Binimetinib
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Zach Leibowitz [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Binimetinib is a kinase inhibitor that is FDA approved for the treatment of patients, in combination with encorafenib, with unresectable or metastatic melanoma with a BRAF V600E or V600K mutation, as detected by an FDA-approved test. Common adverse reactions include fatigue, nausea, diarrhea, vomiting, and abdominal pain.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indication
- Binimetinib is indicated, in combination with encorafenib, for the treatment of patients with unresectable or metastatic melanoma with a BRAF V600E or V600K mutation, as detected by an FDA-approved test.
Dosage
- The recommended dose is 45 mg orally twice daily in combination with encorafenib. Take binimetinib with or without food.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding binimetinib Off-Label Guideline-Supported Use and Dosage (Adult) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding binimetinib Off-Label Non-Guideline-Supported Use and Dosage (Adult) in the drug label.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
The safety and effectiveness of binimetinib have not been established in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding binimetinib Off-Label Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding binimetinib Off-Label Non-Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Contraindications
None.
Warnings
Cardiomyopathy
- Cardiomyopathy, manifesting as left ventricular dysfunction associated with symptomatic or asymptomatic decreases in ejection fraction, has been reported in patients treated with binimetinib in combination with encorafenib. In COLUMBUS, evidence of cardiomyopathy (decrease in LVEF below the institutional LLN with an absolute decrease in LVEF ≥ 10% below baseline as detected by echocardiography or MUGA) occurred in 7% of patients receiving binimetinib plus encorafenib. Grade 3 left ventricular dysfunction occurred in 1.6% of patients. The median time to first occurrence of left ventricular dysfunction (any grade) in patients receiving binimetinib in combination with encorafenib was 3.6 months (range 0 to 21 months). Cardiomyopathy resolved in 87% of patients receiving binimetinib plus encorafenib.
- Assess ejection fraction by echocardiogram or MUGA scan prior to initiating treatment, one month after initiating treatment, and then every 2 to 3 months during treatment. The safety of binimetinib in combination with encorafenib has not been established in patients with a baseline ejection fraction that is either below 50% or below the institutional lower limit of normal (LLN). Patients with cardiovascular risk factors should be monitored closely when treated with binimetinib.
- Withhold, reduce dose, or permanently discontinue based on severity of adverse reaction.
Venous Thromboembolism
- In COLUMBUS, venous thromboembolism (VTE) occurred in 6% of patients receiving binimetinib in combination with encorafenib, including 3.1% of patients who developed pulmonary embolism. Withhold, reduce dose, or permanently discontinue based on severity of adverse reaction.
Ocular Toxicities
Serous Retinopathy
- In COLUMBUS, serous retinopathy occurred in 20% of patients treated with binimetinib in combination with encorafenib; 8% were retinal detachment and 6% were macular edema. Symptomatic serous retinopathy occurred in 8% of patients with no cases of blindness. No patient discontinued binimetinib due to serous retinopathy; 6% of patients required dose interruptions or dose reductions. The median time to onset of the first event of serous retinopathy (all grades) was 1.2 months (range 0 to 17.5 months).
- Assess for visual symptoms at each visit. Perform an ophthalmologic examination at regular intervals, for new or worsening visual disturbances, and to follow new or persistent ophthalmologic findings. Withhold, reduce dose, or permanently discontinue based on severity of adverse reaction.
Retinal Vein Occlusion
- RVO is a known class-related adverse reaction of MEK inhibitors and may occur in patients treated with binimetinib in combination with encorafenib. In patients with BRAF mutation-positive melanoma receiving binimetinib with encorafenib (n=690), 1 patient experienced RVO (0.1%).
- The safety of binimetinib has not been established in patients with a history of RVO or current risk factors for RVO including uncontrolled glaucoma or a history of hyperviscosity or hypercoagulability syndromes.
- Perform ophthalmologic evaluation for patient-reported acute vision loss or other visual disturbance within 24 hours. Permanently discontinue binimetinib in patients with documented RVO.
Uveitis
- Uveitis, including iritis and iridocyclitis, has been reported in patients treated with binimetinib in combination with encorafenib. In COLUMBUS, the incidence of uveitis among patients treated with binimetinib in combination with encorafenib was 4%.
