Andexanet alfa
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Yashasvi Aryaputra[2], Anmol Pitliya, M.B.B.S. M.D.[3]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING: THROMBOEMBOLIC RISKS, ISCHEMIC RISKS, CARDIAC ARREST, AND SUDDEN DEATHS
See full prescribing information for complete Boxed Warning.
Treatment with andexanet alfa has been associated with serious and life-threatening adverse events, including:
|
Overview
Andexanet alfa is a sterile, white to off-white lyophilized powder available in single-use vials, containing 100 mg of coagulation factor Xa formulated with the inactive ingredients tromethamine (Tris), L-arginine hydrochloride, sucrose (2% w/v), mannitol (5% w/v), and polysorbate 80 (0.01% w/v) at pH 7.8 that is FDA approved for the treatment of patients treated with rivaroxaban and apixaban, when reversal of anticoagulation is needed due to life-threatening or uncontrolled bleeding. There is a Black Box Warning for this drug as shown here. Common adverse reactions include urinary tract infections and pneumonia.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Andexanet alfa is indicated:
- For patients treated with rivaroxaban and apixaban, when reversal of anticoagulation is needed due to life-threatening or uncontrolled bleeding.
- This indication is approved under accelerated approval based on the change from baseline in anti-FXa activity in healthy volunteers. An improvement in hemostasis has not been established. Continued approval for this indication may be contingent upon the results of studies to demonstrate an improvement in hemostasis in patients.
