Atovaquone-Proguanil
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Turky Alkathery, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Atovaquone-Proguanil is an antimalarial that is FDA approved for the prophylaxis of Plasmodium falciparum malaria, including in areas where chloroquine resistance has been reported. Treatment of acute, uncomplicated P. falciparum malaria. Common adverse reactions include diarrhea, dreams, oral ulcers, headache, abdominal pain, nausea, vomiting, asthenia, anorexia, and dizziness.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
Prevention of Malaria
- Atovaquone/proguanil is indicated for the prophylaxis of Plasmodium falciparum malaria, including in areas where chloroquine resistance has been reported.
Treatment of Malaria
- Atovaquone/proguanil is indicated for the treatment of acute, uncomplicated P. falciparum malaria. Atovaquone/proguanil has been shown to be effective in regions where the drugs chloroquine, halofantrine, mefloquine, and amodiaquine may have unacceptable failure rates, presumably due to drug resistance.
Dosage
- The daily dose should be taken at the same time each day with food or a milky drink. In the event of vomiting within 1 hour after dosing, a repeat dose should be taken.
- atovaquone/proguanil may be crushed and mixed with condensed milk just prior to administration to patients who may have difficulty swallowing tablets.
Prevention of Malaria
- Start prophylactic treatment with atovaquone/proguanil 1 or 2 days before entering a malaria‑endemic area and continue daily during the stay and for 7 days after return.
- Adults: One atovaquone/proguanil Tablet (adult strength = 250 mg atovaquone/100 mg proguanil hydrochloride) per day.
Treatment of Acute Malaria
- Adults: Four atovaquone/proguanil Tablets (adult strength; total daily dose 1 g atovaquone/400 mg proguanil hydrochloride) as a single daily dose for 3 consecutive days.
- Do not use Atovaquone/proguanil for malaria prophylaxis in patients with severe renal impairment (creatinine clearance <30 mL/min). Use with caution for the treatment of malaria in patients with severe renal impairment, only if the benefits of the 3-day treatment regimen outweigh the potential risks associated with increased drug exposure. No dosage adjustments are needed in patients with mild (creatinine clearance 50 to 80 mL/min) or moderate (creatinine clearance 30 to 50 mL/min) renal impairment.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Atovaquone-Proguanil in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Atovaquone-Proguanil in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Indication
Prevention of Malaria
- Atovaquone/proguanil is indicated for the prophylaxis of Plasmodium falciparum malaria, including in areas where chloroquine resistance has been reported.
Treatment of Malaria
- Atovaquone/proguanil is indicated for the treatment of acute, uncomplicated P. falciparum malaria. atovaquone/proguanil has been shown to be effective in regions where the drugs chloroquine, halofantrine, mefloquine, and amodiaquine may have unacceptable failure rates, presumably due to drug resistance.
Dosage
Prevention of Malaria
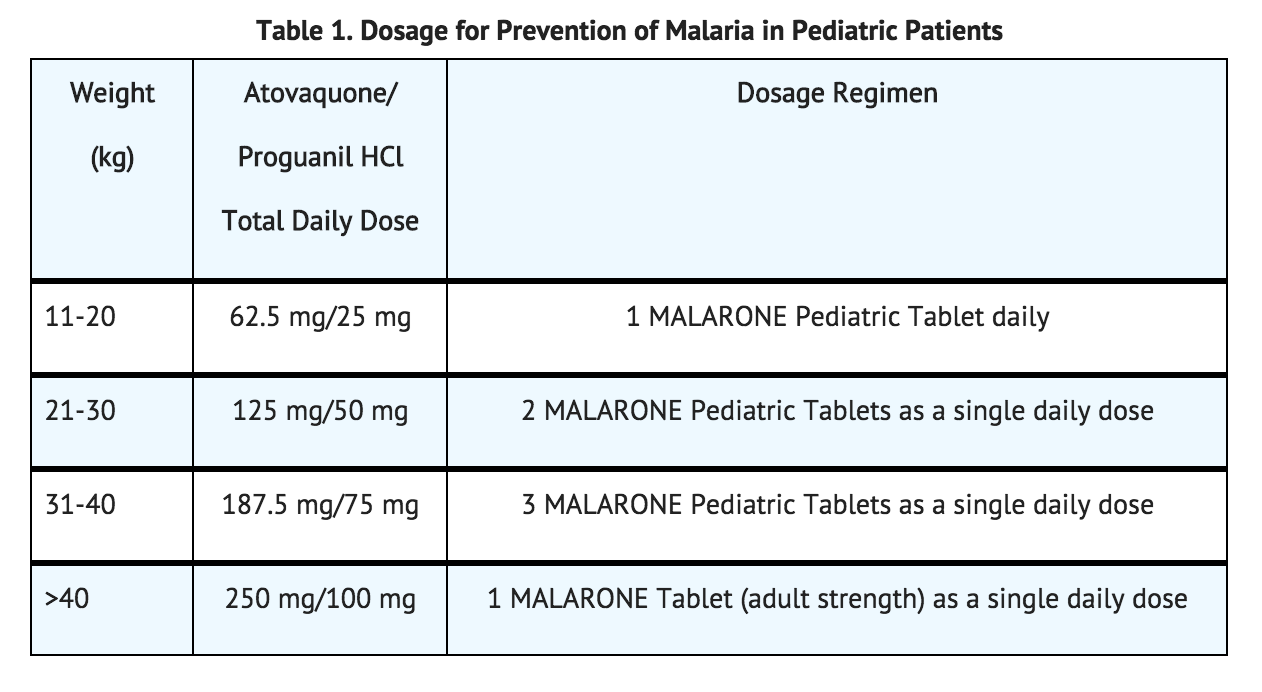
- Pediatric Patients: The dosage for prevention of malaria in pediatric patients is based upon body weight (Table 1).
Treatment of Acute Malaria
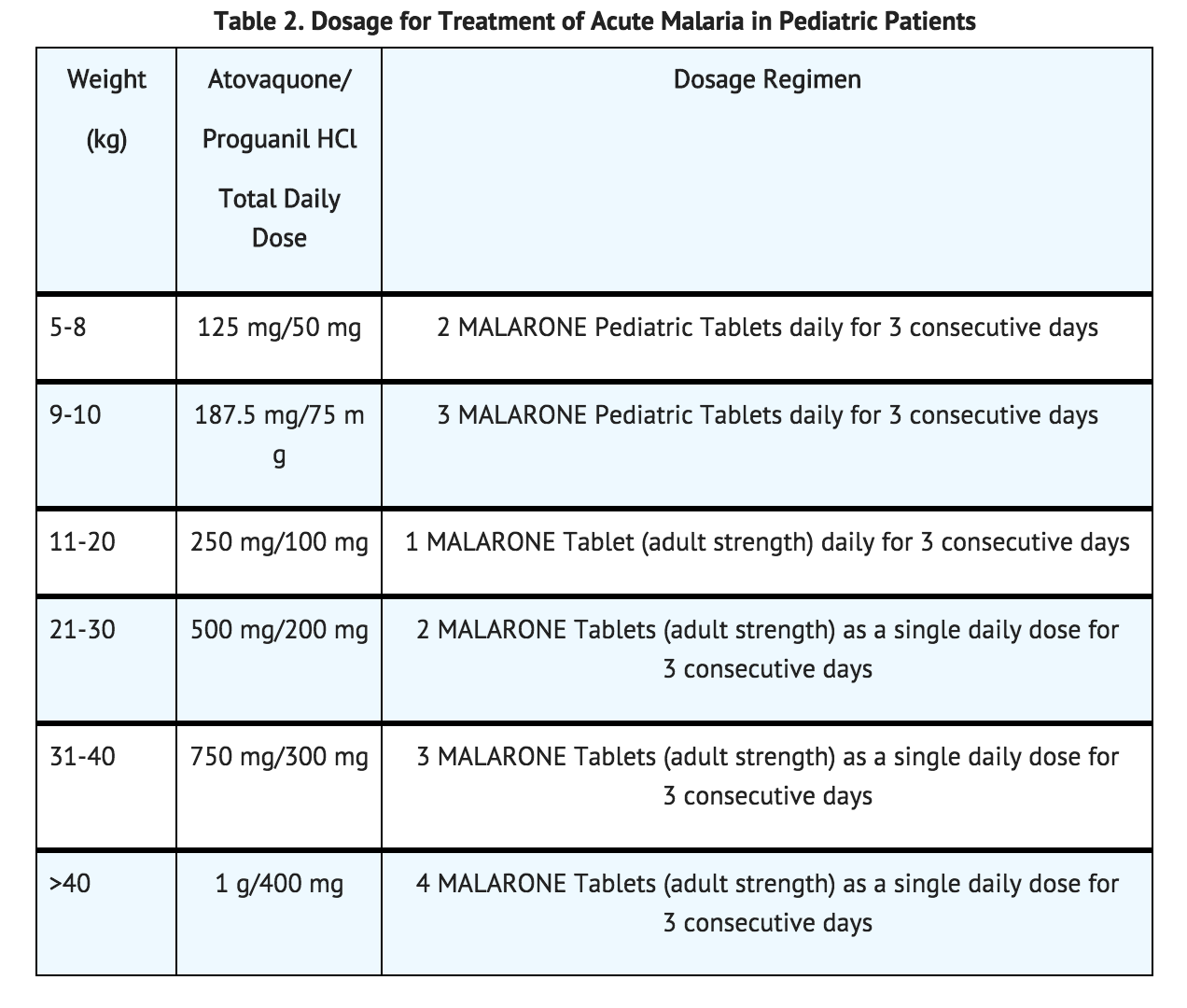
- Pediatric Patients: The dosage for treatment of acute malaria in pediatric patients is based upon body weight (Table 2).