- Assess for visual symptoms at each visit. Perform an ophthalmologic evaluation at regular intervals and for new or worsening visual disturbances, and to follow new or persistent ophthalmologic findings. Withhold, reduce dose, or permanently discontinue based on severity of adverse reaction.
Interstitial Lung Disease
- In patients with BRAF mutation-positive melanoma receiving binimetinib with encorafenib (n=690), 2 patients (0.3%) developed interstitial lung disease (ILD), including pneumonitis.
- Assess new or progressive unexplained pulmonary symptoms or findings for possible ILD. Withhold, reduce dose, or permanently discontinue based on severity of adverse reaction.
Hepatotoxicity
- Hepatotoxicity can occur when binimetinib is administered in combination with encorafenib. In COLUMBUS, the incidence of Grade 3 or 4 increases in liver function laboratory tests in patients receiving binimetinib in combination with encorafenib was 6% for alanine aminotransferase (ALT), 2.6% for aspartate aminotransferase (AST), and 0.5% for alkaline phosphatase. No patient experienced Grade 3 or 4 serum bilirubin elevation.
- Monitor liver laboratory tests before initiation of binimetinib, monthly during treatment, and as clinically indicated. Withhold, reduce dose, or permanently discontinue based on severity of adverse reaction.
Rhabdomyolysis
- Rhabdomyolysis can occur when binimetinib is administered in combination with encorafenib. In COLUMBUS, elevation of laboratory values of serum CPK occurred in 58% of patients treated with binimetinib in combination with encorafenib. In patients with BRAF mutation-positive melanoma receiving binimetinib with encorafenib (n=690), rhabdomyolysis was reported in 1 patient (0.1%).
- Monitor CPK and creatinine levels prior to initiating binimetinib, periodically during treatment, and as clinically indicated. Withhold, reduce dose, or permanently discontinue based on severity of adverse reaction.
Hemorrhage
- Hemorrhage can occur when binimetinib is administered in combination with encorafenib. In COLUMBUS, hemorrhage occurred in 19% of patients receiving binimetinib in combination with encorafenib. Grade 3 or greater hemorrhage occurred in 3.2% of patients. The most frequent hemorrhagic events were gastrointestinal, including rectal hemorrhage (4.2%), hematochezia (3.1%), and hemorrhoidal hemorrhage (1%). Fatal intracranial hemorrhage in the setting of new or progressive brain metastases occurred in 1.6% of patients.
- Withhold, reduce dose, or permanently discontinue based on severity of adverse reaction.
Embryo-Fetal Toxicity
- Based on findings from animal studies and its mechanism of action, binimetinib can cause fetal harm when administered to a pregnant woman. Binimetinib was embryotoxic and abortifacient when administered to rabbits during the period of organogenesis at doses greater than or equal to those resulting in exposures approximately 5 times the human exposure at the recommended clinical dose of 45 mg twice daily.
- Advise women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with binimetinib and for at least 30 days after the final dose.
Risks Associated with Combination Treatment
- Binimetinib is indicated for use in combination with encorafenib. Refer to the encorafenib prescribing information for additional risk information that applies to combination use treatment.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- The data described in Warnings and Precautions reflect exposure of 192 patients with BRAF V600 mutation-positive unresectable or metastatic melanoma to binimetinib (45 mg twice daily) in combination with encorafenib (450 mg once daily) in a randomized open-label, active-controlled trial (COLUMBUS) or, for rare events, exposure of 690 patients with BRAF V600 mutation-positive melanoma to binimetinib (45 mg twice daily) in combination with encorafenib at doses between 300 mg and 600 mg once daily across multiple clinical trials.
- The data described below reflect exposure of 192 patients with BRAF V600 mutation-positive unresectable or metastatic melanoma to binimetinib (45 mg twice daily) in combination with encorafenib (450 mg once daily) in COLUMBUS.
- The COLUMBUS trial excluded patients with a history of Gilbert's syndrome, abnormal left ventricular ejection fraction, prolonged QTc (> 480 msec), uncontrolled hypertension, and history or current evidence of retinal vein occlusion. The median duration of exposure was 11.8 months for patients treated with binimetinib in combination with encorafenib and 6.2 months for patients treated with vemurafenib.