Limitation of Use
- Andexanet alfa has not been shown to be effective for, and is not indicated for, the treatment of bleeding related to any FXa inhibitors other than apixaban and rivaroxaban.
Dose
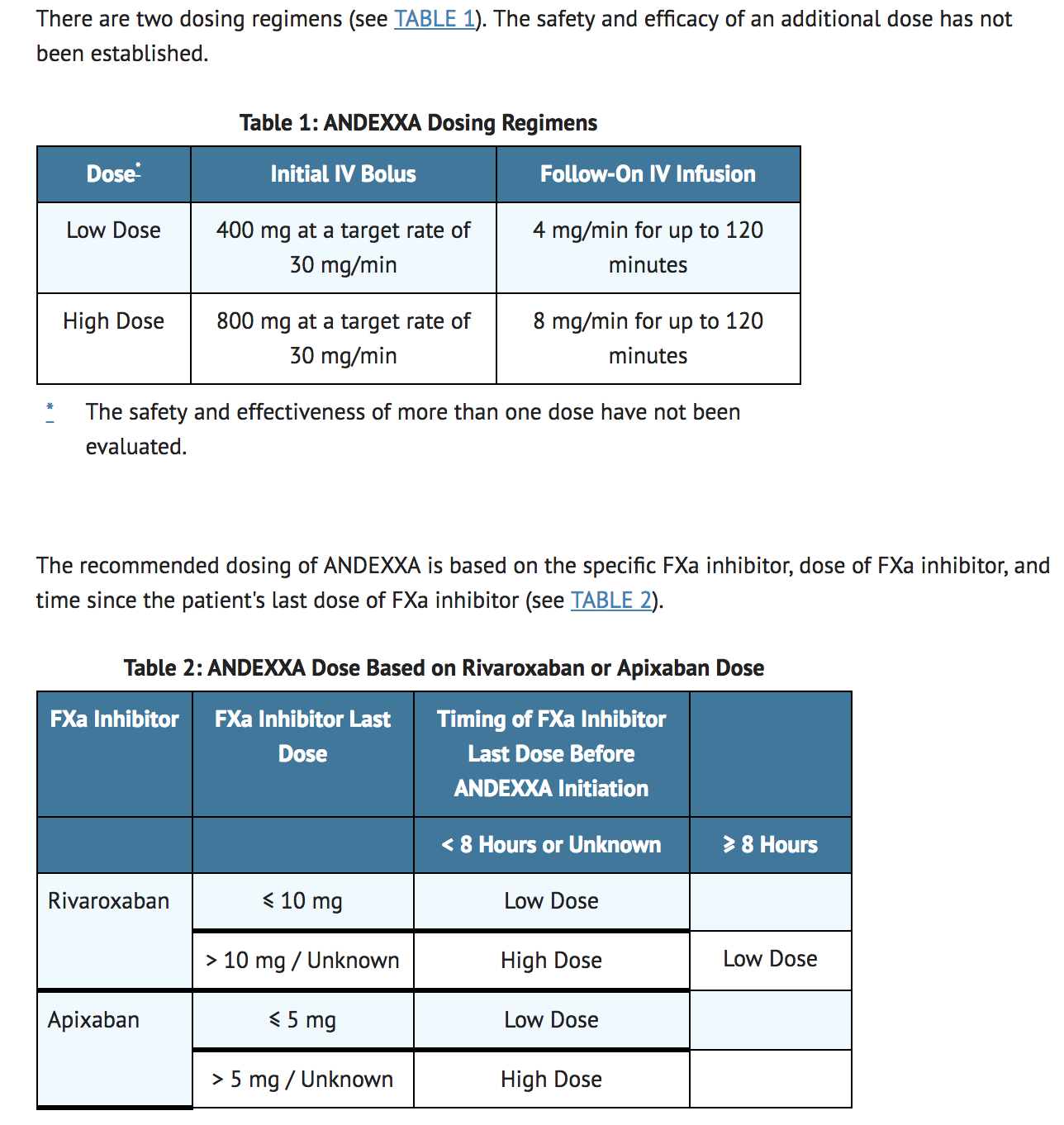
Reconstitution
- Upon reconstitution, the parenteral drug product should be inspected visually for particulate matter and discoloration prior to administration.
- The reconstituted solution contains coagulation factor Xa (recombinant), inactivated-zhzo at a concentration of 10 mg/mL.
- Reconstituted andexanet alfa in vials is stable at room temperature for up to 8 hours, or may be stored for up to 24 hours at 2°C to 8°C.
- Reconstituted andexanet alfa in IV bags is stable at room temperature for up to 8 hours, or may be stored for up to 16 hours at 2°C to 8°C.
IV Bolus Preparation
- Reconstitute each 100 mg vial of andexanet alfa (Figure A) using a 10-mL syringe and 20-gauge (or higher) needle. Slowly inject 10 mL Sterile Water for Injection (SWFI), USP, directing the solution onto the inside wall of the vial to minimize foaming (Figure A).
- To reduce the total reconstitution time needed during preparation, reconstitute all required vials in succession.
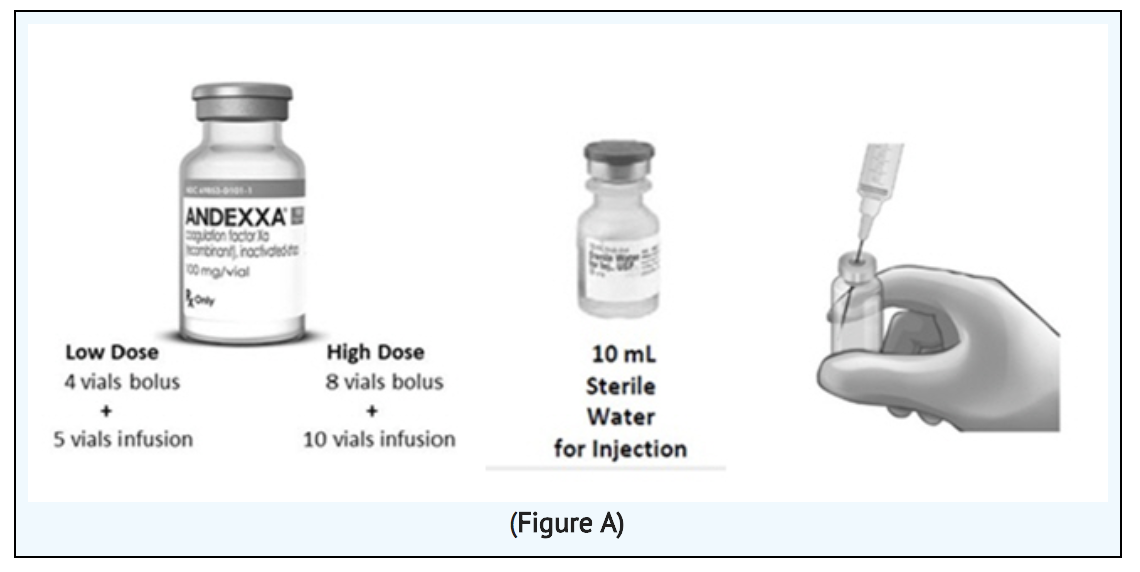
- To ensure dissolution of the cake or powder, gently swirl each vial until complete dissolution of powder occurs. Do not shake; shaking could lead to foaming (Figure B). Typical dissolution time for each vial is approximately 3 to 5 minutes. If dissolution is incomplete, discard the vial and do not use the product.
