosphorus on a monthly basis, measured 2 weeks post-dose, for the first 3 months of treatment, and thereafter as appropriate. If serum phosphorus is within the normal range, continue with the same dose.
Dose Decrease
- Reassess fasting serum phosphorus level 2 weeks after dose adjustment.
- Do not adjust burosumab more frequently than every 4 weeks.
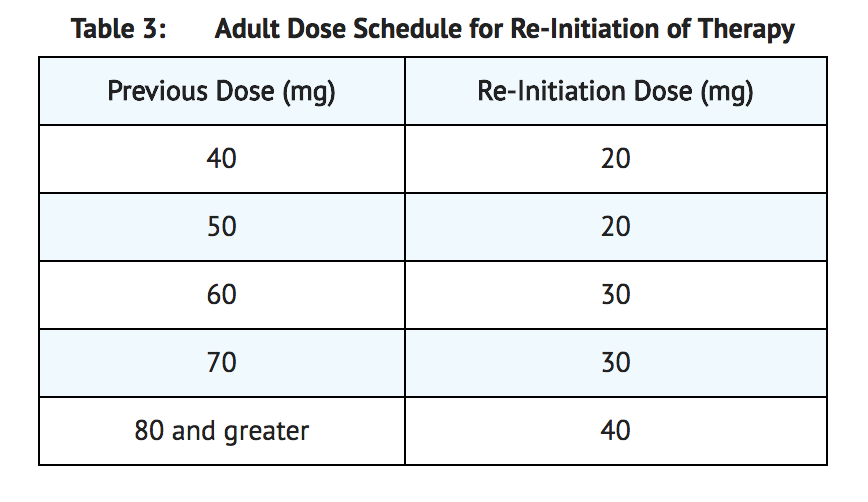
- If serum phosphorus is above the normal range, withhold the next dose and reassess the serum phosphorus level after 4 weeks. The patient must have serum phosphorus below the normal range to be able to reinitiate burosumab. Once serum phosphorus is below the normal range, treatment may be restarted at approximately half the initial starting dose up to a maximum dose of 40 mg every 4 weeks according to the dose schedule shown in Table 3. Reassess serum phosphorus 2 weeks after any change in dose.
Missed Dose
- If a patient misses a dose, resume burosumab as soon as possible at the prescribed dose.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding burosumab Off-Label Guideline-Supported Use and Dosage (Adult) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding burosumab Off-Label Non-Guideline-Supported Use and Dosage (Adult) in the drug label.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Indications:
- Burosumab is indicated for the treatment of X-linked hypophosphatemia (XLH) in adult and pediatric patients 1 year of age and older.
Pediatric Patients with X-linked Hypophosphatemia (1 to less than 18 years of age)
- The recommended starting dose regimen is 0.8 mg/kg of body weight, rounded to the nearest 10 mg, administered every two weeks. The minimum starting dose is 10 mg up to a maximum dose of 90 mg.
- After initiation of treatment with burosumab, measure fasting serum phosphorus every 4 weeks for the first 3 months of treatment, and thereafter as appropriate. If serum phosphorus is above the lower limit of the reference range for age and below 5 mg/dL, continue treatment with the same dose. Follow dose adjustment schedule below to maintain serum phosphorus within the reference range for age.
Dose Adjustment
- Reassess fasting serum phosphorus level 4 weeks after dose adjustment.
- Do not adjust burosumab more frequently than every 4 weeks.
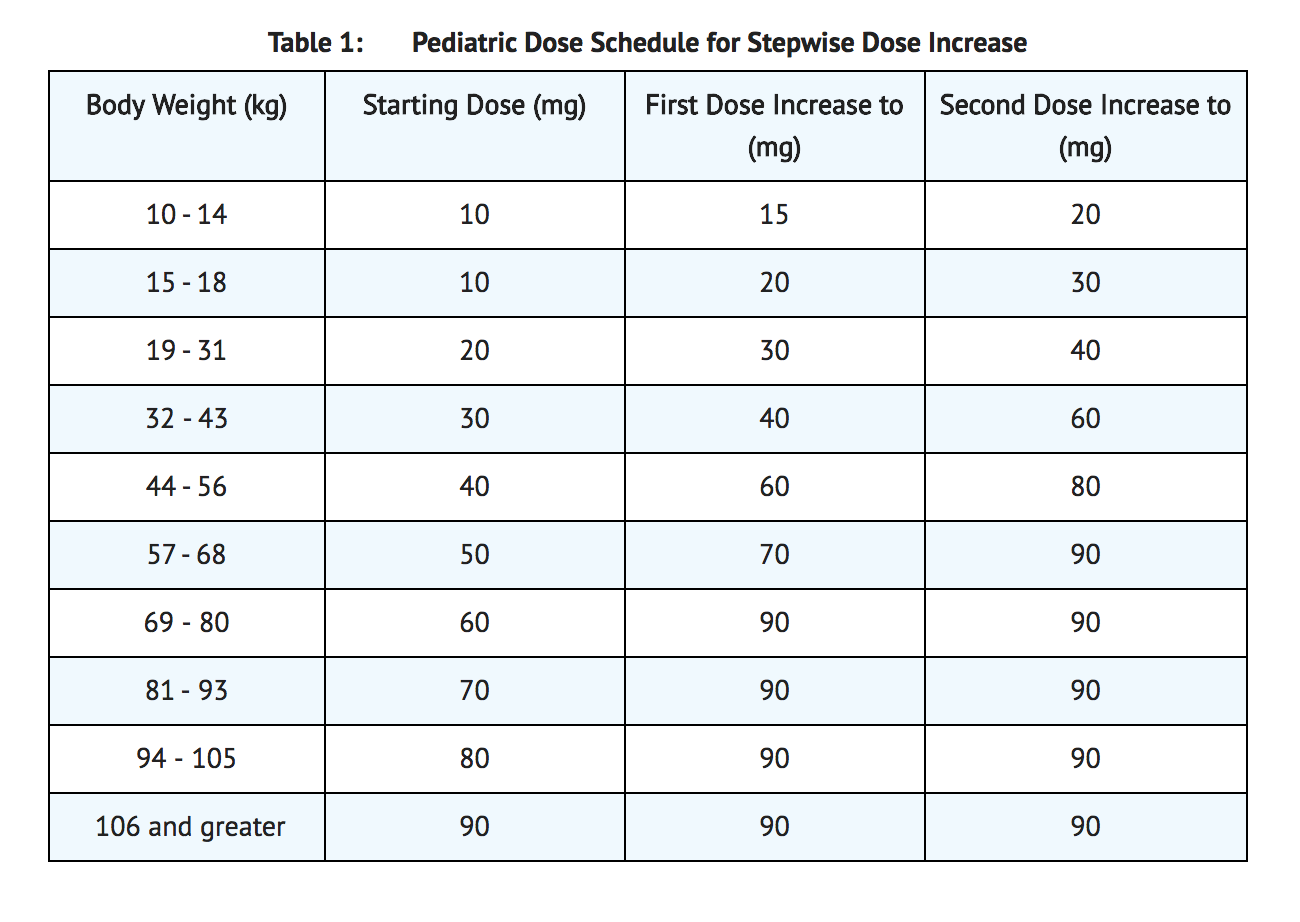
- Dose Increase: If serum phosphorus is below the reference range for age, the dose may be increased stepwise up to approximately 2 mg/kg, administered every two weeks (maximum dose of 90 mg) according to the dosing schedule shown in Table 1.
