Thyroid hormone
|
WikiDoc Resources for Thyroid hormone |
|
Articles |
|---|
|
Most recent articles on Thyroid hormone Most cited articles on Thyroid hormone |
|
Media |
|
Powerpoint slides on Thyroid hormone |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Thyroid hormone at Clinical Trials.gov Trial results on Thyroid hormone Clinical Trials on Thyroid hormone at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Thyroid hormone NICE Guidance on Thyroid hormone
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Thyroid hormone Discussion groups on Thyroid hormone Patient Handouts on Thyroid hormone Directions to Hospitals Treating Thyroid hormone Risk calculators and risk factors for Thyroid hormone
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Thyroid hormone |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Phone:617-632-7753
Overview
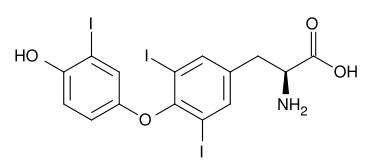
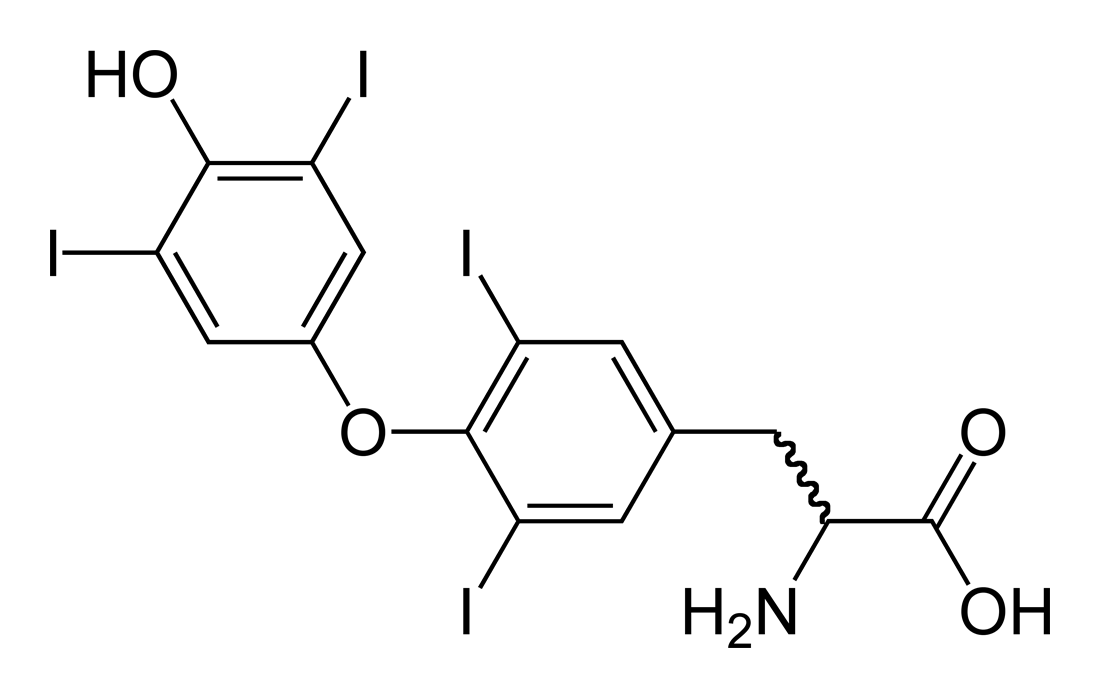
The thyroid hormones, thyroxine (T4) and triiodothyronine (T3), are tyrosine-based hormones produced by the thyroid gland. An important component in the synthesis is iodine. The major form of thyroid hormone in the blood is thyroxine (T4). The ratio of T4 to T3 released in the blood is roughly 20 to 1. Thyroxine is converted to the active T3 (three to four times more potent than T4) within cells by deiodinases (5'-iodinase). These are further processed by decarboxylation and deiodination to produce iodothyronamine (T1a) and thyronamine (T0a).
Circulation
Most of the thyroid hormone circulating in the blood is bound to transport proteins. Only a very small fraction of the circulating hormone is free (unbound) and biologically active, hence measuring concentrations of free thyroid hormones is of great diagnostic value.
When thyroid hormone is bound, it is not active, so the amount of free T3/T4 is what is important. For this reason, measuring total thyroxine in the blood can be misleading.
| Type | Percent |
| bound to thyroxine-binding globulin (TBG) | 70% |
| bound to transthyretin or "thyroxine-binding prealbumin" (TTR or TBPA) | 10-15% |
| albumin | 15-20% |
| unbound T4 (fT4) | 0.03% |
| unbound T3 (fT3) | 0.3% |
T3 and T4 cross the cell membrane, probably via amino acid importins, and function via a well-studied set of nuclear receptors in the nucleus of the cell, the thyroid hormone receptors.