- Use 60-mL or larger syringe with a 20-gauge (or higher) needle to withdraw the reconstituted andexanet alfa solution from each of the vials until the required dosing volume is achieved. Note the total volume withdrawn into the syringe.
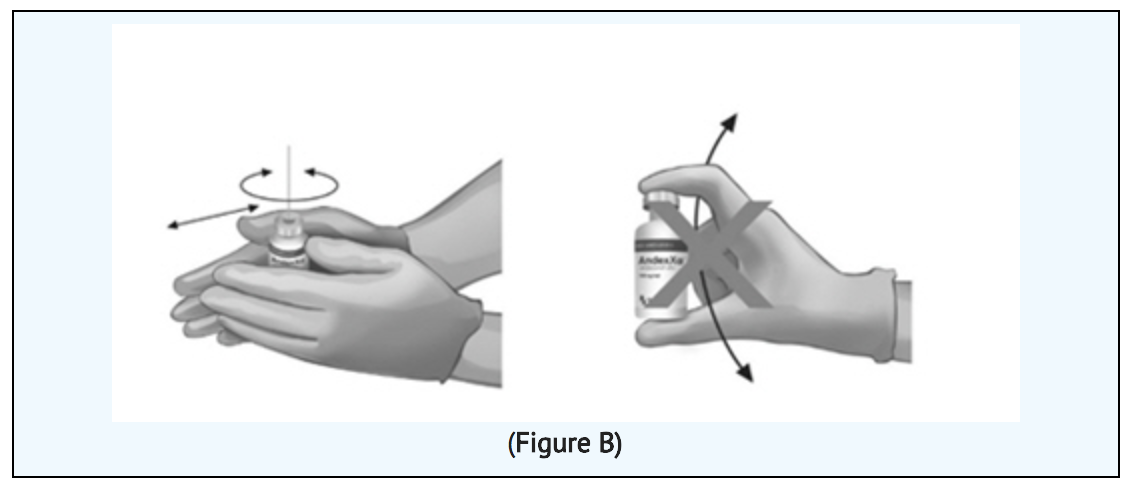
- Transfer the andexanet alfa solution from the syringe into an empty polyolefin or polyvinyl chloride IV bag with a volume of 250 mL or less (Figure C).
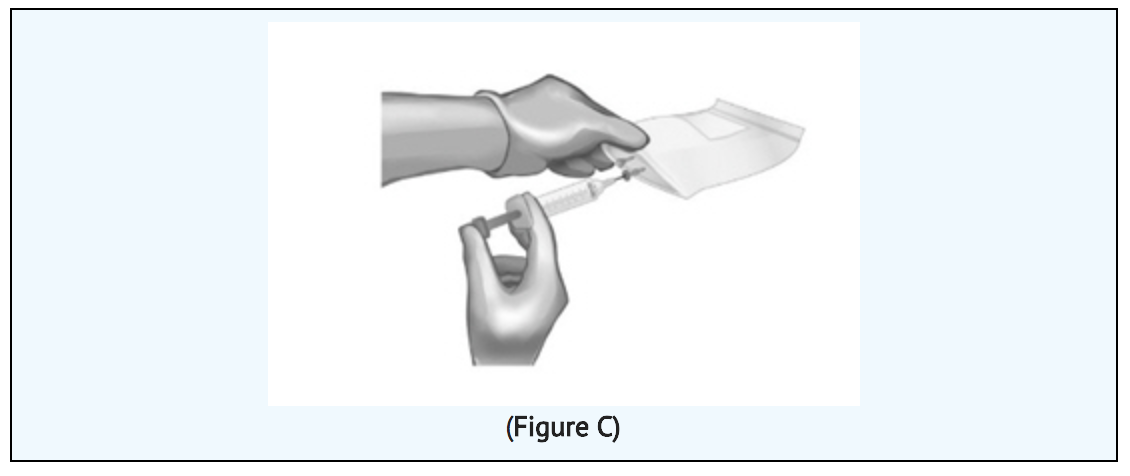
- Discard the syringe and needle.