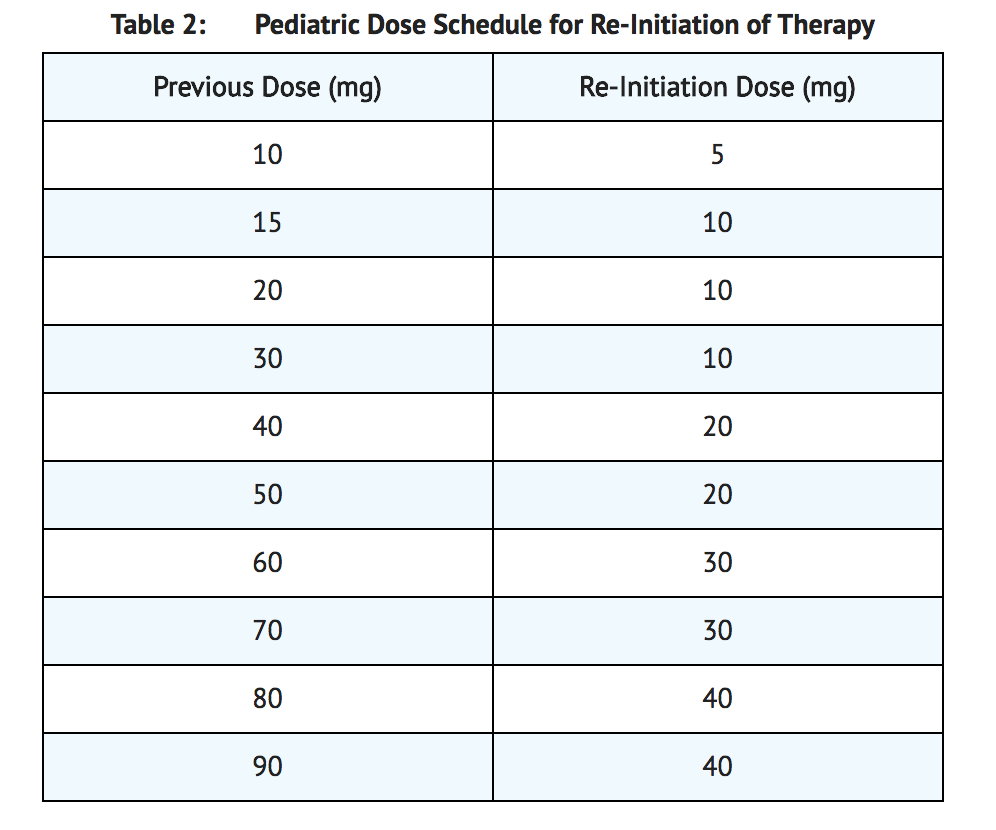
- Dose Decrease: If serum phosphorus is above 5 mg/dL, withhold the next dose and reassess the serum phosphorus level in 4 weeks. The patient must have serum phosphorus below the reference range for age to reinitiate burosumab. Once serum phosphorus is below the reference range for age, treatment may be restarted according to the dose schedule shown in Table 2. Reassess serum phosphorus level 4 weeks after dose adjustment. If the level remains below the reference range for age after the re-initiation dose, the dose can be adjusted according to Table 1.
Missed Dose
- If a patient misses a dose, resume burosumab as soon as possible at the prescribed dose.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding burosumab Off-Label Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding burosumab Off-Label Non-Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Contraindications
- Do not use burosumab with oral phosphate and active vitamin D analogs.
- Do not initiate burosumab treatment if serum phosphorus is within or above the normal range for age.
- Burosumab is contraindicated in patients with severe renal impairment or end stage renal disease because these conditions are associated with abnormal mineral metabolism.
Warnings
Hypersensitivity
- Hypersensitivity reactions (e.g. rash, urticaria) have been reported in patients with burosumab. Discontinue burosumab if serious hypersensitivity reactions occur and initiate appropriate medical treatment.
Hyperphosphatemia and Risk of Nephrocalcinosis
- Increases in serum phosphorus to above the upper limit of normal may be associated with an increased risk of nephrocalcinosis. For patients already taking burosumab, dose interruption and/or dose reduction may be required based on a patient’s serum phosphorus levels.
Injection Site Reactions
- Administration of burosumab may result in local injection site reactions. Discontinue burosumab if severe injection site reactions occur and administer appropriate medical treatment.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
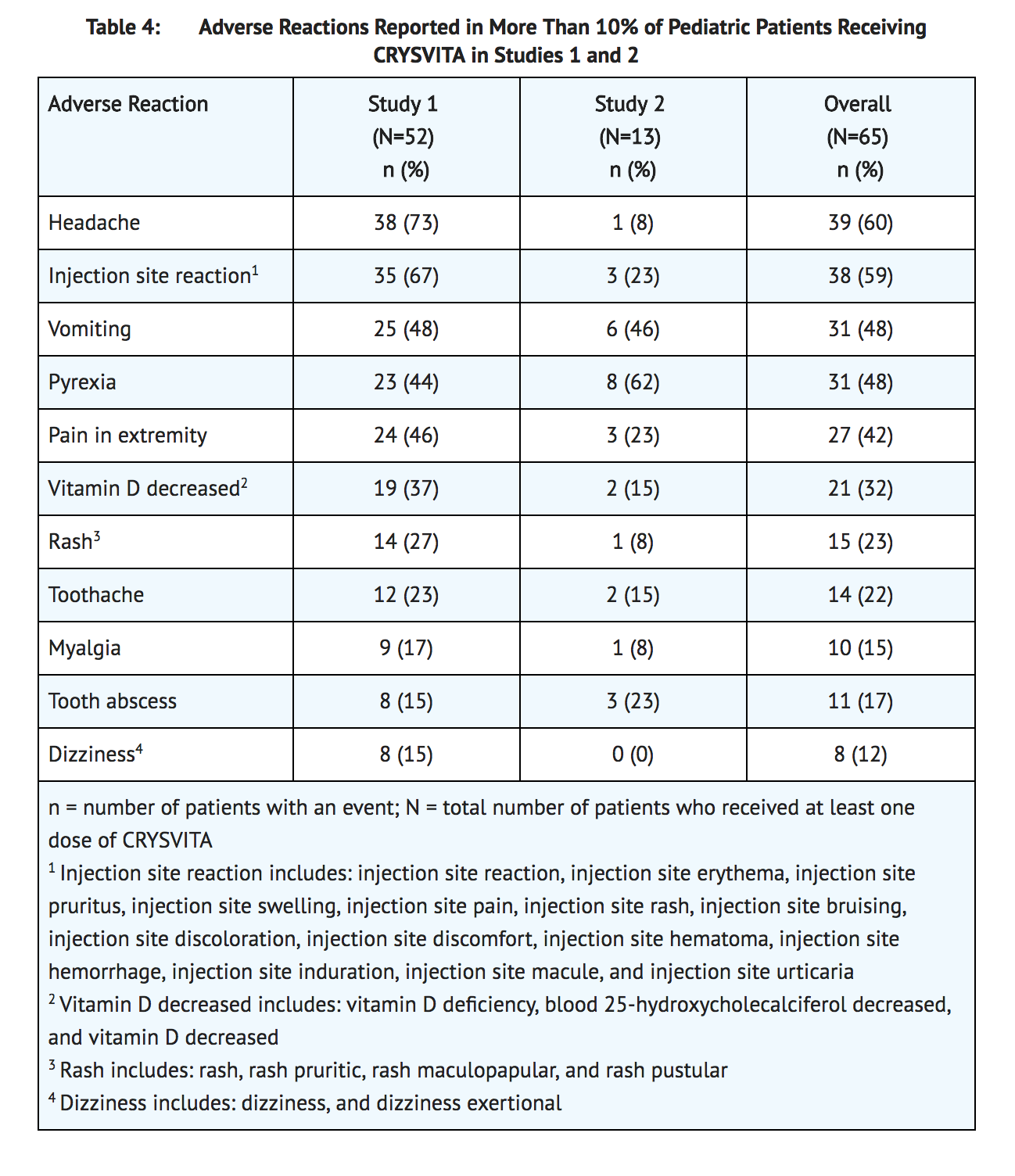
Adverse Reactions in Pediatric Patients with XLH
- The safety data described below reflect exposure to burosumab in 65 pediatric XLH patients that included 52 exposed for at least 64 weeks (Study 1) and 13 exposed for at least 40 weeks (Study 2). Overall, pediatric XLH patients have been exposed to burosumab for a mean duration of 108 weeks (min 40.9, max 150.0). Burosumab was studied in two pediatric open-label phase 2 studies (Study 1, ages 5 to 12 years, n = 52; Study 2, ages ≥ 1 to < 5 years, n = 13). Overall, the patient population was 1-12 years (mean age 7.4 years), 51% male, and 89% white/Caucasian and diagnosed with XLH. In Study 1, 26 of the patients received burosumab at a mean dose of 1.05 mg/kg (range 0.4 – 2.0 mg/kg) every 2 weeks at Week 64; the other 26 patients received burosumab every 4 weeks. In Study 2, patients received burosumab at a mean dose of 0.89 mg/kg (range 0.8 – 1.2 mg/kg) every 2 weeks at Week 40. Adverse reactions reported in more than 10% of burosumab-treated patients from Studies 1 and 2 are shown in Table 4.
