Bone infarction
| Bone infarction | |
 | |
|---|---|
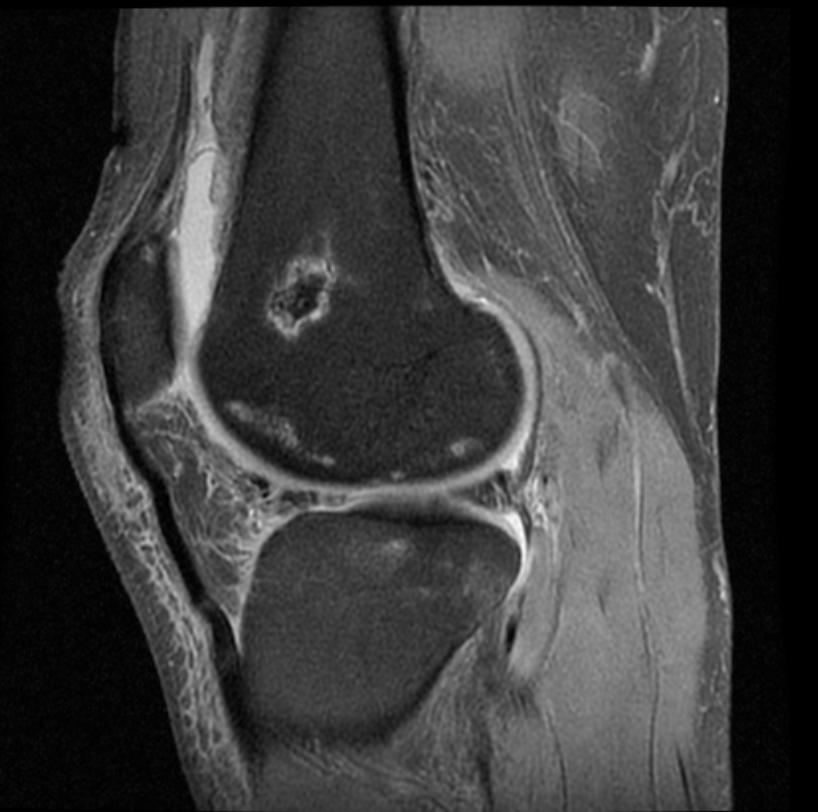
| MRI: Bone infarction (Image courtesy of RadsWiki) |
|
WikiDoc Resources for Bone infarction |
|
Articles |
|---|
|
Most recent articles on Bone infarction Most cited articles on Bone infarction |
|
Media |
|
Powerpoint slides on Bone infarction |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Bone infarction at Clinical Trials.gov Trial results on Bone infarction Clinical Trials on Bone infarction at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Bone infarction NICE Guidance on Bone infarction
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Bone infarction Discussion groups on Bone infarction Patient Handouts on Bone infarction Directions to Hospitals Treating Bone infarction Risk calculators and risk factors for Bone infarction
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Bone infarction |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Risk factors for bone infarcts include steroid use, sickle cell anemia, medications, Gaucher's disease, systemic lupus erythematosis, cancer, organ transplantation and thyroid disease. Osteonecrosis or AVN occurs in 5%–50% of Sistemic Lupus Eritematosus patients and mainly affects weight-bearing joints. It may be attributable to SLE itself or intensified by steroid therapy. This situation is confounding because almost all SLE patients are treated with corticosteroids at some point, although they may be receiving cyclophosphamide, azathioprine, or nonsteroidal anti-inflammatory drugs at the time of presentation. The femoral head is most commonly affected, followed by the humeral head, femoral condyle, and tibial plateau. Radiographs are usually normal in early AVN, and late changes of bone sclerosis indicate the presence of irreversible articular damage. With radiography, a grading system is used to denote the severity of AVN according to the sclerosis, flattening of the articular surface, and joint space abnormalities. This scale ranges from stage 0 (clinically suspected AVN) to stage V (obvious joint space narrowing and articular surface disruption. Two basic factors in bone scintigraphy—hyperemia of the affected bone and osteogenesis—are important in AVN. Unfortunately, hyperemia and osteogenesis are absent in acutely infarcted bone; therefore, early AVN will appear as photopenic areas on technetium-99m methylene diphosphonate bone scans. Within days, recruitment of osteoclasts to resorb necrotic bone and of osteoblasts to build or bridge new bone yields increased radiotracer uptake at the margins of the infarction. In fact, this healing, which occurs gradually, is seen once irreparable articular surface damage has been sustained. Thus, bone scintigraphic findings can be nonspecific as well as reflect more advanced AVN. Prospective studies have demonstrated that MR imaging is superior to and more sensitive than radiography and scintigraphy for documenting early AVN, and MR imaging has been used to document osteonecrosis in asymptomatic SLE patients receiving high-dose corticosteroids. The MR imaging appearance of AVN correlates with the pathophysiologic features of the process. Vascular insufficiency leads to necrosis of different cell types, starting with hematopoietic cells, followed by adipocytes and, finally, osteocytes. Therefore, the earliest MR imaging examination may be normal due to the lack of edema, hemorrhage, or bone marrow response. At this juncture, gadolinium-enhanced MR imaging may demonstrate lack of enhancement of the devascularized areas when the findings at standard spin-echo and short inversion time inversion-recovery imaging are still normal.
Diagnosis
MRI
Initial abnormalities at MR imaging consist of bone marrow edema, which can be extensive even when the area of infarction is small. Over a period of days, reactive changes at the margins of the infarct become visible and manifest as low-signal-intensity areas on standard spin-echo T1- and T2-weighted images. Vascularized granulation tissue just inside the reactive bone manifests with intermediate to high signal intensity on T2-weighted images, producing a line of low signal intensity with an adjacent high-signal-intensity line. Subchondral fractures manifest with high signal intensity on T2-weighted images and are accompanied by fluid signal intensity or edema. Collapse of the articular surface results in loss of the normal spheric contour of bone and incongruity of the articular surfaces. Such collapse usually has low signal intensity on T2-weighted images, a finding that is compatible with fibrotic changes in the infarcted bone marrow. (Images shown below are courtesy of RadsWiki)
Patient#1
-
MRI: Bone infarction
-
MRI: Bone infarction
-
MRI: Bone infarction
-
MRI: Bone infarction
Patient#2