- Discard the vials, including any unused portion.
Continuous IV Infusion Preparation
- Follow the same procedure outlined above for IV bolus preparation. Reconstitute the number of vials needed based on the dose requirements. More than one 40 to 60-mL syringe, or an equivalent 100-mL syringe, may be used for transfer of reconstituted solution to the IV bag.
- Infusion will require a 0.2 or 0.22 micron in-line polyethersulfone or equivalent low protein-binding filter.
Administration
- Administer andexanet alfa intravenously, using a 0.2 or 0.22 micron in-line polyethersulfone or equivalent low protein-binding filter.
- Start the bolus at a target rate of approximately 30 mg/minute.
- Within 2 minutes following the bolus dose, administer the continuous IV infusion for up to 120 minutes.
Restarting Antithrombotic Therapy
- Patients treated with FXa inhibitor therapy have underlying disease states that predispose them to thromboembolic events. Reversing FXa inhibitor therapy exposes patients to the thrombotic risk of their underlying disease. To reduce the risk of thrombosis, resume anticoagulant therapy as soon as medically appropriate following treatment with andexanet alfa.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding andexanet alfa Off-Label Guideline-Supported Use and Dosage (Adult) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding andexanet alfa Off-Label Non-Guideline-Supported Use and Dosage (Adult) in the drug label.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Andexanet alfa FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding andexanet alfa Off-Label Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding andexanet alfa Off-Label Non-Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Contraindications
- None
Warnings
|
WARNING: THROMBOEMBOLIC RISKS, ISCHEMIC RISKS, CARDIAC ARREST, AND SUDDEN DEATHS
See full prescribing information for complete Boxed Warning.
Treatment with andexanet alfa has been associated with serious and life-threatening adverse events, including:
|
Thromboembolic and Ischemic Risks
- Arterial and venous thromboembolic events, ischemic events, and cardiac events, including sudden death, were observed within 30 days post-andexanet alfa administration in 33 of the 185 patients (18%) evaluable for safety in the ongoing ANNEXA-4 study. The median time to first event was 6 days. Of the 86 patients who were re-anticoagulated prior to a thrombotic event, 11 (12.7%) patients experienced a thromboembolic, ischemic event, cardiac event or death.
- Monitor patients treated with andexanet alfa for signs and symptoms of arterial and venous thromboembolic events, ischemic events, and cardiac arrest. To reduce thromboembolic risk, resume anticoagulant therapy as soon as medically appropriate following treatment with andexanet alfa.
- The safety of andexanet alfa has not been evaluated in patients who experienced thromboembolic events or disseminated intravascular coagulation within two weeks prior to the life-threatening bleeding event requiring treatment with andexanet alfa. Safety of andexanet alfa also has not been evaluated in patients who received prothrombin complex concentrates, recombinant factor VIIa, or whole blood products within seven days prior to the bleeding event.
Re-elevation or Incomplete Reversal of Anti-FXa Activity
- The time course of anti-FXa activity following andexanet alfa administration was consistent among the healthy volunteer studies and the ANNEXA-4 study in bleeding patients. Compared to baseline, there was a rapid and substantial decrease in anti-FXa activity corresponding to the andexanet alfa bolus. This decrease was sustained through the end of the andexanet alfa continuous infusion. Following the infusion, there was an increase in anti-FXa activity, which peaked 4 hours after infusion in ANNEXA-4 subjects. After this peak, the anti-FXa activity decreased at a rate similar to the clearance of the FXa inhibitors.