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Atovaquone-Proguanil in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Atovaquone-Proguanil in pediatric patients.
Contraindications
Hypersensitivity
- Atovaquone/proguanil is contraindicated in individuals with known hypersensitivity reactions (e.g., anaphylaxis, erythema multiforme or Stevens-Johnson syndrome, angioedema, vasculitis) to atovaquone or proguanil hydrochloride or any component of the formulation.
Severe Renal Impairment
- Atovaquone/proguanil is contraindicated for prophylaxis of P. falciparum malaria in patients with severe renal impairment (creatinine clearance <30 mL/min) because of pancytopenia in patients with severe renal impairment treated with proguanil.
Warnings
Vomiting and Diarrhea
- Absorption of atovaquone may be reduced in patients with diarrhea or vomiting. If atovaquone/proguanil is used in patients who are vomiting, parasitemia should be closely monitored and the use of an antiemetic considered. Vomiting occurred in up to 19% of pediatric patients given treatment doses of atovaquone/proguanil. In the controlled clinical trials, 15.3% of adults received an antiemetic when they received atovaquonep/roguanil and 98.3% of these patients were successfully treated. In patients with severe or persistent diarrhea or vomiting, alternative antimalarial therapy may be required.
Relapse of Infection
- In mixed P. falciparum and Plasmodium vivax infections, P. vivax parasite relapse occurred commonly when patients were treated with atovaquone/proguanil alone.
- In the event of recrudescent P. falciparum infections after treatment with atovaquone/proguanil or failure of chemoprophylaxis with atovaquone/proguanil, patients should be treated with a different blood schizonticide.
Hepatotoxicity
- Elevated liver laboratory tests and cases of hepatitis and hepatic failure requiring liver transplantation have been reported with prophylactic use of atovaquone/proguanil.
Severe or Complicated Malaria
- Atovaquone/proguanil has not been evaluated for the treatment of cerebral malaria or other severe manifestations of complicated malaria, including hyperparasitemia, pulmonary edema, or renal failure. Patients with severe malaria are not candidates for oral therapy.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- Because atovaquone/proguanil contains atovaquone/proguanil hydrochloride, the type and severity of adverse reactions associated with each of the compounds may be expected. The lower prophylactic doses of atovaquone/proguanil were better tolerated than the higher treatment doses.
- Prophylaxis of P. falciparum malaria: In 3 clinical trials (2 of which were placebo‑controlled) 381 adults (mean age 31 years) received atovaquone/proguanil for the prophylaxis of malaria; the majority of adults were black (90%) and 79% were male. In a clinical trial for the prophylaxis of malaria, 125 pediatric patients (mean age 9 years) received atovaquone/proguanil; all subjects were black and 52% were male. Adverse experiences reported in adults and pediatric patients, considered attributable to therapy, occurred in similar proportions of subjects receiving atovaquone/proguanil or placebo in all studies. Prophylaxis with atovaquone/proguanil was discontinued prematurely due to a treatment‑related adverse experience in 3 of 381 (0.8%) adults and 0 of 125 pediatric patients.
- In a placebo‑controlled study of malaria prophylaxis with atovaquone/proguanil involving 330 pediatric patients (aged 4 to 14 years) in Gabon, a malaria-endemic area, the safety profile of atovaquone/proguanil was consistent with that observed in the earlier prophylactic studies in adults and pediatric patients. The most common treatment‑emergent adverse events with atovaquone/proguanil were abdominal pain (13%), headache (13%), and cough (10%). abdominal pain (13% vs. 8%) and vomiting (5% vs. 3%) were reported more often with atovaquone/proguanil than with placebo. No patient withdrew from the study due to an adverse experience with atovaquone/proguanil. No routine laboratory data were obtained during this study.
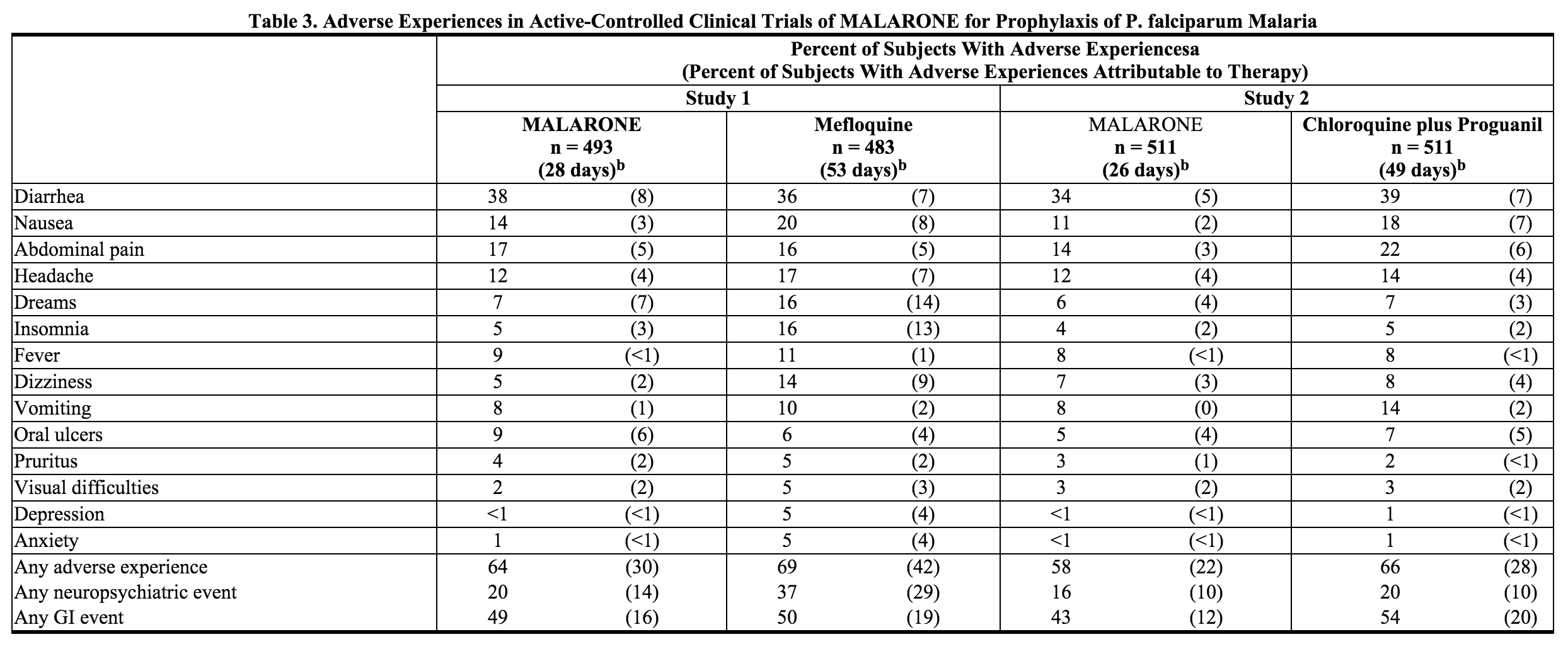
- Non‑immune travelers visiting a malaria‑endemic area received atovaquone/proguanil (n = 1,004) for prophylaxis of malaria in 2 active-controlled clinical trials. In one study (n = 493), the mean age of subjects was 33 years and 53% were male; 90% of subjects were white, 6% of subjects were black and the remaining were of other racial/ethnic groups. In the other study (n = 511), the mean age of subjects was 36 years and 51% were female; the majority of subjects (97%) were white. Adverse experiences occurred in a similar or lower proportion of subjects receiving atovaquone/proguanil than an active comparator (Table 3). Fewer neuropsychiatric adverse experiences occurred in subjects who received atovaquone/proguanil than mefloquine. Fewer gastrointestinal adverse experiences occurred in subjects receiving atovaquone/proguanil than chloroquine/proguanil. Compared with active comparator drugs, subjects receiving atovaquone/proguanil had fewer adverse experiences overall that were attributed to prophylactic therapy (Table 3). Prophylaxis with atovaquone/proguanil was discontinued prematurely due to a treatment‑related adverse experience in 7 of 1,004 travelers.
- In a third active‑controlled study, atovaquone/proguanil (n = 110) was compared with chloroquine/proguanil (n = 111) for the prophylaxis of malaria in 221 non-immune pediatric patients (2 to 17 years of age). The mean duration of exposure was 23 days for atovaquone/proguanil, 46 days for chloroquine, and 43 days for proguanil, reflecting the different recommended dosage regimens for these products. Fewer patients treated with atovaquone/proguanil reported abdominal pain (2% vs. 7%) or nausea (<1% vs. 7%) than children who received chloroquine/proguanil. Oral ulceration (2% vs. 2%), vivid dreams (2% vs. <1%), and blurred vision (0% vs. 2%) occurred in similar proportions of patients receiving either atovaquone/proguanil or chloroquine/proguanil, respectively. Two patients discontinued prophylaxis with chloroquine/proguanil due to adverse events, while none of those receiving atovaquone/proguanil discontinued due to adverse events.