- The most common (≥ 25%) adverse reactions in patients receiving binimetinib in combination with encorafenib were fatigue, nausea, diarrhea, vomiting, and abdominal pain.
- Adverse reactions leading to dose interruptions of binimetinib occurred in 33% of patients receiving binimetinib in combination with encorafenib; the most common were left ventricular dysfunction (6%) and serous retinopathy (5%). Adverse reactions leading to dose reductions of binimetinib occurred in 19% of patients receiving binimetinib in combination with encorafenib; the most common were left ventricular dysfunction (3%), serous retinopathy (3%), and colitis (2%). Five percent (5%) of patients receiving binimetinib in combination with encorafenib experienced an adverse reaction that resulted in permanent discontinuation of binimetinib. The most common adverse reactions resulting in permanent discontinuation of binimetinib were hemorrhage in 2% and headache in 1% of patients.
- Table 3 and Table 4 present adverse drug reactions and laboratory abnormalities, respectively, identified in COLUMBUS. The COLUMBUS trial was not designed to demonstrate a statistically significant difference in adverse reaction rates for binimetinib in combination with encorafenib, as compared to vemurafenib, for any specific adverse reaction listed in Table 3.

- Other clinically important adverse reactions occurring in < 10% of patients who received binimetinib in combination with encorafenib were:
- Gastrointestinal disorders: Colitis
- Skin and subcutaneous tissue disorders: Panniculitis
- Immune system disorders: Drug hypersensitivity

Postmarketing Experience
There is limited information regarding Binimetinib Postmarketing Experience in the drug label.
Drug Interactions
- No clinically important drug interactions have been observed with binimetinib.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): Risk Summary
- Based on findings from animal reproduction studies and its mechanism of action, binimetinib can cause fetal harm when administered to a pregnant woman. There are no available clinical data on the use of binimetinib during pregnancy. In animal reproduction studies, oral administration of binimetinib during the period of organogenesis was embryotoxic and an abortifacient in rabbits at doses greater than or equal to those resulting in exposures approximately 5 times the human exposure at the clinical dose of 45 mg twice daily. Advise pregnant women of the potential risk to a fetus.
- In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Animal Data
- In reproductive toxicity studies, administration of binimetinib to rats during the period of organogenesis resulted in maternal toxicity, decreased fetal weights and increased variations in ossification at doses ≥ 30 mg/kg/day (approximately 37 times the human exposure based on AUC at the recommended clinical dose of 45 mg twice daily). In pregnant rabbits, administration of binimetinib during the period of organogenesis resulted in maternal toxicity, decreased fetal body weights, an increase in malformations, and increased post-implantation loss, including total loss of pregnancy at doses ≥ 10 mg/kg/day (approximately 5 times the human exposure based on AUC at the recommended clinical dose of 45 mg twice daily). There was a significant increase in fetal ventricular septal defects and pulmonary trunk alterations at 20 mg/kg/day of binimetinib (less than 8 times the human exposure at the recommended clinical dose of 45 mg twice daily).
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Binimetinib in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Binimetinib during labor and delivery.
Nursing Mothers
Risk Summary
- There are no data on the presence of binimetinib or its active metabolite in human milk, or the effects of binimetinib on the breastfed infant, or on milk production. Because of the potential for serious adverse reactions from binimetinib in breastfed infants, advise women not to breastfeed during treatment with binimetinib and for 3 days after the final dose.
Pediatric Use
- The safety and effectiveness of binimetinib have not been established in pediatric patients.
Geriatic Use
- Of the 690 patients with BRAF mutation-positive melanoma who received binimetinib (45 mg twice daily) in combination with encorafenib at doses between 300 mg and 600 mg once daily across multiple clinical trials, 20% were aged 65 to 74 years and 8% were aged 75 years and older. No overall differences in the safety or effectiveness of binimetinib plus encorafenib were observed in elderly patients as compared to younger patients.
Gender
There is no FDA guidance on the use of Binimetinib with respect to specific gender populations.
Race
There is no FDA guidance on the use of Binimetinib with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Binimetinib in patients with renal impairment.