Hypersensitivity Reactions
- In pediatric patients, the most frequent potential hypersensitivity events were rash (22%), injection site rash (6%), and urticaria (5%).
Hyperphosphatemia
- In pediatric studies, there were no events of hyperphosphatemia reported.
Injection Site Reactions (ISR)
- In pediatric studies, approximately 58% of the patients had a local reaction (e.g. injection site urticaria, erythema, rash, swelling, bruising, pain, pruritus, and hematoma) at the site of burosumab injection. Injection site reactions were generally mild in severity, occurred within 1 day of injection, lasted approximately 1 to 3 days, required no treatment, and resolved in almost all instances.
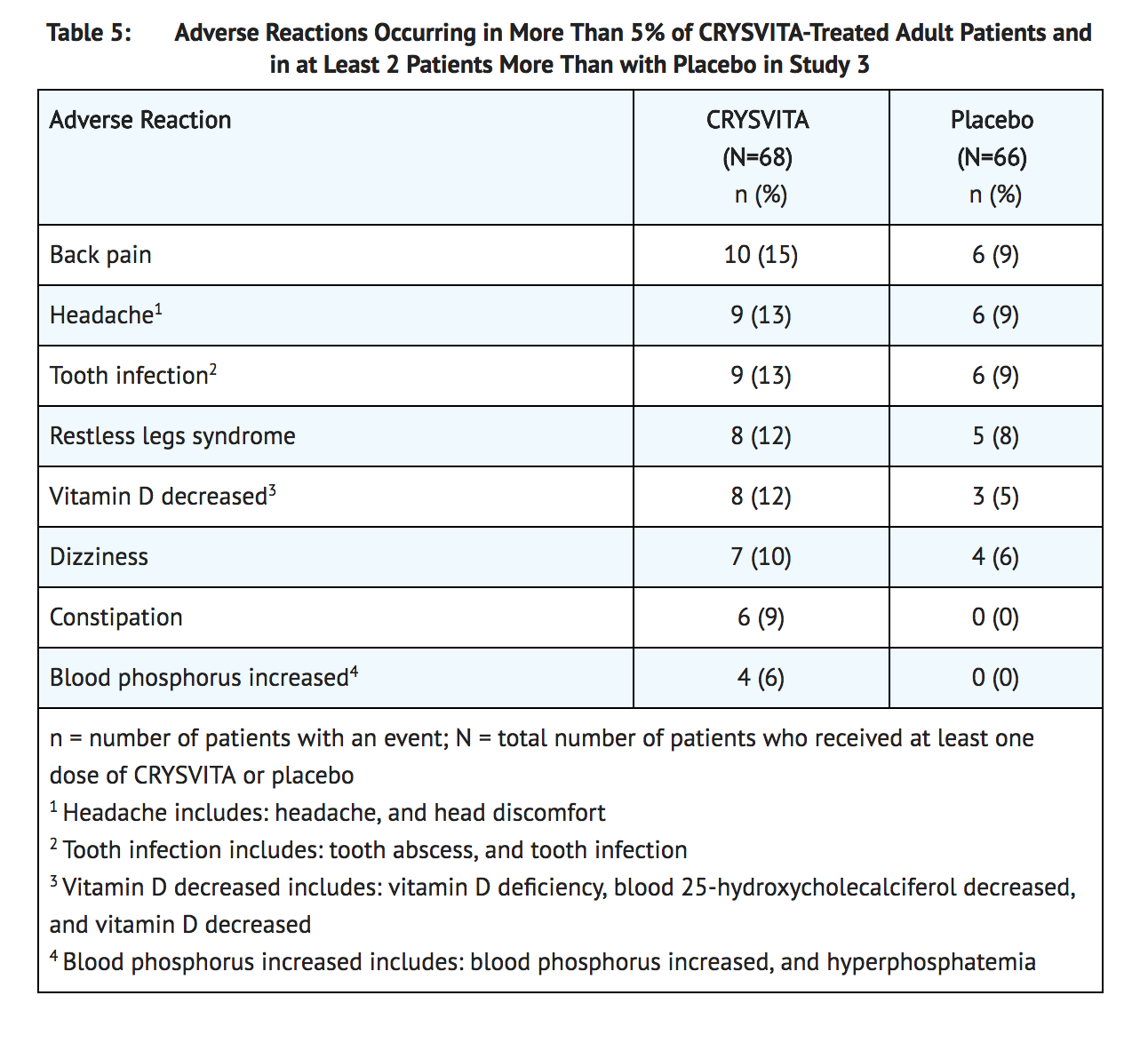
Adverse Reactions in Adult Patients with XLH
- The safety data described below reflect exposure to burosumab in 68 adult XLH patients, age 20-63 years (mean age 41 years), of whom most were white/Caucasian (81%) and female (65%). These patients were enrolled in a randomized, double-blind, placebo-controlled Phase 3 study in adults with XLH (Study 3: burosumab = 68, Placebo = 66), in which patients received burosumab at a mean dose of 0.95 mg/kg (range 0.3 – 1.2 mg/kg) subcutaneously every 4 weeks at Week 24. Adverse reactions reported in more than 5% of burosumab-treated patients and 2 patients or more than with placebo from the 24-week placebo-controlled portion of Study 3 are shown in Table 5.