- Thirty-eight patients who were anticoagulated with apixaban had baseline levels of anti-FXa activity >150 ng/mL. Nineteen of these 38 (50%) patients experienced a > 93% decrease from baseline anti-FXa activity after administration of andexanet alfa. Eleven patients who were anticoagulated with rivaroxaban had baseline anti-FXa activity levels > 300 ng/mL. Five of the 11 patients experienced a > 90% decrease from baseline anti-FXa activity after administration of andexanet alfa.
Adverse Reactions
Clinical Trials Experience
- The most common adverse reactions (≥ 5%) in patients receiving andexanet alfa were urinary tract infections and pneumonia.
- The most common adverse reactions (≥ 3%) in healthy volunteers treated with andexanet alfa were infusion-related reactions.
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
- In the pooled safety analysis of clinical trials of andexanet alfa, 223 healthy volunteers received FXa inhibitors followed by treatment with andexanet alfa. The frequency of adverse reactions was similar in the andexanet alfa-treated group (120/223, 54%) and the placebo-treated group (54/94, 57%). Infusion-related adverse reactions occurred in 18% (39/223) of the andexanet alfa-treated group, and was the only adverse reaction that occurred more frequently than in the placebo group. No serious or severe adverse reactions were reported.
- The ANNEXA-4 study is an ongoing multinational, prospective, open-label study using andexanet alfa in patients presenting with acute major bleeding who have recently received a FXa inhibitor. To date, safety data are available for 185 patients. Approximately half of the patients are male with median age of 78 years. Patients had received either apixaban (98/185, 53%) or rivaroxaban (72/185, 40%), as anticoagulation treatment for atrial fibrillation (143/185, 77%) or venous thromboembolism (48/185, 26%). In the majority of patients, andexanet alfa was used to reverse anticoagulant therapy following either an intracranial hemorrhage (106; 57%) or a gastrointestinal bleed (58; 31%), with the remaining 21 patients (11%) experiencing bleeding at other sites. Patients were assessed at a 30-day follow-up visit following infusion of andexanet alfa.
Deaths
- In the ongoing ANNEXA-4 study, there were 25 deaths (14%) prior to the Day 30 follow-up visit. Eight patients died within 10 days after the andexanet alfa infusion. The percentage of patients, by bleeding type, who died prior to the Day 30 follow-up visit was: 14% for intracranial bleeding, 10% for gastrointestinal bleeding, and 19% for other bleeding types.
Thromboembolic Events
- In the ongoing ANNEXA-4 study, 33/185 (17.8%) patients experienced one or more of the following events: deep venous thrombosis (11/33; 33%), ischemic stroke (9/33; 24%), acute myocardial infarction (5/33; 15%), pulmonary embolism (5/33; 15%), cardiogenic shock (3/33; 9%), sudden death (2/33; 6%), congestive heart failure (2/33; 6%), acute respiratory failure (2/33; 6%), cardiac arrest (1/33; 3%), cardiac thrombus (1/33; 3%), embolic stroke (1/33; 3%), iliac artery thrombosis (1/33; 3%), and non-sustained ventricular tachycardia (1/33; 3%). The median time to the first event in these 33 subjects was 6 days. Eleven of 33 (33%) patients were on antithrombotic therapy at the time of the event.
- No thromboembolic events were observed in 223 healthy volunteers who received FXa inhibitors and were treated with andexanet alfa.
Infusion-related Reactions'
- Infusion-related reactions occurred in 18% (39/223) of andexanet alfa-treated healthy volunteers vs. 6% (6/94) of placebo-treated subjects. These reactions were characterized by a range of symptoms including flushing, feeling hot, cough, dysgeusia, and dyspnea. Symptoms were mild to moderate in severity, and 90% (35/39) did not require treatment. One subject with a history of hives prematurely discontinued andexanet alfa after developing mild hives.