T1a and T0a are positively charged and do not cross the membrane; they are believed to function via the trace amine-associated receptor TAAR1 (TAR1, TA1), a G-protein-coupled receptor located in the cell membrane.
Another critical diagnostic tool is the amount of thyroid-stimulating hormone (TSH) that is present.
Function
The thyronines act on the body to increase the basal metabolic rate, affect protein synthesis and increase the body's sensitivity to catecholamines (such as adrenaline) by permissiveness. The thyroid hormones are essential to proper development and differentiation of all cells of the human body. These hormones also regulate protein, fat, and carbohydrate metabolism, affecting how human cells use energetic compounds. Numerous physiological and pathological stimuli influence thyroid hormone synthesis.
The thyronamines function via some unknown mechanism to inhibit neuronal activity; this plays an important role in the hibernation cycles of mammals and the moulting behaviour of birds. One effect of administering the thyronamines is a severe drop in body temperature.
Related diseases
Both excess and deficiency of thyroxine can cause disorders.
- Thyrotoxicosis or hyperthyroidism (more specifically Graves Disease) is the clinical syndrome caused by an excess of circulating free thyroxine, free triiodothyronine, or both. It is a common disorder that affects approximately 2% of women and 0.2% of men.
- Hypothyroidism (an example is Hashimoto's thyroiditis) is the case where there is a deficiency of thyroxine, triiodiothyronine, or both.