Hepatic Impairment
- Binimetinib concentrations may increase in patients with moderate or severe hepatic impairment. Dose adjustment for binimetinib is not recommended in patients with mild hepatic impairment (total bilirubin > 1 and ≤ 1.5 × ULN and any AST or total bilirubin ≤ ULN and AST > ULN). Reduce the dose of binimetinib for patients with moderate (total bilirubin > 1.5 and ≤ 3 × ULN and any AST) or severe (total bilirubin levels > 3 × ULN and any AST) hepatic impairment.
Females of Reproductive Potential and Males
Pregnancy Testing
- Verify the pregnancy status of females of reproductive potential prior to initiating binimetinib.
Contraception
- Binimetinib can cause fetal harm when administered to a pregnant woman.
Females
- Advise females of reproductive potential to use effective contraception during treatment with binimetinib and for at least 30 days after the final dose.
Immunocompromised Patients
There is no FDA guidance one the use of Binimetinib in patients who are immunocompromised.
Administration and Monitoring
Administration
Patient Selection
- Confirm the presence of a BRAF V600E or V600K mutation in tumor specimens prior to initiating binimetinib. Information on FDA-approved tests for the detection of BRAF V600E and V600K mutations in melanoma is available at: http://www.fda.gov/CompanionDiagnostics.
Recommended Dosage
- The recommended dosage of binimetinib is 45 mg orally taken twice daily, approximately 12 hours apart, in combination with encorafenib until disease progression or unacceptable toxicity. Refer to the encorafenib prescribing information for recommended encorafenib dosing information.
- Binimetinib may be taken with or without food. Do not take a missed dose of binimetinib within 6 hours of the next dose of binimetinib.
- Do not take an additional dose if vomiting occurs after binimetinib administration but continue with the next scheduled dose.
Dosage Modifications for Adverse Reactions
- If encorafenib is permanently discontinued, discontinue binimetinib.
- Dose reductions for adverse reactions associated with binimetinib are presented in Table 1.

- Dosage modifications for adverse reactions associated with binimetinib are presented in Table 2.

- Refer to the encorafenib prescribing information for dose modifications for adverse reactions associated with encorafenib.
Dosage Modifications for Moderate or Severe Hepatic Impairment
- For patients with moderate (total bilirubin greater than 1.5 and less than or equal to 3 × ULN and any AST) or severe (total bilirubin levels greater than 3 × ULN and any AST) hepatic impairment, the recommended dosage is 30 mg orally taken twice daily.
Monitoring
There is limited information regarding Binimetinib Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Binimetinib and IV administrations.
Overdosage
- Since binimetinib is 97% bound to plasma proteins, hemodialysis is likely to be ineffective in the treatment of overdose with binimetinib.