Hypersensitivity Reactions
- In the double-blind period of Study 3, approximately 6% of patients in both the burosumab and placebo treatment groups experienced a hypersensitivity event. The events were mild or moderate and did not require discontinuation.
Hyperphosphatemia
- In the double-blind period of Study 3, 7% of patients in the burosumab treatment group experienced hyperphosphatemia meeting the protocol-specified criteria for dose reduction (either a single serum phosphorus greater than 5.0 mg/dL or serum phosphorus greater than 4.5 mg/dL [the upper limit of normal] on two occasions). The hyperphosphatemia was managed with dose reduction. The dose for all patients meeting the protocol-specified criteria was reduced 50 percent. A single patient required a second dose reduction for continued hyperphosphatemia.
Injection Site Reactions (ISR)
- In the double-blind period of Study 3, approximately 12% of patients in both the burosumab and placebo treatment groups had a local reaction (e.g. injection site reaction, erythema, rash, bruising, pain, pruritus, and hematoma) at the site of the injection. Injection site reactions were generally mild in severity, occurred within 1 day of injection, lasted approximately 1 to 3 days, required no treatment, and resolved in almost all instances.
Restless Leg Syndrome (RLS)
- In the double-blind period of Study 3, approximately 12% of the burosumab treatment group had worsening of baseline restless leg syndrome (RLS) or new onset RLS of mild to moderate severity; these events did not lead to dose discontinuation. Nonserious RLS has also been reported in other repeat dose adult XLH studies; in one case, worsening baseline RLS led to drug discontinuation and subsequent resolution of the event.
Spinal Stenosis
- Spinal stenosis is prevalent in adults with XLH and spinal cord compression has been reported. In the burosumab phase 2 and phase 3 studies of adults with XLH (total N=176), a total of 6 patients underwent spinal surgery. Most of these cases appeared to involve progression of a pre-existing spinal stenosis. It is unknown if burosumab therapy exacerbates spinal stenosis or spinal cord compression.
Immunogenicity
- As with all therapeutic proteins, there is potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to burosumab-twza in the studies described below with the incidence of antibodies in other studies or to other products may be misleading.
- Pre-existing anti-drug antibodies (ADA) have been detected in up to 10% of patients in clinical studies. ADA was not detected in patients who were antibody negative at the start of treatment. However, the assay used to measure ADA is subject to interference by serum burosumab-twza, possibly resulting in an underestimation of the incidence of antibody formation. Due to the limitation of the assay conditions, the potential clinical impact of antibodies to burosumab-twza is not known.
Postmarketing Experience
There is limited information regarding Burosumab Postmarketing Experience in the drug label.
Drug Interactions
There is limited information regarding Burosumab Drug Interactions in the drug label.
Use in Specific Populations
Pregnancy
Risk Summary
- There are no available data on burosumab use in pregnant women to inform a drug-associated risk of adverse developmental outcomes. In utero, burosumab-twza exposure in cynomolgus monkeys did not result in teratogenic effects. Adverse effects such as late fetal loss and preterm birth were observed in pregnant cynomolgus monkeys, however, these effects are unlikely to indicate clinical risk because they occurred at a drug exposure that was 64-fold higher, by AUC, than the human exposure at 1 mg/kg every 4 weeks and were accompanied in the non-XLH monkeys by maternal hyperphosphatemia and placental mineralization (see Data). Serum phosphorus levels should be monitored throughout pregnancy. Report pregnancies to the Ultragenyx Adverse Event reporting line at 1-888-756-8657.
- The background risk of major birth defects and miscarriage for the indicated population is unknown; however, the estimated background risk in the U.S. general population of major birth defects is 2% to 4% and of miscarriage is 15% to 20% of clinically recognized pregnancies.
Data (Animal)
- In a reproductive toxicity study in pregnant cynomolgus monkeys without XLH, burosumab-twza was administered intravenously once every two weeks from Day 20 of pregnancy to parturition or cesarean section on Day 133, which includes the period of organogenesis, at doses of 1-, 7- and 64-fold human exposure at the adult human dose of 1 mg/kg every 4 weeks. The treatment did not result in teratogenic effects in fetuses or offspring. An increase in late fetal loss, a shortened gestation period, and an increased incidence of preterm births were observed at 64-fold the human exposure at the adult human dose of 1 mg/kg every 4 weeks, concomitant with maternal hyperphosphatemia and placental mineralization. Burosumab-twza was detected in serum from fetuses indicating transport across the placenta. Hyperphosphatemia but no ectopic mineralization was present in fetuses and offspring of dams exposed to 64-fold human exposure at the 1 mg/kg dose every 4 weeks. Burosumab-twza did not affect pre- and postnatal growth including survivability of the offspring.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Burosumab in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Burosumab during labor and delivery.
Nursing Mothers
Risk Summary
- There is no information regarding the presence of burosumab-twza in human milk, or the effects of burosumab-twza on milk production or the breastfed infant. Maternal IgG is present in breast milk. However, the effects of local gastrointestinal exposure and limited systemic exposure to burosumab-twza in the breastfed infant are unknown. The lack of clinical data during lactation precludes a clear determination of the risk of burosumab to an infant during lactation. Therefore, the developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for burosumab and any potential adverse effects on the breastfed infant from burosumab or from the underlying maternal condition.
Pediatric Use
- Safety and efficacy of burosumab have been established in pediatric patients 1 year and older. Efficacy in pediatric patients 1 year and older with XLH is based on open label studies of 52 pediatric patients 5 to 12 years of age with XLH (Study 1), and in 13 pediatric patients 1 to 4 years of age with XLH (Study 2) evaluating serum phosphorus and radiographic findings. Efficacy in adolescents is supported by studies in pediatric patients less than 13 years of age. Dosing in this age group was derived using modeling and simulation of adult and pediatric PK and PD data.
- Safety and efficacy for burosumab in pediatric patients with XLH below the age of 1 have not been established.
Geriatic Use
- Clinical studies of burosumab did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently from younger patients. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Gender
There is no FDA guidance on the use of Burosumab with respect to specific gender populations.
Race
There is no FDA guidance on the use of Burosumab with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Burosumab in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Burosumab in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Burosumab in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Burosumab in patients who are immunocompromised.
Administration and Monitoring
Administration
General Considerations for Subcutaneous Administration
- Injection sites should be rotated with each injection administered at a different anatomic location (upper arms, upper thighs, buttocks, or any quadrant of abdomen) than the previous injection. Do not inject into moles, scars, or areas where the skin is tender, bruised, red, hard, or not intact. The maximum volume of burosumab per injection site is 1.5 mL. If more than 1.5 mL is required on a given dosing day, the total volume of burosumab should be split and administered at two different injection sites. Monitor for signs of reactions.
- Visually inspect burosumab for particulate matter and discoloration prior to administration. Burosumab is a sterile, preservative-free, clear to slightly opalescent and colorless to pale brown-yellow solution for subcutaneous injection. Do not use if the solution is discolored or cloudy or if the solution contains any particles or foreign particulate matter.
Monitoring
- Clinical improvement of hypophosphatemia may be indicative of efficacy.
- Fasting serum phosphorus level: Prior to therapy initiation in all patients.
- Fasting serum phosphorus level: Every 4 weeks for the first 3 months and then as clinically indicated in pediatric patients.