- Treatment of Acute, Uncomplicated P. falciparum malaria: In 7 controlled trials, 436 adolescents and adults received atovaquone/proguanil for treatment of acute, uncomplicated P. falciparum malaria. The range of mean ages of subjects was 26 to 29 years; 79% of subjects were male. In these studies, 48% of subjects were classified as other racial/ethnic groups, primarily Asian; 42% of subjects were black and the remaining subjects were white. Attributable adverse experiences that occurred in ≥5% of patients were abdominal pain (17%), nausea (12%), vomiting (12%), headache (10%), diarrhea (8%), asthenia (8%), anorexia (5%), and dizziness (5%). Treatment was discontinued prematurely due to an adverse experience in 4 of 436 (0.9%) adolescents and adults treated with atovaquone/proguanil.
- In 2 controlled trials, 116 pediatric patients (weighing 11 to 40 kg) (mean age 7 years) received atovaquone/proguanil for the treatment of malaria. The majority of subjects were black (72%); 28% were of other racial/ethnic groups, primarily Asian. Attributable adverse experiences that occurred in ≥5% of patients were vomiting (10%) and pruritus (6%). vomiting occurred in 43 of 319 (13%) pediatric patients who did not have symptomatic malaria but were given treatment doses of atovaquone/proguanil for 3 days in a clinical trial. The design of this clinical trial required that any patient who vomited be withdrawn from the trial. Among pediatric patients with symptomatic malaria treated with atovaquone/proguanil, treatment was discontinued prematurely due to an adverse experience in 1 of 116 (0.9%).
- In a study of 100 pediatric patients (5 to <11 kg body weight) who received atovaquone/proguanil for the treatment of uncomplicated P. falciparum malaria, only diarrhea (6%) occurred in ≥5% of patients as an adverse experience attributable to atovaquone/proguanil. In 3 patients (3%), treatment was discontinued prematurely due to an adverse experience.
- Abnormalities in laboratory tests reported in clinical trials were limited to elevations of transaminases in malaria patients being treated with atovaquone/proguanil. The frequency of these abnormalities varied substantially across trials of treatment and were not observed in the randomized portions of the prophylaxis trials.
- One active-controlled trial evaluated the treatment of malaria in Thai adults (n = 182); the mean age of subjects was 26 years (range 15 to 63 years); 80% of subjects were male. Early elevations of ALT and AST occurred more frequently in patients treated with atovaquone/proguanil (n = 91) compared to patients treated with an active control, mefloquine (n = 91). On Day 7, rates of elevated ALT and AST with atovaquone/proguanil and mefloquine (for patients who had normal baseline levels of these clinical laboratory parameters) were ALT 26.7% vs. 15.6%; AST 16.9% vs. 8.6%, respectively. By Day 14 of this 28‑day study, the frequency of transaminase elevations equalized across the 2 groups.
Postmarketing Experience
- In addition to adverse events reported from clinical trials, the following events have been identified during postmarketing use of atovaquone/proguanil. Because they are reported voluntarily from a population of unknown size, estimates of frequency cannot be made. These events have been chosen for inclusion due to a combination of their seriousness, frequency of reporting, or potential causal connection to atovaquone/proguanil.
- Blood and Lymphatic System Disorders: Neutropenia and anemia. Pancytopenia in patients with severe renal impairment treated with proguanil.
- Immune System Disorders: Allergic reactions including anaphylaxis, angioedema, and urticaria, and vasculitis.
- Nervous System Disorders: Seizures and psychotic events (such as hallucinations); however, a causal relationship has not been established.
- Gastrointestinal Disorders: Stomatitis.
- Hepatobiliary Disorders: Elevated liver laboratory tests, hepatitis, cholestasis; hepatic failure requiring transplant has been reported.
- Skin and Subcutaneous Tissue Disorders: Photosensitivity, rash, erythema multiforme, and Stevens-Johnson syndrome.
Drug Interactions
Rifampin/Rifabutin
- Concomitant administration of rifampin or rifabutin is known to reduce atovaquone concentrations. The concomitant administration of atovaquone/proguanil and rifampin or rifabutin is not recommended.
Anticoagulants
- Proguanil may potentiate the anticoagulant effect of warfarin and other coumarin-based anticoagulants. The mechanism of this potential drug interaction has not been established. Caution is advised when initiating or withdrawing malaria prophylaxis or treatment with atovaquone/proguanil in patients on continuous treatment with coumarin-based anticoagulants. When these products are administered concomitantly, coagulation tests should be closely monitored.
Tetracycline
- Concomitant treatment with tetracycline has been associated with a reduction in plasma concentrations of atovaquone. Parasitemia should be closely monitored in patients receiving tetracycline.
Metoclopramide
- While antiemetics may be indicated for patients receiving atovaquone/proguanil, metoclopramide may reduce the bioavailability of atovaquone and should be used only if other antiemetics are not available.
- Concomitant administration of atovaquone and indinavir did not result in any change in the steady‑state AUC and Cmax of indinavir but resulted in a decrease in the Ctrough of indinavir. Caution should be exercised when prescribing atovaquone with indinavir due to the decrease in trough concentrations of indinavir.
Use in Specific Populations
Pregnancy
- Atovaquone: Atovaquone was not teratogenic and did not cause reproductive toxicity in rats at doses up to 1,000 mg/kg/day corresponding to maternal plasma concentrations up to 7.3 times the estimated human exposure during treatment of malaria based on AUC. In rabbits, atovaquone caused adverse fetal effects and maternal toxicity at a dose of 1,200 mg/kg/day corresponding to plasma concentrations that were approximately 1.3 times the estimated human exposure during treatment of malaria based on AUC. Adverse fetal effects in rabbits, including decreased fetal body lengths and increased early resorptions and post-implantation losses, were observed only in the presence of maternal toxicity.
- In a pre- and post-natal study in rats, atovaquone did not produce adverse effects in offspring at doses up to 1,000 mg/kg/day corresponding to AUC exposures of approximately 7.3 times the estimated human exposure during treatment of malaria.
- Proguanil: A pre- and post-natal study in Sprague-Dawley rats revealed no adverse effects at doses up to 16 mg/kg/day of proguanil hydrochloride (up to 0.04-times the average human exposure based on AUC). Pre- and post-natal studies of proguanil in animals at exposures similar to or greater than those observed in humans have not been conducted.
- Atovaquone/proguanil: The combination of atovaquone/proguanil hydrochloride was not teratogenic in pregnant rats at atovaquone:proguanil hydrochloride (50:20 mg/kg/day) corresponding to plasma concentrations up to 1.7 and 0.1 times, respectively, the estimated human exposure during treatment of malaria based on AUC. In pregnant rabbits, the combination of atovaquone/proguanil hydrochloride was not teratogenic or embryotoxic to rabbit fetuses at atovaquone:proguanil hydrochloride (100:40 mg/kg/day) corresponding to plasma concentrations of approximately 0.3 and 0.5 times, respectively, the estimated human exposure during treatment of malaria based on AUC.
- There are no adequate and well‑controlled studies of atovaquone and/or proguanil hydrochloride in pregnant women. Atovaquone/proguanil should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Falciparum malaria carries a higher risk of morbidity and mortality in pregnant women than in the general population. Maternal death and fetal loss are both known complications of falciparum malaria in pregnancy. In pregnant women who must travel to malaria‑endemic areas, personal protection against mosquito bites should always be employed in addition to antimalarials.
- The proguanil component of atovaquone/proguanil acts by inhibiting the parasitic dihydrofolate reductase. However, there are no clinical data indicating that folate supplementation diminishes drug efficacy. For women of childbearing age receiving folate supplements to prevent neural tube birth defects, such supplements may be continued while taking atovaquone/proguanil.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Atovaquone-Proguanil in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Atovaquone-Proguanil during labor and delivery.
Nursing Mothers
- It is not known whether atovaquone is excreted into human milk. In a rat study, atovaquone concentrations in the milk were 30% of the concurrent atovaquone concentrations in the maternal plasma.
- Proguanil is excreted into human milk in small quantities.
- Caution should be exercised when atovaquone/proguanil is administered to a nursing woman.
Pediatric Use
- Prophylaxis of Malaria: Safety and effectiveness have not been established in pediatric patients who weigh less than 11 kg. The efficacy and safety of atovaquone/proguanil have been established for the prophylaxis of malaria in controlled trials involving pediatric patients weighing 11 kg or more.
- Treatment of Malaria: Safety and effectiveness have not been established in pediatric patients who weigh less than 5 kg. The efficacy and safety of atovaquone/proguanil for the treatment of malaria have been established in controlled trials involving pediatric patients weighing 5 kg or more.
Geriatic Use
- Clinical trials of atovaquone/proguanil did not include sufficient numbers of subjects aged 65 years and older to determine whether they respond differently from younger subjects. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, the higher systemic exposure to cycloguanil, and the greater frequency of concomitant disease or other drug therapy.
Gender
There is no FDA guidance on the use of Atovaquone-Proguanil with respect to specific gender populations.
Race
There is no FDA guidance on the use of Atovaquone-Proguanil with respect to specific racial populations.
Renal Impairment
- Do not use atovaquone/proguanil for malaria prophylaxis in patients with severe renal impairment (creatinine clearance <30 mL/min). Use with caution for the treatment of malaria in patients with severe renal impairment, only if the benefits of the 3-day treatment regimen outweigh the potential risks associated with increased drug exposure. No dosage adjustments are needed in patients with mild (creatinine clearance 50 to 80 mL/min) or moderate (creatinine clearance 30 to 50 mL/min) renal impairment.