- Clinical depression can sometimes be caused by hypothyroidism[1]. Some research[2] has shown that T3 is found in the junctions of synapses, and regulates the amounts and activity of serotonin, norepinephrine, and Gamma-aminobutyric acid (GABA) in the brain.
Medical use of thyroid hormones
Both T3 and T4 are used to treat thyroid hormone deficiency (hypothyroidism). They are both absorbed well by the gut, so can be given orally. Levothyroxine, the most commonly used synthetic thyroxine form, is a stereoisomer of physiological thyroxine, which is metabolised more slowly and hence usually only needs once-daily administration. Natural desiccated thyroid hormones, which are derived from pig thyroid glands, are a "natural" hypothyroid treatment containing 20% T3 and traces of T2, T1 and calcitonin.
Thyronamines have no medical usages yet, though their use has been proposed for controlled induction of hypothermia which causes the brain to enter a protective cycle, useful in preventing damage during ischemic shock.
Synthetic thyroxine was first successfully produced by Charles Robert Harington and George Barger in 1926.
Structure and production of the thyroid hormones
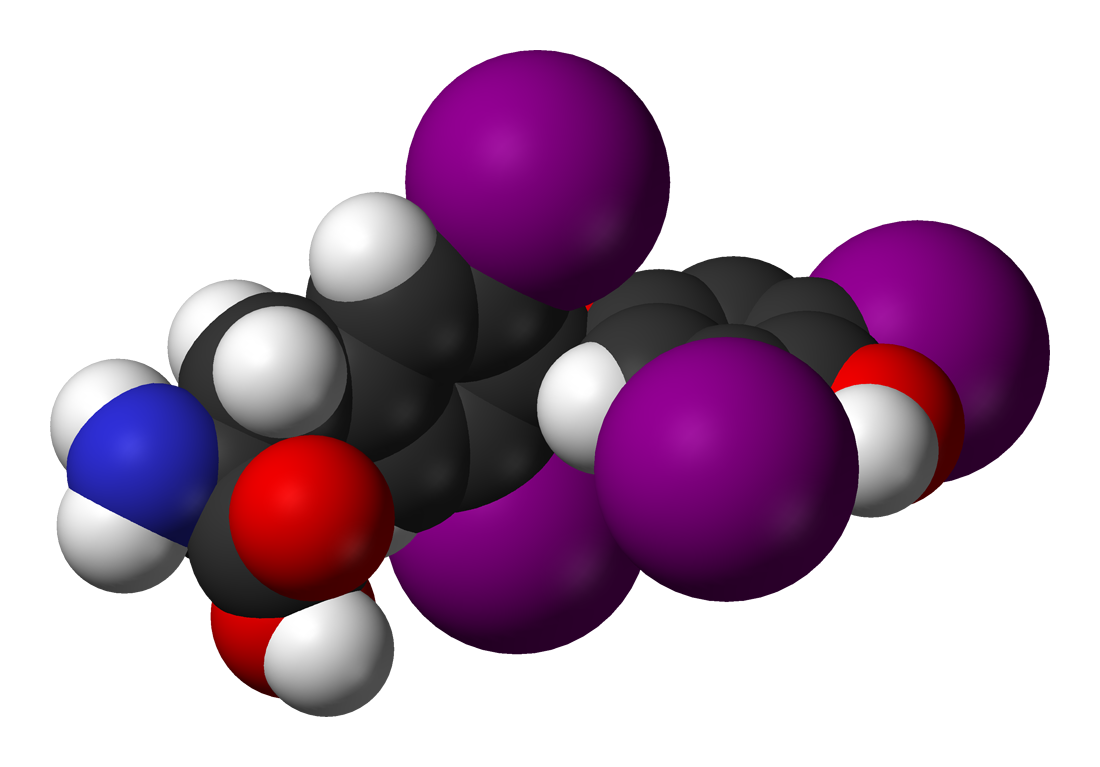
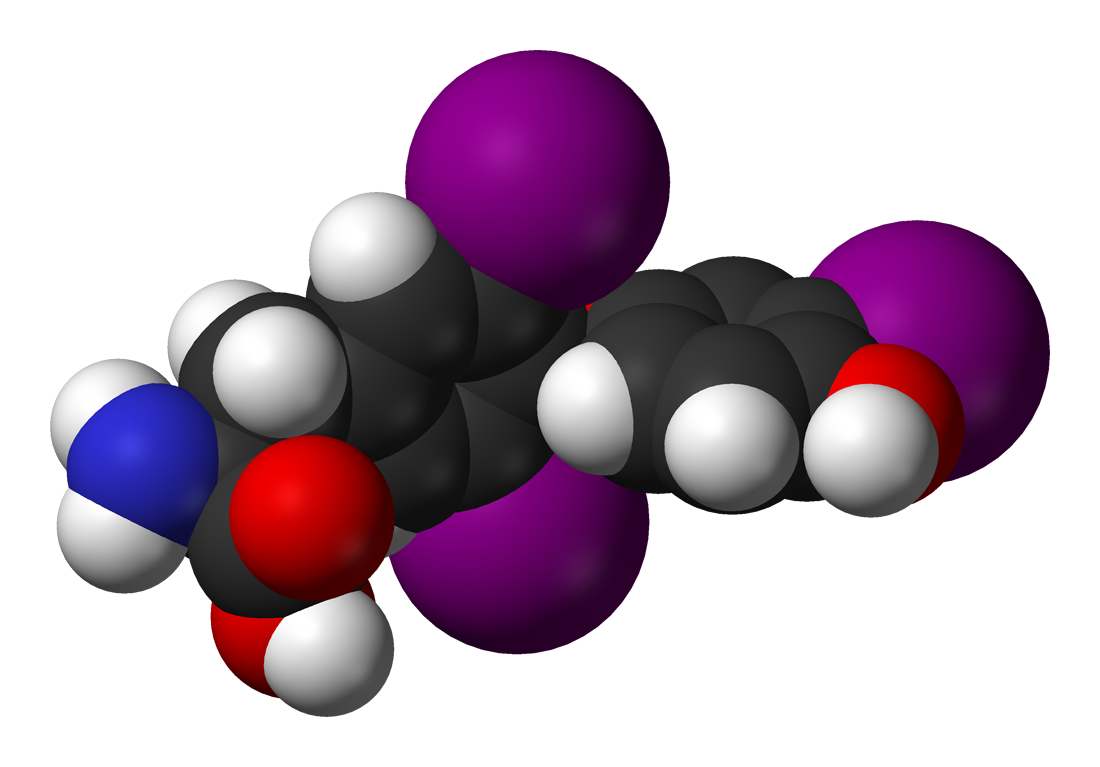
Thyroxine (3,5,3',5'-tetraiodothyronine) is produced by follicular cells of the thyroid gland. It is produced as the precursor thyroglobulin (this is not the same as TBG), which is cleaved by enzymes to produce active T4.