Pharmacology
| |
Binimetinib
| |
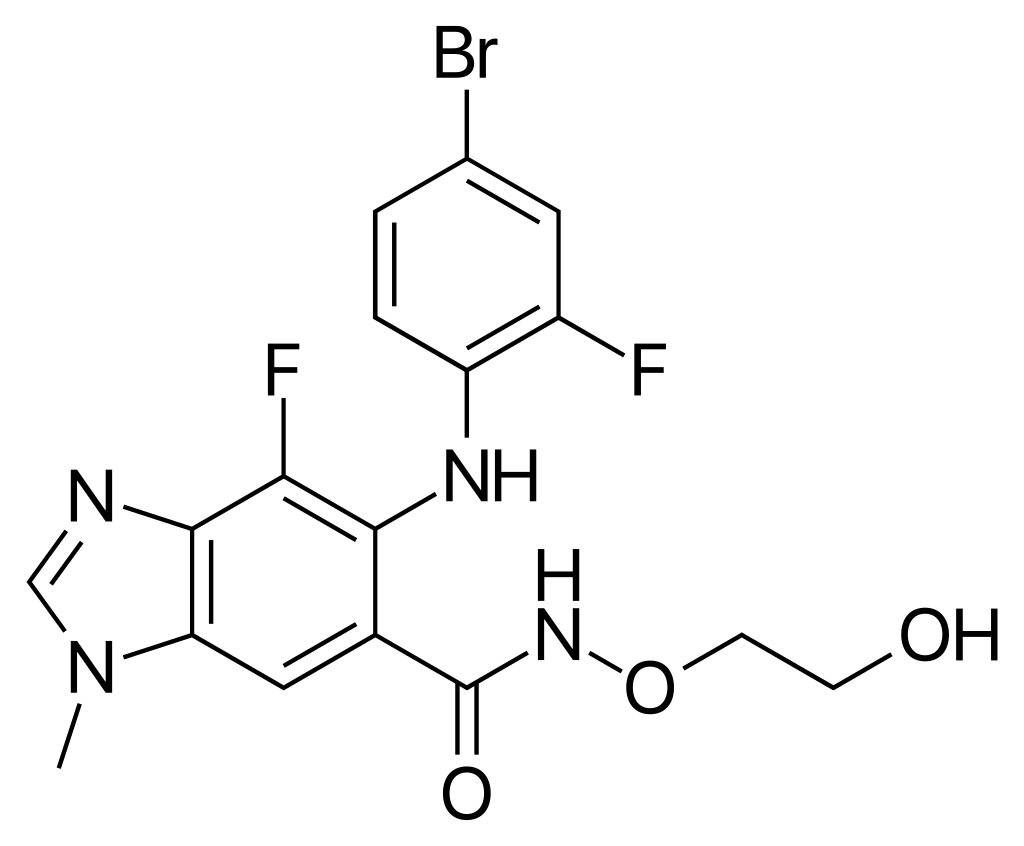
| Systematic (IUPAC) name | |
| 5-((4-bromo-2-fluorophenyl)amino)-4-fluoro-N-(2-hydroxyethoxy)-1-methyl-1H-benzo[d]imidazole-6-carboxamide | |
| Identifiers | |
| CAS number | |
| ATC code | L01 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 441.23 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status |
Investigational |
| Routes | ? |
Mechanism of Action
- Binimetinib is a reversible inhibitor of mitogen-activated extracellular signal regulated kinase 1 (MEK1) and MEK2 activity. MEK proteins are upstream regulators of the extracellular signal-related kinase (ERK) pathway. In vitro, binimetinib inhibited extracellular signal-related kinase (ERK) phosphorylation in cell-free assays as well as viability and MEK-dependent phosphorylation of BRAF-mutant human melanoma cell lines. Binimetinib also inhibited in vivo ERK phosphorylation and tumor growth in BRAF-mutant murine xenograft models.
- Binimetinib and encorafenib target two different kinases in the RAS/RAF/MEK/ERK pathway. Compared to either drug alone, coadministration of encorafenib and binimetinib resulted in greater anti-proliferative activity in vitro in BRAF mutation-positive cell lines and greater anti-tumor activity with respect to tumor growth inhibition in BRAF V600E mutant human melanoma xenograft studies in mice. Additionally, the combination of binimetinib and encorafenib delayed the emergence of resistance in BRAF V600E mutant human melanoma xenografts in mice compared to either drug alone.
Structure
The molecular formula is C17H15BrF2N4O3 and the molecular weight is 441.2 daltons. The chemical structure of binimetinib is shown below:

Pharmacodynamics
Cardiac Electrophysiology
- Following binimetinib 45 mg twice daily, no clinically meaningful QT prolongation was observed.
Pharmacokinetics
- The pharmacokinetics of binimetinib was studied in healthy subjects and patients with solid tumors. After twice-daily dosing, the accumulation is 1.5-fold and the coefficient of variation (CV%) of the area under the concentration-time curve (AUC) is < 40% at steady state. The systemic exposure of binimetinib is approximately dose proportional.
Absorption
- After oral administration, at least 50% of the binimetinib dose was absorbed with a median time to maximum concentration (Tmax) of 1.6 hours.
Effect of Food
- The administration of a single dose of binimetinib 45 mg with a high-fat, high-calorie meal (consisting of approximately 150 calories from protein, 350 calories from carbohydrate, and 500 calories from fat) in healthy subjects had no effect on binimetinib exposure.
Distribution
- Binimetinib is 97% bound to human plasma proteins and the blood-to-plasma ratio is 0.72. The geometric mean (CV%) of apparent volume of distribution of binimetinib is 92 L (45%).