Hepatic Impairment
- No dosage adjustments are needed in patients with mild or moderate hepatic impairment. No trials have been conducted in patients with severe hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Atovaquone-Proguanil in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Atovaquone-Proguanil in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral.
Monitoring
- If used in patients who are vomiting, parasitemia should be closely monitored and the use of an antiemetic considered.
- Proguanil may potentiate anticoagulant effect of warfarin and other coumarin-based anticoagulants. Caution advised when initiating or withdrawing atovaquone/proguanil in patients on anticoagulants; coagulation tests should be closely monitored.
- Tetracycline may reduce atovaquone concentrations; parasitemia should be closely monitored.
IV Compatibility
There is limited information regarding the compatibility of Atovaquone-Proguanil and IV administrations.
Overdosage
- There is no information on overdoses of MALARONE substantially higher than the doses recommended for treatment.
- There is no known antidote for atovaquone, and it is currently unknown if atovaquone is dialyzable. Overdoses up to 31,500 mg of atovaquone have been reported. In one such patient who also took an unspecified dose of dapsone, methemoglobinemia occurred. Rash has also been reported after overdose.
- Overdoses of proguanil hydrochloride as large as 1,500 mg have been followed by complete recovery, and doses as high as 700 mg twice daily have been taken for over 2 weeks without serious toxicity. Adverse experiences occasionally associated with proguanil hydrochloride doses of 100 to 200 mg/day, such as epigastric discomfort and vomiting, would be likely to occur with overdose. There are also reports of reversible hair loss and scaling of the skin on the palms and/or soles, reversible aphthous ulceration, and hematologic side effects.
Pharmacology
Atovaquone-Proguanil
| |
| Combination of | |
| Atovaquone | Antimalarial medication |
| Proguanil | Antimalarial medication |
| Identifiers | |
| CAS number | ? |
| ATC code | P01 |
| PubChem | |
| Therapeutic considerations | |
| Licence data |
|
| Pregnancy cat. | |
| Legal status |
POM(UK) Template:Unicode Prescription only |
| Routes | Oral |
Mechanism of Action
- The constituents of MALARONE, atovaquone/proguanil hydrochloride, interfere with 2 different pathways involved in the biosynthesis of pyrimidines required for nucleic acid replication. Atovaquone is a selective inhibitor of parasite mitochondrial electron transport. Proguanil hydrochloride primarily exerts its effect by means of the metabolite cycloguanil, a dihydrofolate reductase inhibitor. Inhibition of dihydrofolate reductase in the malaria parasite disrupts deoxythymidylate synthesis.
Structure
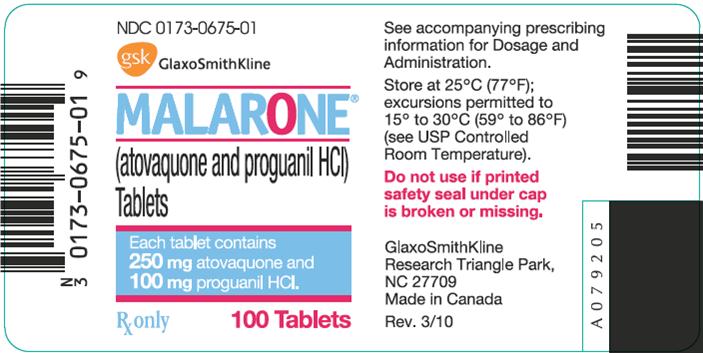
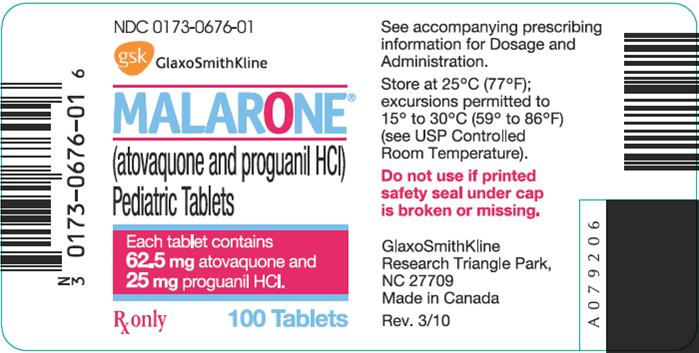
- MALARONE (atovaquone/proguanil hydrochloride) Tablets (adult strength) and MALARONE (atovaquone/proguanil hydrochloride) Pediatric Tablets, for oral administration, contain a fixed‑dose combination of the antimalarial agents atovaquone/proguanil hydrochloride.
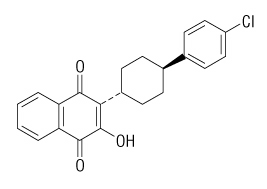
- The chemical name of atovaquone is trans-2-[4-(4-chlorophenyl)cyclohexyl]-3-hydroxy-1,4-naphthalenedione. Atovaquone is a yellow crystalline solid that is practically insoluble in water. It has a molecular weight of 366.84 and the molecular formula C22H19ClO3. The compound has the following structural formula:
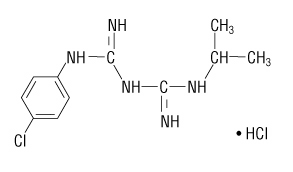
- The chemical name of proguanil hydrochloride is 1-(4-chlorophenyl)-5-isopropyl-biguanide hydrochloride. Proguanil hydrochloride is a white crystalline solid that is sparingly soluble in water. It has a molecular weight of 290.22 and the molecular formula C11H16ClN5•HCl. The compound has the following structural formula:
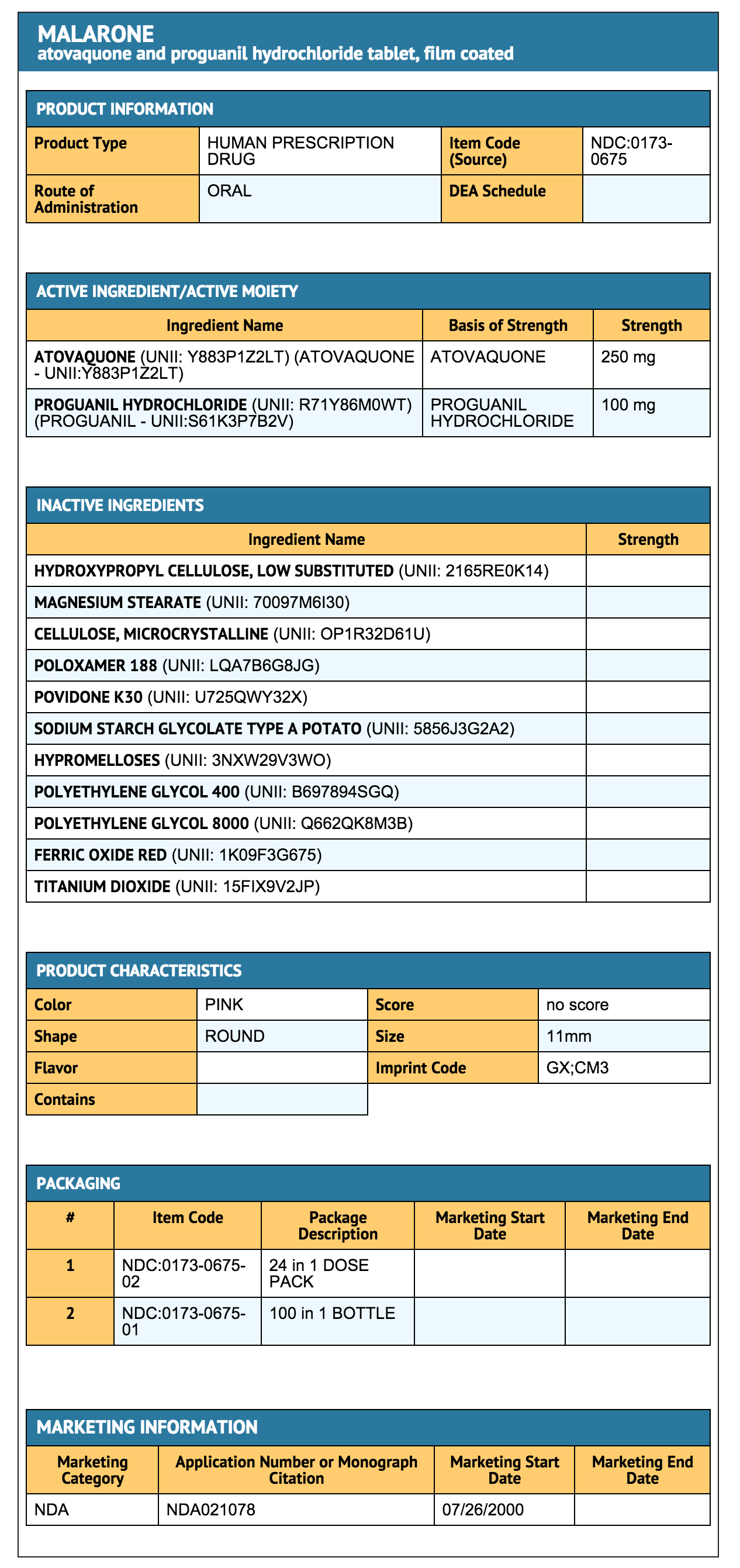
- Each MALARONE Tablet (adult strength) contains 250 mg of atovaquone and 100 mg of proguanil hydrochloride and each MALARONE Pediatric Tablet contains 62.5 mg of atovaquone and 25 mg of proguanil hydrochloride. The inactive ingredients in both tablets are low‑substituted hydroxypropyl cellulose, magnesium stearate, microcrystalline cellulose, poloxamer 188, povidone K30, and sodium starch glycolate. The tablet coating contains hypromellose, polyethylene glycol 400, polyethylene glycol 8000, red iron oxide, and titanium dioxide.