Immunogenicity
- As with all therapeutic proteins, there is the potential for immunogenicity. Using an electrochemiluminescence (ECL)-based assay, 145 andexanet alfa-treated healthy subjects were tested for antibodies to andexanet alfa as well as antibodies cross-reacting with Factor X (FX) and FXa. Low titers of anti-andexanet alfa antibodies were observed in 26/145 healthy subjects (17%); 6% (9/145) were first observed at Day 30 with 20 subjects (14%) still having titers at the last time point (Days 44 to 48). To date, the pattern of antibody response in patients in the ANNEXA-4 study has been similar to that observed in healthy volunteers with 6% (6/98) of the patients having antibodies against andexanet alfa. None of these anti-andexanet alfa antibodies were neutralizing. No antibodies cross-reacting with FX or FXa were detected in healthy subjects (0/145) or in bleeding patients (0/98) to date.
- Detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors, including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to andexanet alfa with the incidence of antibodies to other products may be misleading.
Postmarketing Experience
There is limited information regarding Andexanet alfa Postmarketing Experience in the drug label.
Drug Interactions
There is limited information regarding Andexanet alfa Drug Interactions in the drug label.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): There are no adequate and well-controlled studies of andexanet alfa in pregnant women to inform patients of associated risks. Animal reproductive and development studies have not been conducted with andexanet alfa.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Andexanet alfa in women who are pregnant.
Labor and Delivery
- The safety and effectiveness of andexanet alfa during labor and delivery have not been evaluated.
Nursing Mothers
- There is no information regarding the presence of andexanet alfa in human milk, the effects on the breastfed child, or the effects on milk production.
- The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for andexanet alfa and any potential adverse effects on the breastfed child from andexanet alfa or from the underlying maternal condition.
Pediatric Use
- The safety and efficacy of andexanet alfa in the pediatric population have not been studied.
Geriatic Use
- Of the 185 subjects in the ANNEXA-4 study of andexanet alfa, 161 were 65 years of age or older and 113 were 75 years of age or older. No overall differences in safety or efficacy were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
- The pharmacokinetics of andexanet alfa in older (≥ 65 years, n=10) patients were not different compared to younger (18-45 years, n=10) patients.
Gender
There is no FDA guidance on the use of Andexanet alfa with respect to specific gender populations.
Race
There is no FDA guidance on the use of Andexanet alfa with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Andexanet alfa in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Andexanet alfa in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Andexanet alfa in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Andexanet alfa in patients who are immunocompromised.
Administration and Monitoring
Administration
- Administer andexanet alfa intravenously, using a 0.2 or 0.22 micron in-line polyethersulfone or equivalent low protein-binding filter.
- Start the bolus at a target rate of approximately 30 mg/minute.
- Within 2 minutes following the bolus dose, administer the continuous IV infusion for up to 120 minutes.
Monitoring
- Normalization of coagulation parameters indicates efficacy
- Monitor for a reduction in anti-factor Xa activity
- Signs and symptoms of arterial and venous thromboembolic events, ischemic events, and cardiac arrest
IV Compatibility
There is limited information regarding the compatibility of Andexanet alfa and IV administrations.
Overdosage
There is limited information regarding Andexanet alfa overdosage. If you suspect drug poisoning or overdose, please contact the National Poison Help hotline (1-800-222-1222) immediately.
Pharmacology
Andexanet alfa
| |
| Systematic (IUPAC) name | |
| ? | |
| Identifiers | |
| CAS number | |
| ATC code | V03 |
| PubChem | ? |
| Chemical data | |
| Formula | ? |
| Mol. mass | ? |
| Synonyms | PRT064445, PRT4445 |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status |
Approved |
| Routes | Intravenous injection |
Mechanism of Action
- Coagulation factor Xa (recombinant), inactivated-zhzo exerts its procoagulant effect by binding and sequestering the FXa inhibitors, rivaroxaban and apixaban. Another observed procoagulant effect of the andexanet alfa protein is its ability to bind and inhibit the activity of Tissue Factor Pathway Inhibitor (TFPI). Inhibition of TFPI activity can increase tissue factor-initiated thrombin generation.