- Fasting serum phosphorus level: Monthly, 2 weeks after dose is given, for the first 3 months and then as clinically indicated in adult patients.
- Injection site reactions.
IV Compatibility
There is limited information regarding the compatibility of Burosumab and IV administrations.
Overdosage
- There have been no reports of overdose with burosumab. Burosumab has been administered in pediatric clinical trials without dose limiting toxicity using doses up to 2 mg/kg body weight with a maximal dose of 90 mg, administered every two weeks. In adult clinical trials, no dose limiting toxicity has been observed using doses up to 1 mg/kg or a maximal total dose of 128 mg every 4 weeks. In non-XLH rabbits and cynomolgus monkeys, ectopic mineralization in multiple tissues and organs was observed at doses of burosumab-twza that resulted in supra-physiologic serum phosphate levels. Adverse effects on bone including reductions in bone mineral density, bone mineralization and bone strength were also observed at exposure greater than human exposure.
- In case of overdose, it is recommended that serum phosphorus levels, serum calcium levels and renal function be measured immediately and monitored periodically until resolution to normal/baseline levels. In case of hyperphosphatemia, withhold burosumab and initiate appropriate medical treatment.
Pharmacology
Mechanism of Action
- X-linked hypophosphatemia is caused by excess fibroblast growth factor 23 (FGF23) which suppresses renal tubular phosphate reabsorption and the renal production of 1,25 dihydroxy vitamin D. Burosumab-twza binds to and inhibits the biological activity of FGF23 restoring renal phosphate reabsorption and increasing the serum concentration of 1,25 dihydroxy vitamin D.
Structure
There is limited information regarding Burosumab Structure in the drug label.
Pharmacodynamics
- Following SC administration in XLH patients, higher burosumab-twza concentrations were associated with greater increase of serum phosphorus levels. The increase in serum phosphorus was reversible and returned to baseline with elimination of systemic burosumab-twza.
- Ratio of renal tubular maximum reabsorption rate of phosphate to glomerular filtration rate (TmP/GFR) showed dose-dependent increases from baseline.
- Elevation in serum total FGF23 was observed after initiation of burosumab-twza treatment, however, the clinical implication is unknown.
Pharmacokinetics
- The following pharmacokinetic parameters were observed in patients with XLH administered the approved recommended starting dosage based on a 70 kg patient, unless otherwise specified.
- Burosumab-twza exhibited linear pharmacokinetics following SC injections within the dose range of 0.1 to 1 mg/kg (0.08 to 0.8 times the maximum approved recommended dosage based on a 70 kg patient).
- The steady-state trough mean (± SD) concentration of burosumab-twza was 5.8 (± 3.4) mcg/mL in adult patients.
Absorption
- The burosumab-twza mean Tmax values ranged from 8 to 11 days.
Distribution
- The apparent volume of distribution of burosumab-twza is 8 L.
Elimination
- The apparent clearance is 0.290 L/day. The half-life of burosumab-twza is approximately 19 days.
Metabolism
- The exact pathway for burosumab-twza metabolism has not been characterized. Burosumab-twza is expected to be degraded into small peptides and amino acids via catabolic pathways.
Specific Populations
- No clinical significant difference in burosumab-twza pharmacokinetics was observed based on age.
- The effect of renal or hepatic impairment on the pharmacokinetics of burosumab-twza is unknown.
Pediatric Patients
- The steady-state trough concentration was 15.8 (± 9.4) mcg/mL in patients aged 5-12 years, and 11.2 (± 4.6) mcg/mL in patients aged 1-4 years.
Body Weight
- Clearance and volume of distribution of burosumab-twza increases with body weight.
Drug Interaction Studies
- No drug interaction studies have been conducted with burosumab.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- The carcinogenic potential of burosumab-twza has not been evaluated in long term animal studies.
- Studies have not been performed to evaluate the mutagenic potential of burosumab-twza.
- No specific fertility studies have been performed in animals to evaluate the effects of burosumab-twza.
- Toxicology studies with burosumab-twza of up to 40 weeks duration in non-XLH cynomolgus monkeys did not show significant adverse effects on female reproductive organs at doses up to 65-fold human exposure at the dose of 1 mg/kg every 4 weeks. In male monkeys, minimal mineralization of the rete testis or seminiferous tubules associated with hyperphosphatemia was observed at 11- to 37-fold human exposure, but semen analysis did not show any adverse effects.
Animal Toxicology and/or Pharmacology
- In rabbits and cynomolgus monkeys, inhibition of FGF23 signaling by burosumab-twza increased serum phosphate and 1,25 dihydroxy vitamin D. Ectopic mineralization in multiple tissues and organs was observed at doses of burosumab-twza that resulted in supra-physiologic serum phosphate levels in the non-XLH animals. In a study in wild type (WT) and hypophosphatemic Hyp mice, a murine model of XLH, ectopic mineralization was markedly less in Hyp mice.
- In adult cynomolgus monkeys, burosumab-twza increased bone turnover, mineral content and/or mineral density and cortical thickness at 37- to 65-fold human exposure at the dose of 1 mg/kg every 4 weeks. Adverse effects on bone including reductions in bone mineral density, bone mineralization and bone strength were observed in adult male monkeys at 37- to 47-fold human exposure at the dose of 1 mg/kg every 4 weeks.
- In juvenile cynomolgus monkeys, burosumab-twza increased bone turnover, mineral content and/or mineral density and/or cortical thickness at 0.5- to 5-fold clinical pediatric exposure. Bone mineralization was decreased in a male monkey at 5-fold pediatric exposure but there was no effect on bone strength. Burosumab-twza did not affect bone development in juvenile monkeys at doses up to 5-fold pediatric exposure.
Clinical Studies
Pediatric X-linked Hypophosphatemia
- Burosumab has been evaluated in 65 pediatric patients with XLH.
- Study 1 (NCT 02163577) is a randomized, open-label study in 52 prepubescent XLH patients, 5 to 12 years old, which compared treatment with burosumab administered every 2 weeks versus every 4 weeks. Following an initial 16-week dose titration phase, patients completed 48-weeks of treatment with burosumab every 2 weeks. All 52 patients completed at least 64 weeks on study; no patient discontinued. Burosumab-twza dose was adjusted to target a fasting serum phosphorus concentration of 3.5 to 5.0 mg/dL based on the fasting phosphorus level the day of dosing. Twenty-six of 52 patients received burosumab every two weeks up to a maximum dose of 2 mg/kg. The average dose was 0.73 mg/kg (range: 0.3, 1.5) at week 16, 0.98 mg/kg (range: 0.4, 2.0) at week 40 and 1.04 mg/kg (range: 0.4, 2.0) at week 60. The remaining 26 patients received burosumab every four weeks. At study entry, the mean age of patients was 8.5 years and 46% were male. Ninety-six percent had received oral phosphate and active vitamin D analogs for a mean (SD) duration of 7 (2.4) years. Oral phosphate and active vitamin D analogs were discontinued prior to study enrollment. Ninety-four percent of patients had radiographic evidence of rickets at baseline.
- Study 2 (NCT 02750618) is a 64-week open-label study in 13 pediatric XLH patients, 1 to 4 years old. Patients received burosumab at a dose of 0.8 mg/kg every two weeks with titration up to 1.2 mg/kg based on serum phosphorus measurements. All patients completed at least 40 weeks on study; no patients discontinued. At study entry, the mean age of patients was 2.9 years and 69% were male. All patients had radiographic evidence of rickets at baseline and had received oral phosphate and active vitamin D analogs for a mean (SD) duration of 16.9 (13.9) months. Oral phosphate and active vitamin D analogs were discontinued prior to study enrollment.