Pharmacodynamics
- No trials of the pharmacodynamics of MALARONE have been conducted.
Pharmacokinetics
- Absorption: Atovaquone is a highly lipophilic compound with low aqueous solubility. The bioavailability of atovaquone shows considerable inter‑individual variability.
- Dietary fat taken with atovaquone increases the rate and extent of absorption, increasing AUC 2 to 3 times and Cmax 5 times over fasting. The absolute bioavailability of the tablet formulation of atovaquone when taken with food is 23%. MALARONE Tablets should be taken with food or a milky drink.
- Distribution: Atovaquone is highly protein bound (>99%) over the concentration range of 1 to 90 mcg/mL. A population pharmacokinetic analysis demonstrated that the apparent volume of distribution of atovaquone (V/F) in adult and pediatric patients after oral administration is approximately 8.8 L/kg.
- Proguanil is 75% protein bound. A population pharmacokinetic analysis demonstrated that the apparent V/F of proguanil in adult and pediatric patients >15 years of age with body weights from 31 to 110 kg ranged from 1,617 to 2,502 L. In pediatric patients ≤15 years of age with body weights from 11 to 56 kg, the V/F of proguanil ranged from 462 to 966 L.
- In human plasma, the binding of atovaquone/proguanil was unaffected by the presence of the other.
- Metabolism: In a study where 14C‑labeled atovaquone was administered to healthy volunteers, greater than 94% of the dose was recovered as unchanged atovaquone in the feces over 21 days. There was little or no excretion of atovaquone in the urine (less than 0.6%). There is indirect evidence that atovaquone may undergo limited metabolism; however, a specific metabolite has not been identified. Between 40% to 60% of proguanil is excreted by the kidneys. Proguanil is metabolized to cycloguanil (primarily via CYP2C19) and 4-chlorophenylbiguanide. The main routes of elimination are hepatic biotransformation and renal excretion.
- Elimination: The elimination half‑life of atovaquone is about 2 to 3 days in adult patients.
- The elimination half‑life of proguanil is 12 to 21 hours in both adult patients and pediatric patients, but may be longer in individuals who are slow metabolizers.
- A population pharmacokinetic analysis in adult and pediatric patients showed that the apparent clearance (CL/F) of both atovaquone/proguanil are related to the body weight. The values CL/F for both atovaquone/proguanil in subjects with body weight ≥11 kg are shown in Table 4.
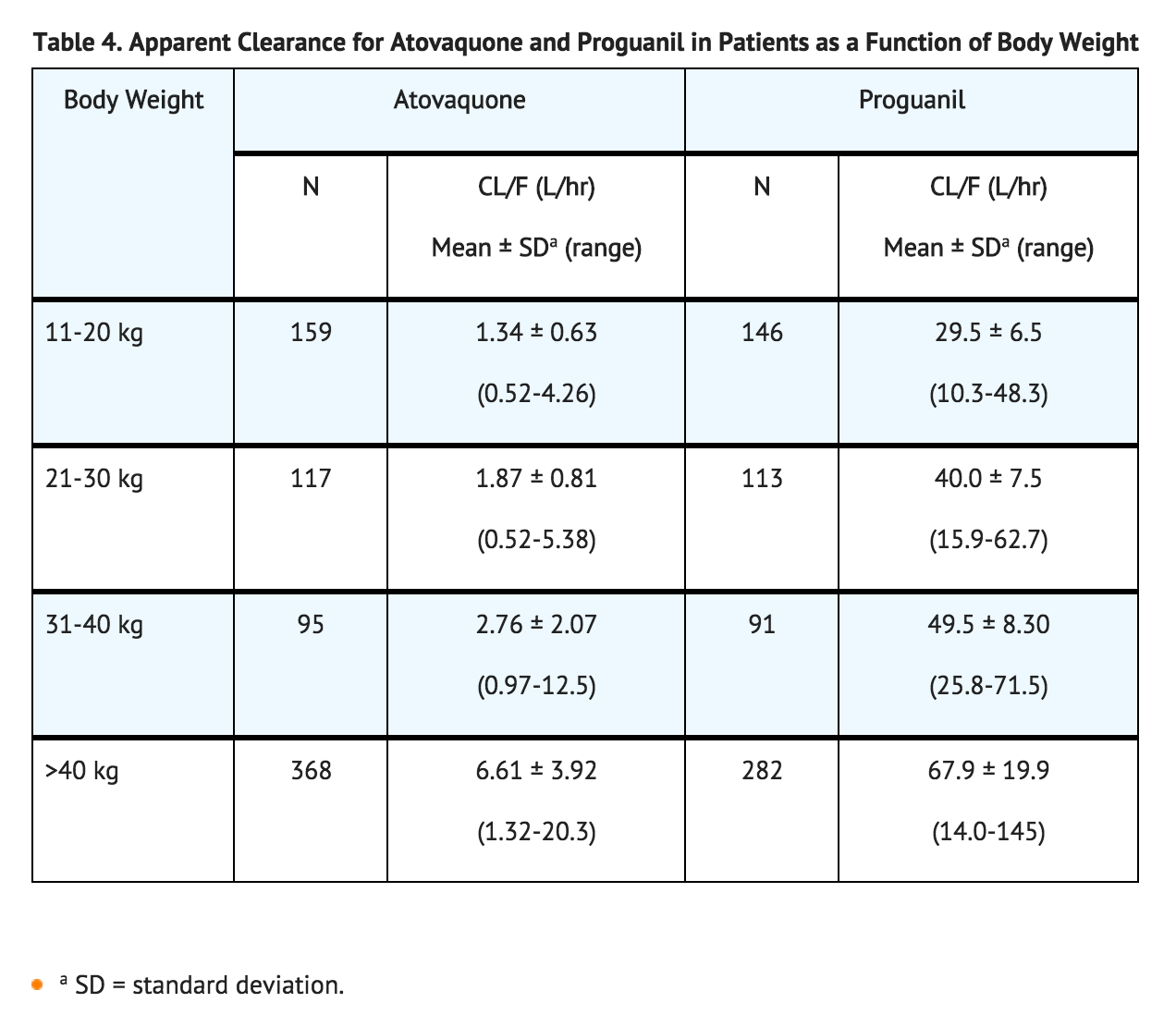
- The pharmacokinetics of atovaquone/proguanil in patients with body weight below 11 kg have not been adequately characterized.
- Pediatrics: The pharmacokinetics of proguanil and cycloguanil are similar in adult patients and pediatric patients. However, the elimination half‑life of atovaquone is shorter in pediatric patients (1 to 2 days) than in adult patients (2 to 3 days). In clinical trials, plasma trough concentrations of atovaquone/proguanil in pediatric patients weighing 5 to 40 kg were within the range observed in adults after dosing by body weight.
- Geriatrics: In a single‑dose study, the pharmacokinetics of atovaquone, proguanil, and cycloguanil were compared in 13 elderly subjects (age 65 to 79 years) to 13 younger subjects (age 30 to 45 years). In the elderly subjects, the extent of systemic exposure (AUC) of cycloguanil was increased (point estimate = 2.36, 90% CI = 1.70, 3.28). Tmax was longer in elderly subjects (median 8 hours) compared with younger subjects (median 4 hours) and average elimination half‑life was longer in elderly subjects (mean 14.9 hours) compared with younger subjects (mean 8.3 hours).
- Renal Impairment: In patients with mild renal impairment (creatinine clearance 50 to 80 mL/min), oral clearance and/or AUC data for atovaquone, proguanil, and cycloguanil are within the range of values observed in patients with normal renal function (creatinine clearance >80 mL/min). In patients with moderate renal impairment (creatinine clearance 30 to 50 mL/min), mean oral clearance for proguanil was reduced by approximately 35% compared with patients with normal renal function (creatinine clearance >80 mL/min) and the oral clearance of atovaquone was comparable between patients with normal renal function and mild renal impairment. No data exist on the use of MALARONE for long-term prophylaxis (over 2 months) in individuals with moderate renal failure. In patients with severe renal impairment (creatinine clearance <30 mL/min), atovaquone Cmax and AUC are reduced but the elimination half‑lives for proguanil and cycloguanil are prolonged, with corresponding increases in AUC, resulting in the potential of drug accumulation and toxicity with repeated dosing.