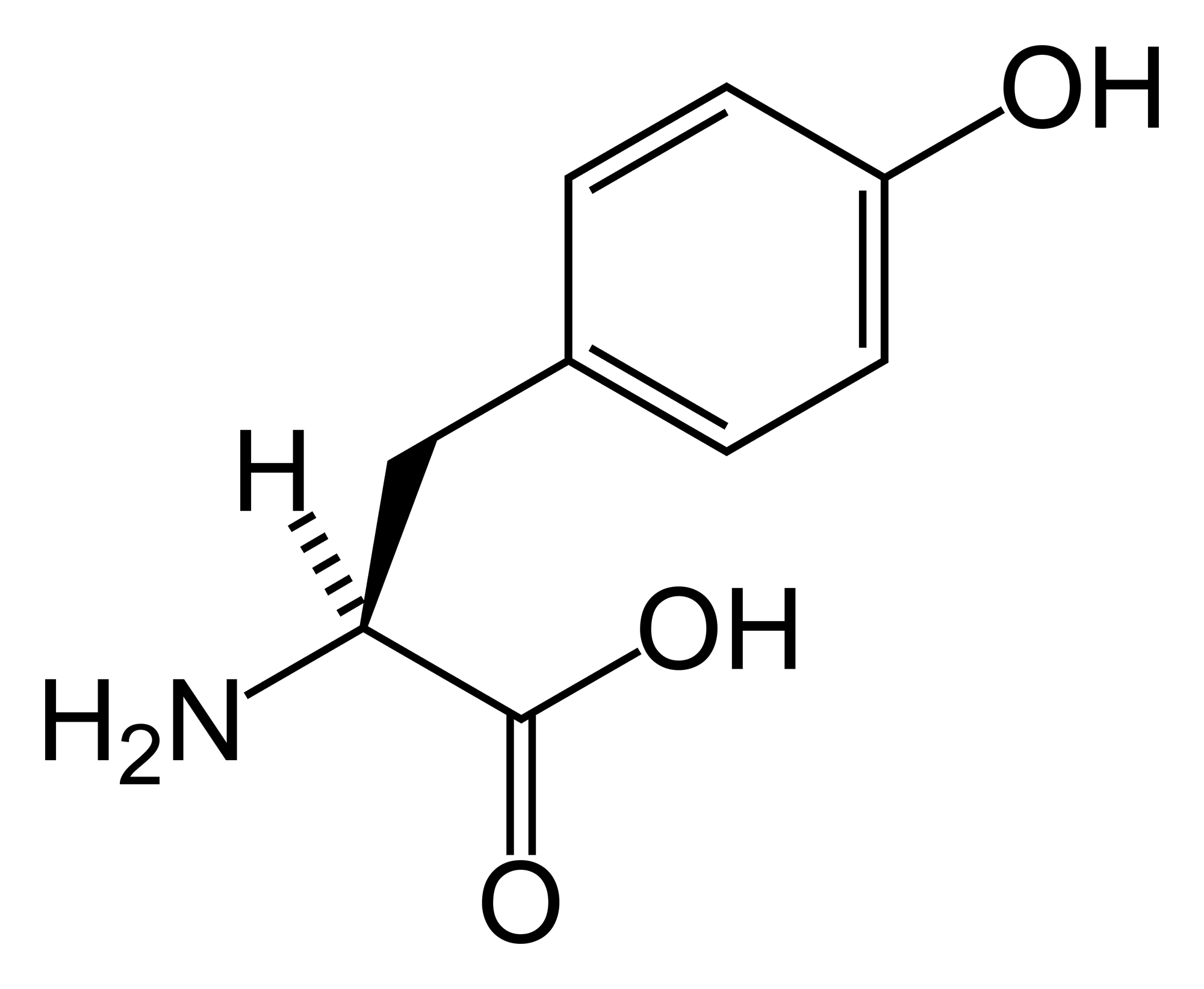
Thyroxine is produced by attaching iodine atoms to the ring structures of tyrosine molecules. Thyroxine contains four iodine atoms. Triiodothyronine is identical to T4, but it has one less iodine atom per molecule.
Iodide is actively absorbed from the bloodstream by a process called 'iodine trapping'and concentrated in the thyroid follicles. (If there is a deficiency of dietary iodine, the thyroid enlarges in an attempt to trap more iodine, resulting in goitre.) Via a reaction with the enzyme thyroperoxidase, iodine is covalently bound to tyrosine residues in the thyroglobulin molecules, forming monoiodotyrosine (MIT) and diiodotyrosine (DIT). Linking two moieties of DIT produces thyroxine. Combining one particle of MIT and one particle of DIT produces triiodothyronine.
- MIT + DIT → triiodothyronine (usually referred to as T3)
- DIT + DIT → thyroxine (referred to as T4)
Proteases digest iodinated thyroglobulin, releasing the hormones T4 and T3, the biologically active agents central to metabolic regulation. Thyroxine is supposedly a prohormone and a reservoir for the most active and main thyroid hormone T3. T4 is converted as required in the tissues by deiodinases. Deficiency of deiodinase can mimic an iodine deficiency. T3 is more active than T4 and is the final form of the hormone, though it is present in less quantity than T4.
Anti-thyroid drugs
Iodine uptake against a concentration gradient is mediated by a sodium iodine symporter. Perchlorate and thiocyanate are drugs that can compete with iodine at this point.
Effects of thyroxine
- Increases cardiac output
- Increases heart rate
- Increases ventilation rate
- Increases basal metabolic rate
- Potentiates brain development
- Thickens endometrium in females
References
See also
- Hormone
- Thyroid gland
- Thyroid-stimulating hormone
- Thyronamines, metabolites of the thyroid hormones that act at the trace amine-associated receptor TAAR1 (TAR1)
- Goitre
- Graves-Basedow disease
External links
- Template:McGrawHillAnimation
- [http://www.thyroidmanager.org/ Collection of medical articles on Thyroid disease including
the hormones]
bg:Трийодтиронин
cs:Hormony štítné žlázy
de:Schilddrüsenhormon
he:תריודוטירונין