Elimination
- The mean (CV%) terminal half-life (t1/2) of binimetinib is 3.5 hours (28.5%) and apparent clearance (CL/F) is 20.2 L/h (24%).
Metabolism
- The primary metabolic pathway is glucuronidation with UGT1A1 contributing up to 61% of the binimetinib metabolism. Other pathways of binimetinib metabolism include N-dealkylation, amide hydrolysis, and loss of ethane-diol from the side chain. The active metabolite M3 produced by CYP1A2 and CYP2C19 represents 8.6% of the binimetinib exposure. Following a single oral dose of 45 mg radiolabeled binimetinib, approximately 60% of the circulating radioactivity AUC in plasma was attributable to binimetinib.
Excretion
- Following a single oral dose of 45 mg radiolabeled binimetinib in healthy subjects, 62% (32% unchanged) of the administered dose was recovered in the feces while 31% (6.5% unchanged) was recovered in the urine.
Specific Populations
- Age (20 to 94 years), sex, or body weight do not have a clinically important effect on the systemic exposure of binimetinib. The effect of race or ethnicity on the pharmacokinetics of binimetinib is unknown.
- Hepatic Impairment: No clinically meaningful changes in binimetinib exposure (AUC and Cmax) were observed in subjects with mild hepatic impairment (total bilirubin > 1 and ≤ 1.5 × ULN and any AST or total bilirubin ≤ ULN and AST > ULN) as compared to subjects with normal liver function (total bilirubin ≤ ULN and AST ≤ ULN). A 2-fold increase in AUC was observed in subjects with moderate (total bilirubin > 1.5 and ≤ 3 × ULN and any AST) or severe (total bilirubin levels > 3 × ULN and any AST) hepatic impairment.
- Renal Impairment: In subjects with severe renal impairment (eGFR ≤ 29 mL/min/1.73 m2), no clinically important changes in binimetinib exposure were observed as compared to subjects with normal renal function.
Drug Interaction Studies
Clinical Studies
- Effect of UGT1A1 Inducers or Inhibitors on Binimetinib: UGT1A1 genotype and smoking (UGT1A1 inducer) do not have a clinically important effect on binimetinib exposure. Simulations predict similar Cmax of binimetinib 45 mg in the presence or absence of atazanavir 400 mg (UGT1A1 inhibitor).
- No differences in binimetinib exposure have been observed when binimetinib is coadministered with encorafenib.
- Effect of Binimetinib on CYP Substrates: Binimetinib did not alter the exposure of a sensitive CYP3A4 substrate (midazolam).
- Effect of Acid Reducing Agents on Binimetinib: The extent of binimetinib exposure (AUC) was not altered in the presence of a gastric acid reducing agent (rabeprazole).
In Vitro Studies
- Effect of Binimetinib on CYP Substrates: Binimetinib is not a time-dependent inhibitor of CYP1A2, CYP2C9, CYP2D6 or CYP3A.
- Effect of Transporters on Binimetinib: Binimetinib is a substrate of P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP). Binimetinib is not a substrate of organic anion transporting polypeptide (OATP1B1, OATP1B3, OATP2B1) or organic cation transporter 1 (OCT1).
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Carcinogenicity studies with binimetinib have not been conducted. Binimetinib was not genotoxic in studies evaluating reverse mutations in bacteria, chromosomal aberrations in mammalian cells, or micronuclei in bone marrow of rats.
- No dedicated fertility studies have been conducted with binimetinib in animals. In general toxicology studies in rats and monkeys, there were no remarkable findings in male or female reproductive organs.
Clinical Studies
- Binimetinib in combination with encorafenib was evaluated in a randomized, active-controlled, open-label, multicenter trial (COLUMBUS; NCT01909453). Eligible patients were required to have BRAF V600E or V600K mutation-positive unresectable or metastatic melanoma, as detected using the bioMerieux THxID™BRAF assay. Patients were permitted to have received immunotherapy in the adjuvant setting and one prior line of immunotherapy for unresectable locally advanced or metastatic disease. Prior use of BRAF inhibitors or MEK inhibitors was prohibited. Randomization was stratified by American Joint Committee on Cancer (AJCC) Stage (IIIB, IIIC, IVM1a or IVM1b, versus IVM1c), Eastern Cooperative Oncology Group (ECOG) performance status (0 versus 1), and prior immunotherapy for unresectable or metastatic disease (yes versus no).