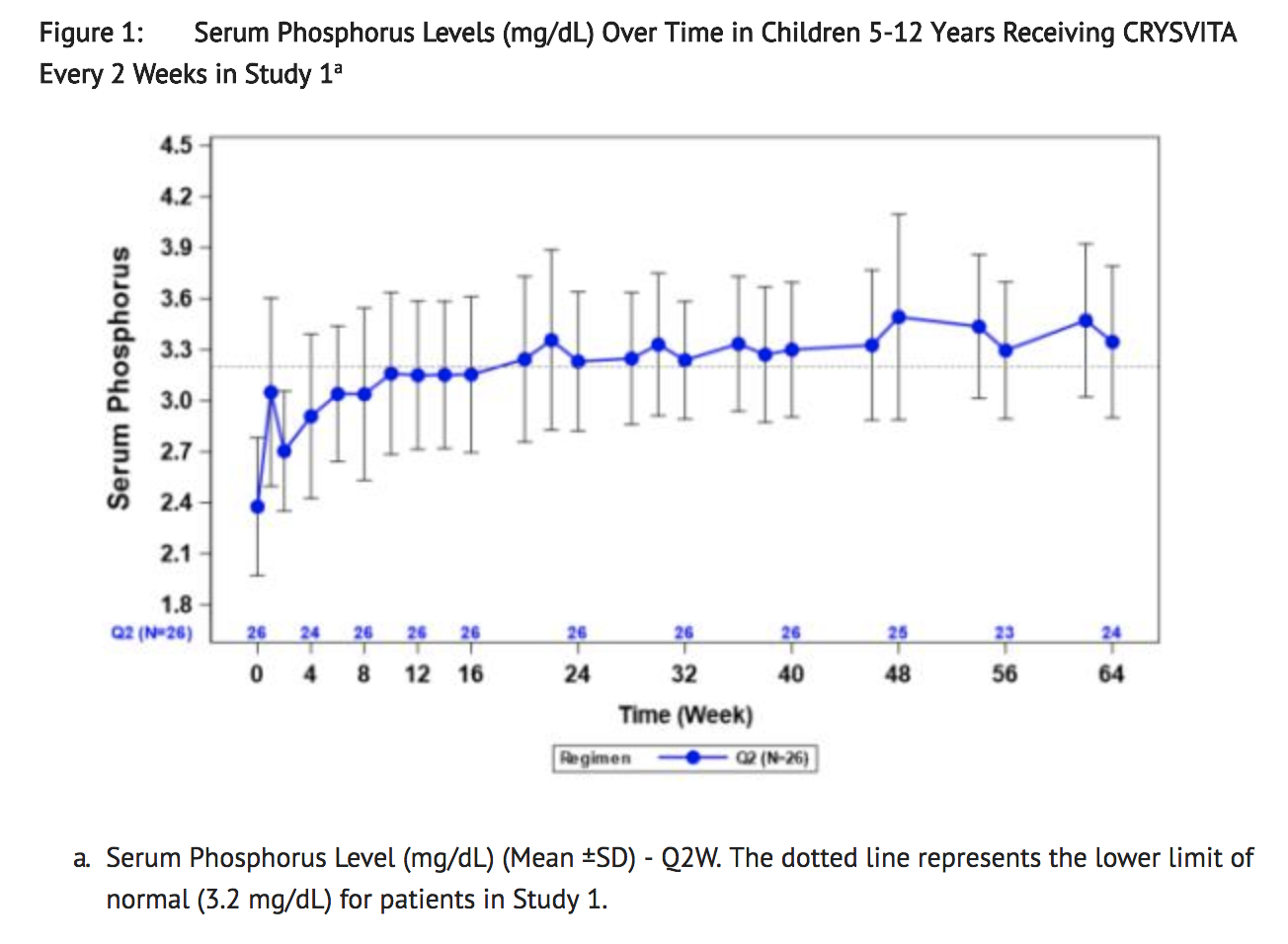
Serum Phosphorus
- In Study 1, burosumab increased mean (SD) serum phosphorus levels from 2.4 (0.40) at baseline to 3.3 (0.40) and 3.4 (0.45) mg/dL at week 40 and week 64 in the patients who received burosumab every 2 weeks (Figure 1). The ratio of renal tubular maximum reabsorption rate of phosphate to glomerular filtration rate (TmP/GFR) increased in these patients from mean (SD) of 2.2 (0.49) at baseline to 3.3 (0.60) and 3.4 (0.53) mg/dL at week 40 and week 64.
- In Study 2, burosumab increased mean (SD) serum phosphorus levels from 2.5 (0.28) mg/dL at baseline to 3.5 (0.49) mg/dL at week 40.
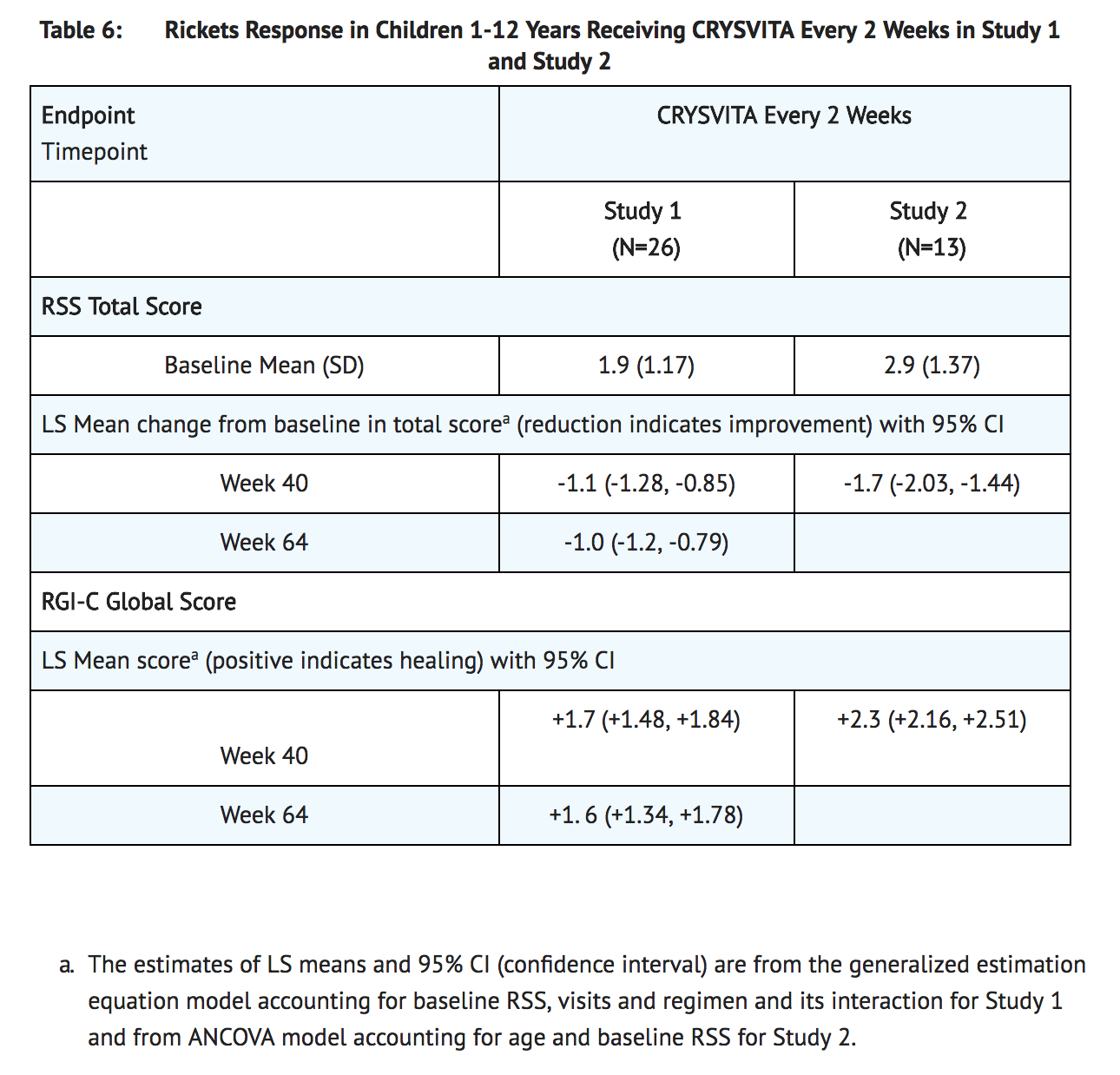
Radiographic Evaluation of Rickets
- Radiographs from 52 burosumab-treated XLH patients in Study 1 and 13 patients in Study 2 were examined to assess XLH-related rickets using the 10-point Thacher Rickets Severity Score (RSS) and the 7-point Radiographic Global Impression of Change (RGI-C). The RSS score is assigned based on images of the wrist and knee from a single timepoint, with higher scores indicating greater rickets severity. The RGI-C score is assigned based on side-by-side comparisons of wrist and knee radiographs from two timepoints, with higher scores indicating greater improvement in radiographic evidence of rickets. A RGI-C score of +2.0 was defined as radiographic evidence of substantial healing.