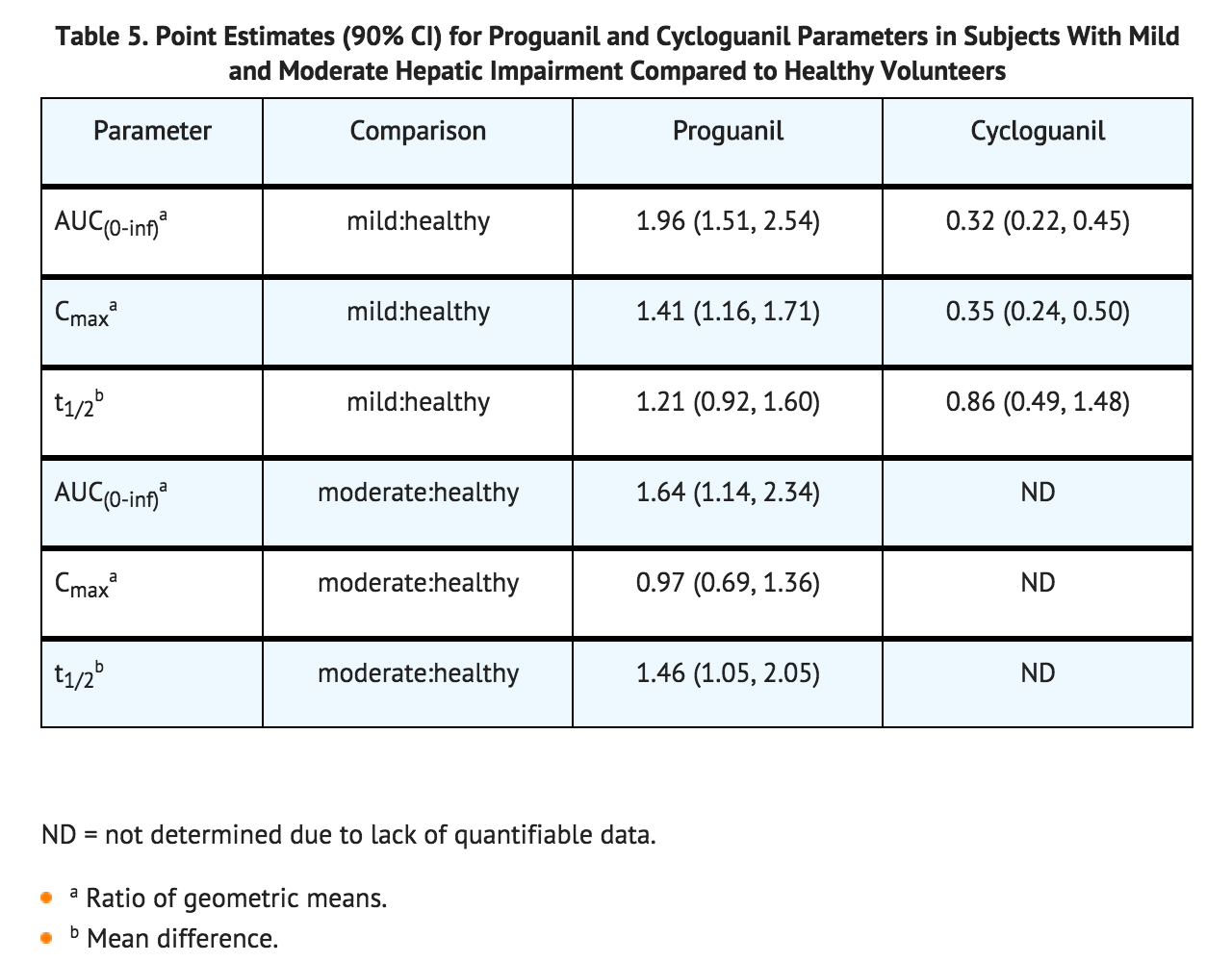
- Hepatic Impairment: In a single‑dose study, the pharmacokinetics of atovaquone, proguanil, and cycloguanil were compared in 13 subjects with hepatic impairment (9 mild, 4 moderate, as indicated by the Child‑Pugh method) to 13 subjects with normal hepatic function. In subjects with mild or moderate hepatic impairment as compared to healthy subjects, there were no marked differences (<50%) in the rate or extent of systemic exposure of atovaquone. However, in subjects with moderate hepatic impairment, the elimination half‑life of atovaquone was increased (point estimate = 1.28, 90% CI = 1.00 to 1.63). Proguanil AUC, Cmax, and its elimination half-life increased in subjects with mild hepatic impairment when compared to healthy subjects (Table 5). Also, the proguanil AUC and its elimination half-life increased in subjects with moderate hepatic impairment when compared to healthy subjects. Consistent with the increase in proguanil AUC, there were marked decreases in the systemic exposure of cycloguanil (Cmax and AUC) and an increase in its elimination half‑life in subjects with mild hepatic impairment when compared to healthy volunteers (Table 5). There were few measurable cycloguanil concentrations in subjects with moderate hepatic impairment. The pharmacokinetics of atovaquone, proguanil, and cycloguanil after administration of MALARONE have not been studied in patients with severe hepatic impairment.
- Drug Interactions: There are no pharmacokinetic interactions between atovaquone/proguanil at the recommended dose.
- Atovaquone is highly protein bound (>99%) but does not displace other highly protein‑bound drugs in vitro.
- Proguanil is metabolized primarily by CYP2C19. Potential pharmacokinetic interactions between proguanil or cycloguanil and other drugs that are CYP2C19 substrates or inhibitors are unknown.
- Rifampin/Rifabutin: Concomitant administration of rifampin or rifabutin is known to reduce atovaquone concentrations by approximately 50% and 34%, respectively. The mechanisms of these interactions are unknown.
- Tetracycline: Concomitant treatment with tetracycline has been associated with approximately a 40% reduction in plasma concentrations of atovaquone.
- Metoclopramide: Concomitant treatment with metoclopramide has been associated with decreased bioavailability of atovaquone.
- Indinavir: Concomitant administration of atovaquone (750 mg twice daily with food for 14 days) and indinavir (800 mg three times daily without food for 14 days) did not result in any change in the steady‑state AUC and Cmax of indinavir but resulted in a decrease in the Ctrough of indinavir (23% decrease [90% CI = 8%, 35%]).
Microbiology
- Activity In Vitro and In Vivo: Atovaquone and cycloguanil (an active metabolite of proguanil) are active against the erythrocytic and exoerythrocytic stages of Plasmodium spp. Enhanced efficacy of the combination compared to either atovaquone or proguanil hydrochloride alone was demonstrated in clinical trials in both immune and non-immune patients.
- Drug Resistance: Strains of P. falciparum with decreased susceptibility to atovaquone or proguanil/cycloguanil alone can be selected in vitro or in vivo. The combination of atovaquone/proguanil hydrochloride may not be effective for treatment of recrudescent malaria that develops after prior therapy with the combination.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Genotoxicity studies have not been performed with atovaquone in combination with proguanil. Effects of MALARONE on male and female reproductive performance are unknown.
- Atovaquone: A 24‑month carcinogenicity study in CD rats was negative for neoplasms at doses up to 500 mg/kg/day corresponding to approximately 54 times the average steady-state plasma concentrations in humans during prophylaxis of malaria. In CD-1 mice, a 24‑month study showed treatment‑related increases in incidence of hepatocellular adenoma and hepatocellular carcinoma at all doses tested (50, 100, and 200 mg/kg/day) which correlated with at least 15 times the average steady‑state plasma concentrations in humans during prophylaxis of malaria.
- Atovaquone was negative with or without metabolic activation in the Ames Salmonella mutagenicity assay, the Mouse Lymphoma mutagenesis assay, and the Cultured Human Lymphocyte cytogenetic assay. No evidence of genotoxicity was observed in the in vivo Mouse Micronucleus assay.
- Atovaquone did not impair fertility in male and female rats at doses up to 1,000 mg/kg/day corresponding to plasma exposures of approximately 7.3 times the estimated human exposure during treatment of malaria based on AUC.
- Proguanil: No evidence of a carcinogenic effect was observed in 24‑month studies conducted in CD-1 mice at doses up to 16 mg/kg/day corresponding to 1.5 times the average human plasma exposure during prophylaxis of malaria based on AUC, and in Wistar Hannover rats at doses up 20 mg/kg/day corresponding to 1.1 times the average human plasma exposure during prophylaxis of malaria based on AUC.
- Proguanil was negative with or without metabolic activation in the Ames Salmonella mutagenicity assay and the Mouse Lymphoma mutagenesis assay. No evidence of genotoxicity was observed in the in vivo Mouse Micronucleus assay.
- Cycloguanil, the active metabolite of proguanil, was also negative in the Ames test, but was positive in the Mouse Lymphoma assay and the Mouse Micronucleus assay. These positive effects with cycloguanil, a dihydrofolate reductase inhibitor, were significantly reduced or abolished with folinic acid supplementation.
- A fertility study in Sprague-Dawley rats revealed no adverse effects at doses up to 16 mg/kg/day of proguanil hydrochloride (up to 0.04-times the average human exposure during treatment of malaria based on AUC). Fertility studies of proguanil in animals at exposures similar to or greater than those observed in humans have not been conducted.
Animal Toxicology and/or Pharmacology
- Fibrovascular proliferation in the right atrium, pyelonephritis, bone marrow hypocellularity, lymphoid atrophy, and gastritis/enteritis were observed in dogs treated with proguanil hydrochloride for 6 months at a dose of 12 mg/kg/day (approximately 3.9 times the recommended daily human dose for malaria prophylaxis on a mg/m2 basis). Bile duct hyperplasia, gall bladder mucosal atrophy, and interstitial pneumonia were observed in dogs treated with proguanil hydrochloride for 6 months at a dose of 4 mg/kg/day (approximately 1.3 times the recommended daily human dose for malaria prophylaxis on a mg/m2 basis). Mucosal hyperplasia of the cecum and renal tubular basophilia were observed in rats treated with proguanil hydrochloride for 6 months at a dose of 20 mg/kg/day (approximately 1.6 times the recommended daily human dose for malaria prophylaxis on a mg/m2 basis). Adverse heart, lung, liver, and gall bladder effects observed in dogs and kidney effects observed in rats were not shown to be reversible.