- Patients were randomized (1:1:1) to receive binimetinib 45 mg twice daily in combination with encorafenib 450 mg once daily (binimetinib in combination with encorafenib), encorafenib 300 mg once daily, or vemurafenib 960 mg twice daily. Treatment continued until disease progression or unacceptable toxicity. Only the results of the approved dosing (binimetinib 45 mg in combination with encorafenib 450 mg) are described below.
- The major efficacy outcome measure was progression-free survival (PFS), as assessed by a blinded independent central review, to compare binimetinib in combination with encorafenib with vemurafenib. Additional efficacy measures included overall survival (OS), as well as objective response rate (ORR) and duration of response (DoR) which were assessed by central review.
- A total of 577 patients were randomized, 192 to the binimetinib in combination with encorafenib arm, 194 to the encorafenib arm, and 191 to the vemurafenib arm. Of the 383 patients randomized to either the binimetinib in combination with encorafenib or the vemurafenib arms, the median age was 56 years (20 to 89 years), 59% were male, 91% were White, and 72% had baseline ECOG performance status of 0. Ninety-five percent (95%) had metastatic disease, 65% were Stage IVM1c, and 4% received prior CTLA-4, PD-1, or PD-L1 directed antibodies. Twenty-eight percent (28%) had elevated baseline serum lactate dehydrogenase (LDH), 45% had ≥ 3 organs with tumor involvement at baseline, and 3% had brain metastases. Based on centralized testing, 100% of patients' tumors tested positive for BRAF mutations; BRAF V600E (88%), BRAF V600K (11%), or both (< 1%).
- Binimetinib in combination with encorafenib demonstrated a statistically significant improvement in PFS compared to vemurafenib. Efficacy results are summarized in Table 5 and Figure 1.


How Supplied
- Binimetinib is supplied as 15 mg yellow/dark yellow, unscored biconvex oval film-coated tablets debossed with a stylized "A" on one side and "15" on the other side, available in bottles of 180 tablets.
Storage
- Store at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C and 30°C (59°F and 86°F).
Images
Drug Images
{{#ask: Page Name::Binimetinib |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel

{{#ask: Label Page::Binimetinib |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Advise the patient to read the FDA-approved patient labeling (Patient Information).
- Inform patients of the following:
Cardiomyopathy
- Advise patients to report any symptoms of heart failure to their healthcare provider.
Venous Thrombosis
- Advise patients to contact their healthcare provider if they experience symptoms of venous thrombosis or pulmonary embolism. Advise patients to seek medical attention for sudden onset of difficulty breathing, leg pain, or swelling.
Ocular Toxicities
- Advise patients to contact their healthcare provider if they experience any changes in their vision.
Interstitial Lung Disease
- Advise patients to contact their healthcare provider if they experience any new or worsening respiratory symptoms including cough or dyspnea.
Hepatotoxicity
- Advise patients that serial testing of serum liver tests (ALT, AST, bilirubin) is recommended during treatment with binimetinib. Instruct patients to report symptoms of liver dysfunction including jaundice, dark urine, nausea, vomiting, loss of appetite, fatigue, bruising, or bleeding.
Rhabdomyolysis
- Advise patients to contact their healthcare provider as soon as possible if they experience unusual or new onset weakness, myalgia, or darkened urine.
Hemorrhage
- Advise patients to notify their healthcare provider if they experience symptoms suggestive of hemorrhage, such as unusual bleeding.
Females and Males of Reproductive Potential
- Embryo-Fetal Toxicity: Advise females with reproductive potential of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with binimetinib and for 30 days after the final dose. Advise females to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, during treatment with binimetinib.
- Lactation: Advise women not to breastfeed during treatment with binimetinib and for 3 days after the final dose.
Patient Package Insert

Precautions with Alcohol
Alcohol-Binimetinib interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
Look-Alike Drug Names
There is limited information regarding Binimetinib Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.