- In Study 1, baseline mean (SD) RSS total score was 1.9 (1.17) in patients receiving burosumab every two weeks. After 40 weeks of treatment with burosumab, mean total RSS decreased from 1.9 to 0.8 (see Table 6). After 40 weeks of treatment with burosumab, the mean RGI-C Global score was +1.7 in patients receiving burosumab every two weeks. Eighteen out of 26 patients achieved an RGI-C score of ≥ +2.0. These findings were maintained at week 64 as shown in Table 6.
- In Study 2, baseline mean (SD) total RSS was 2.9 (1.37) in 13 patients. After 40 weeks of treatment with burosumab, mean total RSS decreased from 2.9 to 1.2 and the mean (SE) RGI-C Global score was +2.3 (0.08). All 13 patients achieved a RGI-C global score ≥ +2.0. The mean (SE) lower limb deformity as assessed by RGI-C, using standing long leg radiographs, was +1.3 (0.14) (see Table 6).
Serum Alkaline Phosphatase Activity
- For Study 1, mean (SD) serum total alkaline phosphatase activity was 462 (110) U/L at baseline and decreased to 354 (73) U/L at Week 64 (-23%, p < 0.0001) in the patients who received burosumab every 2 weeks.
- For Study 2, mean (SD) serum total alkaline phosphatase activity was 549 (194) U/L at baseline and decreased to 335 (88) U/L at Week 40 (mean change: -36%).
Growth
- In Study 1, burosumab treatment for 64 weeks increased standing mean (SD) height Z score from -1.72 (1.03) at baseline to -1.54 (1.13) in the patients who received burosumab every two weeks (LS mean change of +0.19 (95% CI: 0.09 to 0.29).
Adult X-linked Hypophosphatemia
- Study 3 (NCT 02526160) is a randomized, double-blind, placebo-controlled study in 134 adult XLH patients. The study comprises a 24-week placebo-controlled treatment phase. Burosumab was administered at a dose of 1 mg/kg every 4 weeks. At study entry, the mean age of patients was 40 years (range 19 to 66 years) and 35% were male. All patients had skeletal pain associated with XLH/osteomalacia at baseline. The baseline mean (SD) serum phosphorus concentration was below the lower limit of normal at 1.98 (0.31) mg/dL. Oral phosphate and active vitamin D analogs were not allowed during the study. One patient in the burosumab group discontinued treatment.
- Study 4 (NCT 02537431) is a 48-week, open-label, single-arm study in 14 adult XLH patients to assess the effects of burosumab on improvement of osteomalacia as determined by histologic and histomorphometric evaluation of iliac crest bone biopsies. Patients received 1 mg/kg burosumab every four weeks. At study entry, the mean age of patients was 40 years (range 25 to 52 years) and 43% were male. Oral phosphate and active vitamin D analogs were not allowed during the study.
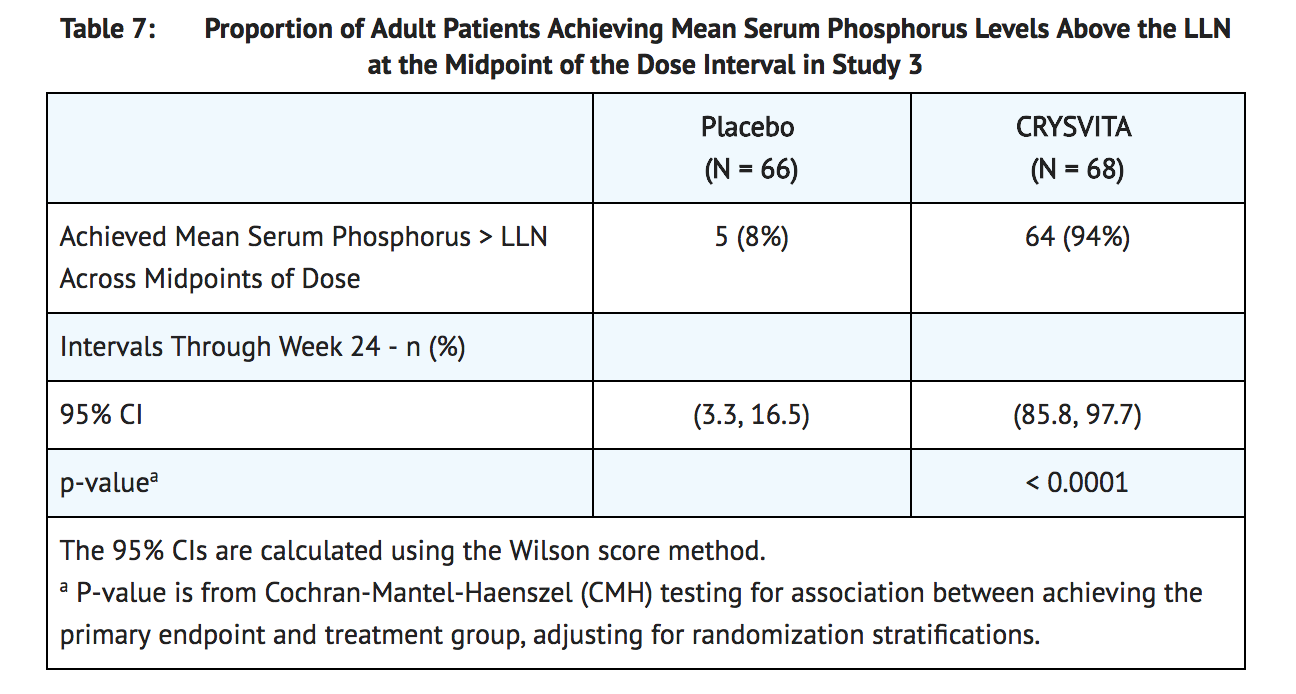
Serum Phosphorus
- In Study 3 at baseline, mean (SD) serum phosphorus was 1.9 (0.32) and 2.0 (0.30) mg/dL in the placebo and burosumab groups respectively. During the initial 24 weeks of treatment, mean (SD) serum phosphorus across the midpoints of dose intervals (2 weeks post dose) was 2.1 (0.30) and 3.2 (0.53) mg/dL in the placebo and burosumab groups, and mean (SD) serum phosphorus across the ends of dose intervals was 2.0 (0.30) and 2.7 (0.45) mg/dL in the placebo and burosumab groups.