Clinical Studies
Prevention of P. falciparum Malaria
- MALARONE was evaluated for prophylaxis of P. falciparum malaria in 5 clinical trials in malaria‑endemic areas and in 3 active‑controlled trials in non‑immune travelers to malaria‑endemic areas.
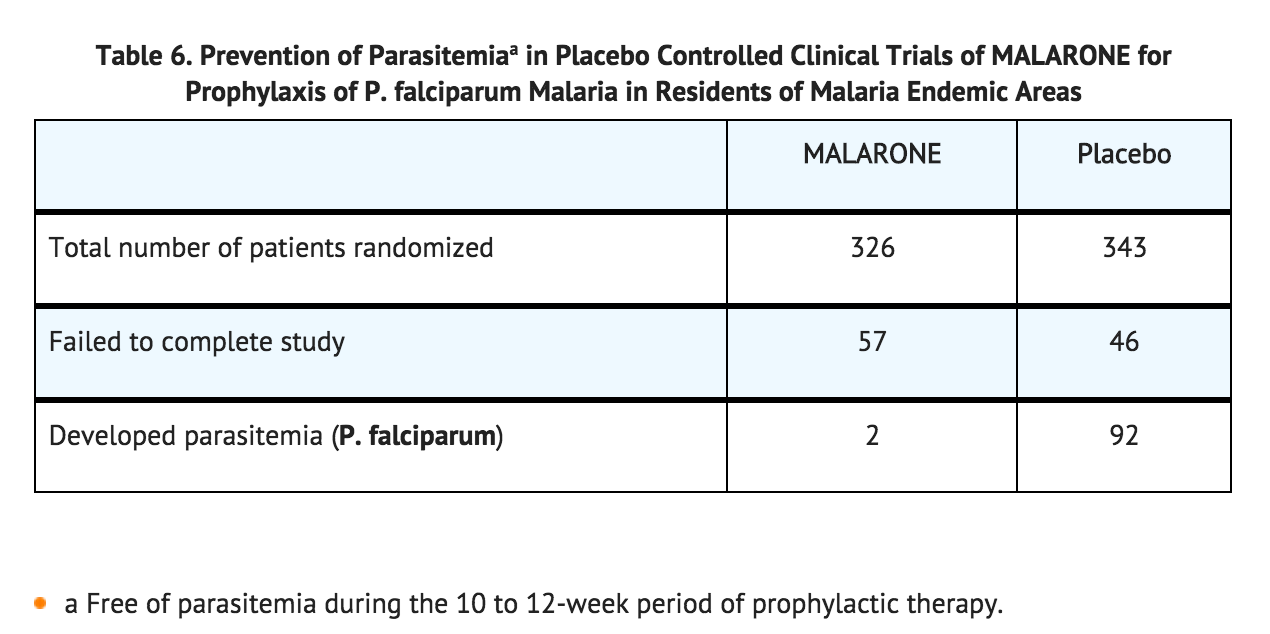
- Three placebo‑controlled trials of 10 to 12 weeks’ duration were conducted among residents of malaria‑endemic areas in Kenya, Zambia, and Gabon. The mean age of subjects was 30 (range 17‑55), 32 (range 16‑64), and 10 (range 5‑16) years, respectively. Of a total of 669 randomized patients (including 264 pediatric patients 5 to 16 years of age), 103 were withdrawn for reasons other than falciparum malaria or drug‑related adverse events (55% of these were lost to follow‑up and 45% were withdrawn for protocol violations). The results are listed in Table 6.
- In another study, 330 Gabonese pediatric patients (weighing 13 to 40 kg, and aged 4 to 14 years) who had received successful open‑label radical cure treatment with artesunate, were randomized to receive either MALARONE (dosage based on body weight) or placebo in a double‑blind fashion for 12 weeks. Blood smears were obtained weekly and any time malaria was suspected. Nineteen of the 165 children given MALARONE and 18 of 165 patients given placebo withdrew from the study for reasons other than parasitemia (primary reason was lost to follow-up). One out of 150 evaluable patients (<1%) who received MALARONE developed P. falciparum parasitemia while receiving prophylaxis with MALARONE compared with 31 (22%) of the 144 evaluable placebo recipients.
- In a 10‑week study in 175 South African subjects who moved into malaria‑endemic areas and were given prophylaxis with 1 MALARONE Tablet daily, parasitemia developed in 1 subject who missed several doses of medication. Since no placebo control was included, the incidence of malaria in this study was not known.
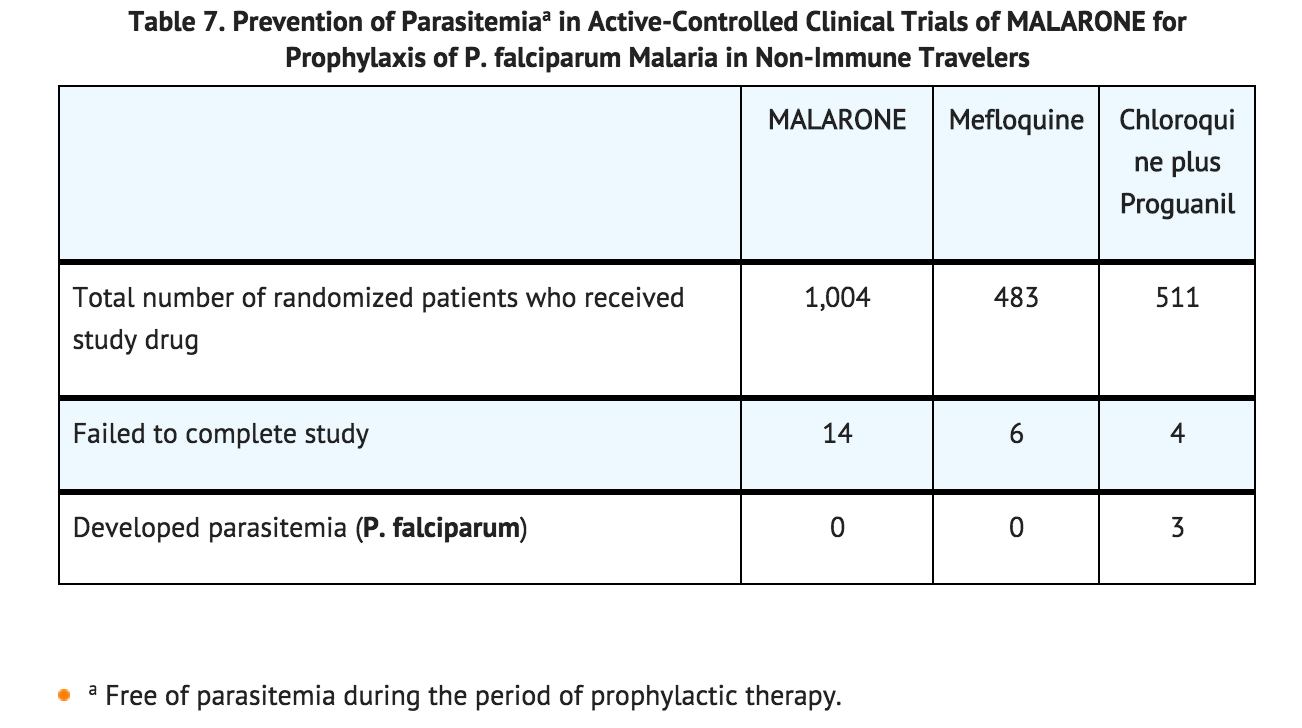
- Two active-controlled trials were conducted in non‑immune travelers who visited a malaria‑endemic area. The mean duration of travel was 18 days (range 2 to 38 days). Of a total of 1,998 randomized patients who received MALARONE or controlled drug, 24 discontinued from the study before follow-up evaluation 60 days after leaving the endemic area. Nine of these were lost to follow-up, 2 withdrew because of an adverse experience, and 13 were discontinued for other reasons. These trials were not large enough to allow for statements of comparative efficacy. In addition, the true exposure rate to P. falciparum malaria in both trials is unknown. The results are listed in Table 7.
- A third randomized, open‑label study was conducted which included 221 otherwise healthy pediatric patients (weighing ≥11 kg and 2 to 17 years of age) who were at risk of contracting malaria by traveling to an endemic area. The mean duration of travel was 15 days (range 1 to 30 days). Prophylaxis with MALARONE (n = 110, dosage based on body weight) began 1 or 2 days before entering the endemic area and lasted until 7 days after leaving the area. A control group (n = 111) received prophylaxis with chloroquine/proguanil dosed according to WHO guidelines. No cases of malaria occurred in either group of children. However, the study was not large enough to allow for statements of comparative efficacy. In addition, the true exposure rate to P. falciparum malaria in this study is unknown.
- Causal Prophylaxis: In separate trials with small numbers of volunteers, atovaquone/proguanil hydrochloride were independently shown to have causal prophylactic activity directed against liver‑stage parasites of P. falciparum. Six patients given a single dose of atovaquone 250 mg 24 hours prior to malaria challenge were protected from developing malaria, whereas all 4 placebo‑treated patients developed malaria.
- During the 4 weeks following cessation of prophylaxis in clinical trial participants who remained in malaria‑endemic areas and were available for evaluation, malaria developed in 24 of 211 (11.4%) subjects who took placebo and 9 of 328 (2.7%) who took MALARONE. While new infections could not be distinguished from recrudescent infections, all but 1 of the infections in patients treated with MALARONE occurred more than 15 days after stopping therapy. The single case occurring on day 8 following cessation of therapy with MALARONE probably represents a failure of prophylaxis with MALARONE.
- The possibility that delayed cases of P. falciparum malaria may occur some time after stopping prophylaxis with MALARONE cannot be ruled out. Hence, returning travelers developing febrile illnesses should be investigated for malaria.
Treatment of Acute, Uncomplicated P. falciparum Malaria Infections
- In 3 phase II clinical trials, atovaquone alone, proguanil hydrochloride alone, and the combination of atovaquone/proguanil hydrochloride were evaluated for the treatment of acute, uncomplicated malaria caused by P. falciparum. Among 156 evaluable patients, the parasitological cure rate (elimination of parasitemia with no recurrent parasitemia during follow‑up for 28 days) was 59/89 (66%) with atovaquone alone, 1/17 (6%) with proguanil hydrochloride alone, and 50/50 (100%) with the combination of atovaquone/proguanil hydrochloride.
- Atovaquone/proguanil was evaluated for treatment of acute, uncomplicated malaria caused by P. falciparum in 8 phase III randomized, open-label, controlled clinical trials (N = 1,030 enrolled in both treatment groups). The mean age of subjects was 27 years and 16% were children ≤12 years of age; 74% of subjects were male. Evaluable patients included those whose outcome at 28 days was known. Among 471 evaluable patients treated with the equivalent of 4 atovaquone/proguanil Tablets once daily for 3 days, 464 had a sensitive response (elimination of parasitemia with no recurrent parasitemia during follow‑up for 28 days) (Table 8). Seven patients had a response of RI resistance (elimination of parasitemia but with recurrent parasitemia between 7 and 28 days after starting treatment). In these trials, the response to treatment with atovaquone/proguanil was similar to treatment with the comparator drug in 4 trials.
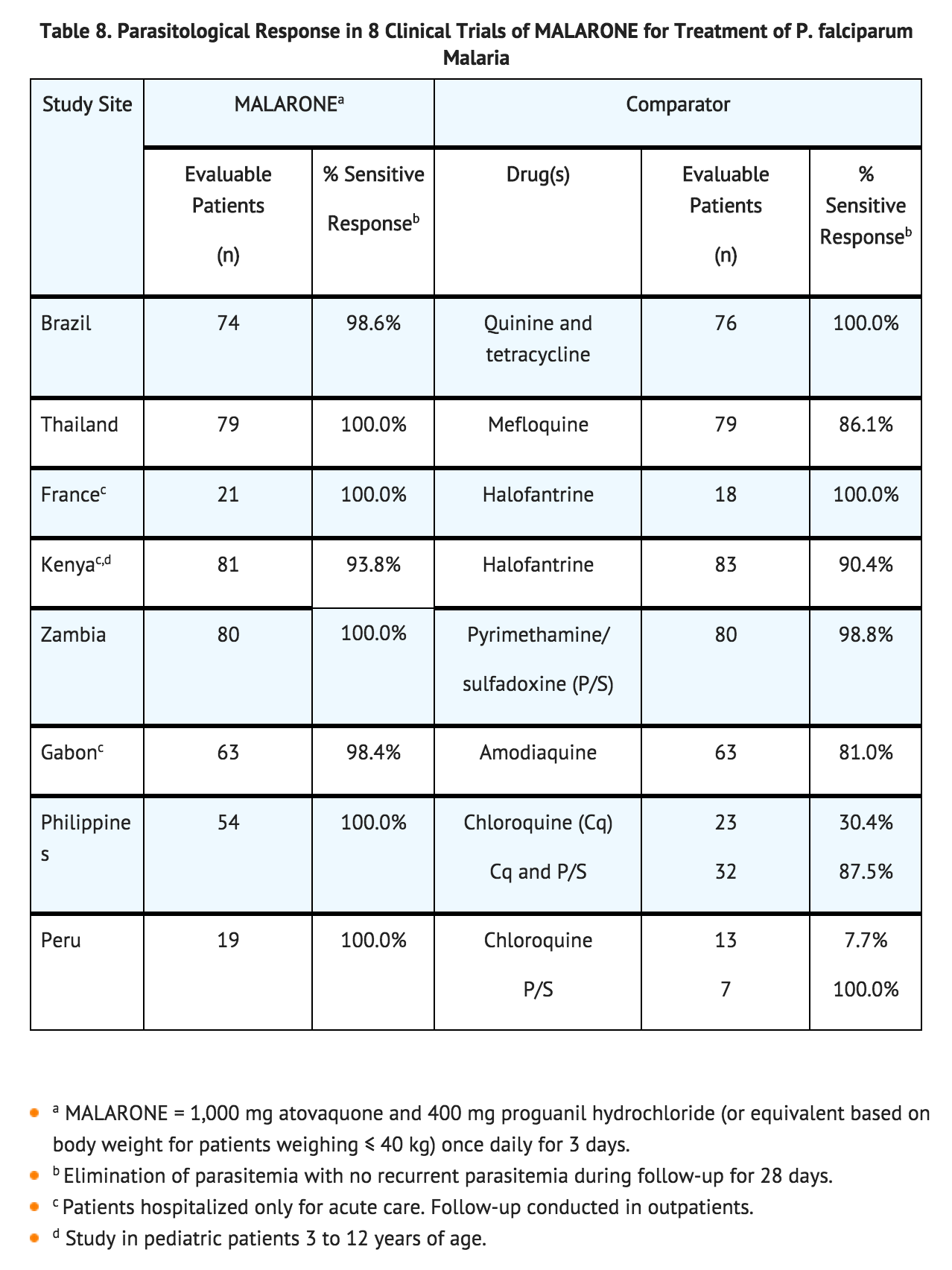
- When these 8 trials were pooled and 2 additional trials evaluating atovaquone/proguanil alone (without a comparator arm) were added to the analysis, the overall efficacy (elimination of parasitemia with no recurrent parasitemia during follow‑up for 28 days) in 521 evaluable patients was 98.7%.
- The efficacy of atovaquone/proguanil in the treatment of the erythrocytic phase of nonfalciparum malaria was assessed in a small number of patients. Of the 23 patients in Thailand infected with P. vivax and treated with atovaquone/proguanil hydrochloride 1,000 mg/400 mg daily for 3 days, parasitemia cleared in 21 (91.3%) at 7 days. Parasite relapse occurred commonly when P. vivax malaria was treated with atovaquone/proguanil alone. Relapsing malarias including P. vivax and P. ovale require additional treatment to prevent relapse.
- The efficacy of atovaquone/proguanil in treating acute uncomplicated P. falciparum malaria in children weighing ≥5 and <11 kg was examined in an open‑label, randomized trial conducted in Gabon. Patients received either atovaquone/proguanil (2 or 3 atovaquone/proguanil Pediatric Tablets once daily depending upon body weight) for 3 days (n = 100) or amodiaquine (10 mg/kg/day) for 3 days (n = 100). In this study, the atovaquone/proguanil Tablets were crushed and mixed with condensed milk just prior to administration. An adequate clinical response (elimination of parasitemia with no recurrent parasitemia during follow‑up for 28 days) was obtained in 95% (87/92) of the evaluable pediatric patients who received atovaquone/proguanil and in 53% (41/78) of those evaluable who received amodiaquine. A response of RI resistance (elimination of parasitemia but with recurrent parasitemia between 7 and 28 days after starting treatment) was noted in 3% and 40% of the patients, respectively. Two cases of RIII resistance (rising parasite count despite therapy) were reported in the patients receiving atovaquone/proguanil. There were 4 cases of RIII in the amodiaquine arm.
How Supplied
- atovaquone/proguanil Tablets, containing 250 mg atovaquone and 100 mg proguanil hydrochloride.
- Bottle of 100 tablets with child-resistant closure (NDC 0173-0675-01).
- Unit Dose Pack of 24 (NDC 0173-0675-02).
- Atovaquone/proguanil Pediatric Tablets, containing 62.5 mg atovaquone and 25 mg proguanil hydrochloride.
- Bottle of 100 tablets with child-resistant closure (NDC 0173-0676-01).
Storage
- Storage Conditions: Store at 25°C (77°F). Temperature excursions are permitted to 15° to 30°C (59° to 86°F) (see USP Controlled Room Temperature).
Images
Drug Images
{{#ask: Page Name::Atovaquone-Proguanil |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Atovaquone-Proguanil |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Patients should be instructed:
- to take MALARONE at the same time each day with food or a milky drink.
- to take a repeat dose of MALARONE if vomiting occurs within 1 hour after dosing.
- to take a dose as soon as possible if a dose is missed, then return to their normal dosing schedule. However, if a dose is skipped, the patient should not double the next dose.
- that rare serious adverse events such as hepatitis, severe skin reactions, neurological, and hematological events have been reported when MALARONE was used for the prophylaxis or treatment of malaria.
- to consult a healthcare professional regarding alternative forms of prophylaxis if prophylaxis with MALARONE is prematurely discontinued for any reason.
- that protective clothing, insect repellents, and bednets are important components of malaria prophylaxis.
- that no chemoprophylactic regimen is 100% effective; therefore, patients should seek medical attention for any febrile illness that occurs during or after return from a malaria‑endemic area and inform their healthcare professional that they may have been exposed to malaria.
- that falciparum malaria carries a higher risk of death and serious complications in pregnant women than in the general population. Pregnant women anticipating travel to malarious areas should discuss the risks and benefits of such travel with their physicians.
Precautions with Alcohol
Alcohol-Atovaquone-Proguanil interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- MALARONE®[2]
Look-Alike Drug Names
There is limited information regarding Look-Alike Drug Names.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.