- A total of 94% of patients treated with burosumab achieved a serum phosphorus level above the lower limit of normal (LLN) compared to 8% in the placebo group through week 24 (Table 7).
- At baseline, the mean (SD) ratio of renal tubular maximum reabsorption rate of phosphate to glomerular filtration rate (TmP/GFR) was 1.60 (0.37) and 1.68 (0.40) mg/dL in the placebo and burosumab groups respectively. At week 22 (midpoint of a dose interval), mean (SD) TmP/GFR was 1.69 (0.37) and 2.73 (0.75) mg/dL in the placebo and burosumab groups. At week 24 (end of a dose interval), mean (SD) TmP/GFR was 1.73 (0.42) and 2.21 (0.48) mg/dL in the placebo and burosumab groups.
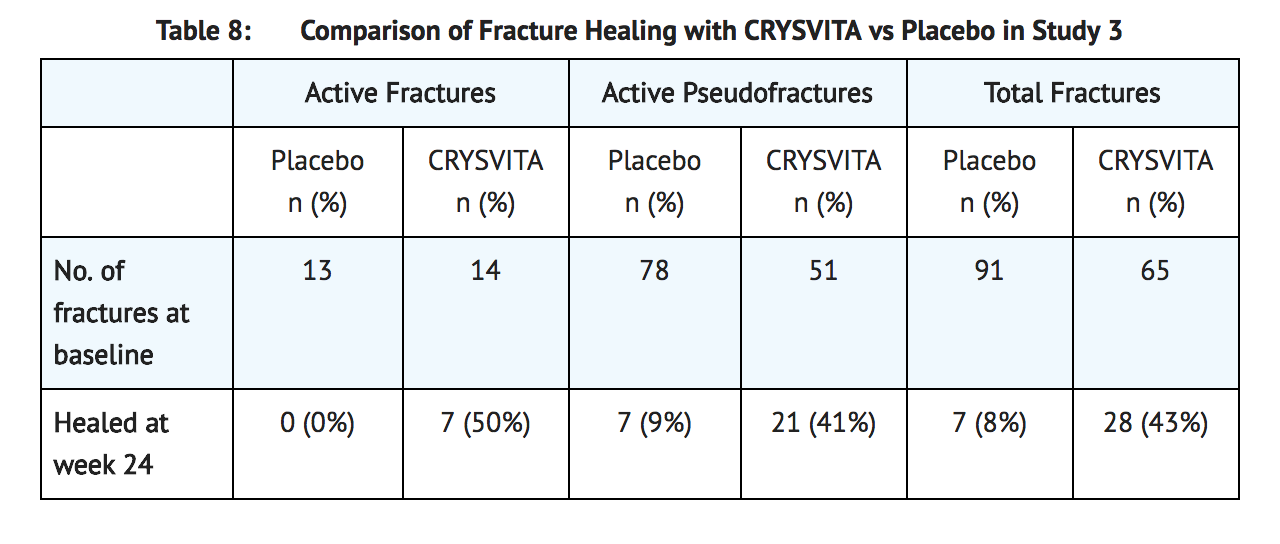
Radiographic Evaluation of Osteomalacia
- In Study 3, a skeletal survey was conducted at baseline to identify osteomalacia-related fractures and pseudofractures. Osteomalacia-related fractures are defined as atraumatic lucencies extending across both bone cortices and pseudofractures are defined as atraumatic lucencies extending across one cortex. There were 52% of patients who had either active (unhealed) fractures (12%) or active pseudofractures (47%) at baseline. The active fractures and pseudofractures were predominantly located in the femurs, tibia/fibula, and metatarsals of the feet. Assessment of these active fracture/pseudofracture sites at week 24 demonstrated a higher rate of complete healing in the burosumab group compared to placebo as shown in Table 8. During treatment through week 24, a total of 6 new fractures or pseudofractures appeared in 68 patients receiving burosumab, compared to 8 new abnormalities in 66 patients receiving placebo.
Bone Histomorphometry
- In Study 4, after 48 weeks of treatment, healing of osteomalacia was observed in ten patients as demonstrated by decreases in Osteoid volume/Bone volume (OV/BV) from a mean (SD) score of 26% (12.4) at baseline to 11% (6.5), a change of -57%. Osteoid thickness (O.Th) declined in eleven patients from a mean (SD) of 17 (4.1) micrometers to 12 (3.1) micrometers, a change of -33%. Mineralization lag time (MLt) declined in 6 patients from a mean (SD) of 594 (675) days to 156 (77) days, a change of -74%.
How Supplied
- Burosumab (burosumab-twza) injection for subcutaneous administration is supplied as a sterile, preservative-free, clear to slightly opalescent and colorless to pale brown-yellow solution. The product is available as one single-dose vial per carton in the following strengths:
- 10 mg/mL (NDC# 69794-102-01).
- 20 mg/mL (NDC# 69794-203-01).
- 30 mg/mL (NDC# 69794-304-01).
Storage
- Burosumab vials must be stored in the original carton until the time of use under refrigerated conditions at 36°F to 46°F (2°C to 8°C). Keep burosumab vial in the original carton to protect from light until time of use.
- Do not freeze or shake burosumab.
- Do not use burosumab beyond the expiration date stamped on the carton.
- Burosumab vials are single-dose only. Discard any unused product.
Images
Drug Images
{{#ask: Page Name::Burosumab |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel

{{#ask: Label Page::Burosumab |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Hypersensitivity Reactions
- Advise patients that burosumab may cause hypersensitivity events such as rash, injection site rash and urticaria. Instruct the patients to contact their physician if such reactions occur.
Injection Site Reactions
- Inform patients that injection site reactions (e.g. erythema, rash, swelling, bruising, pain, pruritus, urticaria, and hematoma) have occurred at the site of burosumab injection. Instruct the patients to contact their physician if such reactions occur.
Restless Leg Syndrome
- Advise patients that burosumab can induce RLS or worsen the symptoms of existing RLS. Instruct the patients to contact their physician if such a reaction occurs.
Pregnancy
- Report pregnancies to the Ultragenyx Adverse Event reporting line at 1-888-756-8657.
Precautions with Alcohol
Alcohol-Burosumab interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
- Crysvita
Look-Alike Drug Names
There is limited information regarding Burosumab Look-Alike Drug Names in the drug label.
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.