Structure
There is limited information regarding Andexanet alfa Structure in the drug label.
Pharmacodynamics
- The effects of andexanet alfa can be measured using assays for its anti-FXa activity, free fraction of FXa inhibitor and thrombin generation. In addition to its ability to sequester the FXa inhibitors, rivaroxaban and apixaban, andexanet alfa has been shown to inhibit the Tissue Factor Pathway Inhibitor (TFPI) activity.
- The dose and dosing regimen of andexanet alfa that are required to reverse anti-FXa activity and to restore thrombin generation were determined in dose-ranging studies on healthy volunteers. Dosing of andexanet alfa, as a bolus followed by a 2-hour continuous infusion, resulted in a rapid decrease in anti-FXa activity (within two minutes after the completion of the bolus administration) followed by reduced anti-FXa activity that was maintained throughout the duration of the continuous infusion. The anti-FXa activity returned to the placebo levels approximately 2 hours after completion of a bolus or continuous infusion. Whereas, TFPI activity in plasma was sustained for at least 22 hours following andexanet alfa administration.
- Elevation of Tissue Factor (TF)-initiated thrombin generation above the baseline range (prior to anticoagulation) occurred within two minutes following a bolus administration of andexanet alfa and was maintained throughout the duration of the continuous infusion. The TF-initiated thrombin generation was elevated above placebo for up to 22 hours. The sustained elevation of thrombin generation over the baseline range, and sustained elevation over placebo were not observed in a contact-activated thrombin generation assay (an assay that is not affected by TF-TFPI interaction).
Pharmacokinetics
Distribution
- The volume of distribution (Vd) for andexanet alfa is approximately equivalent to the blood volume of 5 L.
Elimination
- Clearance for andexanet alfa is approximately 4.3 L/hr. The elimination half-life ranges from 5 to 7 hours.
Drug-Drug Interaction
- The pharmacokinetics of andexanet alfa was not affected by apixaban (5 mg orally BID for 6 days) or rivaroxaban (20 mg orally once daily for 6 days).
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- No animal studies were performed to evaluate the effects of andexanet alfa on carcinogenesis, mutagenesis, or impairment of fertility.
Clinical Studies
- The safety and efficacy of andexanet alfa were evaluated in two prospective, randomized, placebo-controlled studies, conducted in healthy volunteers. Both studies examined the percent change in anti-FXa activity, from baseline to nadir, for the low-dose and high-dose regimens of bolus followed by continuous infusion. Nadir is defined as the smallest value measured within 5 minutes after the end of the continuous infusion.
Study 1(NCT02207725) – apixaban reversal
- In Study 1, healthy subjects (median age: 57 years; range: 50 to 73 years) received apixaban 5 mg twice daily for 3.5 days to achieve steady-state. At 3 hours after the last apixaban dose (~ Cmax), andexanet alfa or placebo was administered. Eight subjects received placebo and 24 received andexanet alfa, administered as a 400 mg intravenous (IV) bolus followed by a 4 mg per minute continuous infusion for 120 minutes (total 480 mg).
Study 2 (NCT02220725) – rivaroxaban reversal
- In Study 2, healthy subjects (median age: 57 years, range: 50 to 68 years) received rivaroxaban 20 mg once per day for 4 days to achieve steady-state. At 4 hours after the last rivaroxaban dose (~ Cmax), andexanet alfa or placebo was administered. Thirteen subjects received placebo and 26 received andexanet alfa, administered as an 800 mg IV bolus followed by an 8 mg per minute continuous infusion for 120 minutes (total 960 mg).
Reduction in Anti-FXa Activity
- The percent change from baseline in anti-FXa activity at its nadir was statistically significant (p < 0.0001) in favor of the andexanet alfa groups compared to placebo in both Studies 1 and 2. The results of Study 1 and Study 2 are provided in Table 3 (see below).
- The time courses of anti-FXa activity before and after andexanet alfa administration are shown in Figure 1.
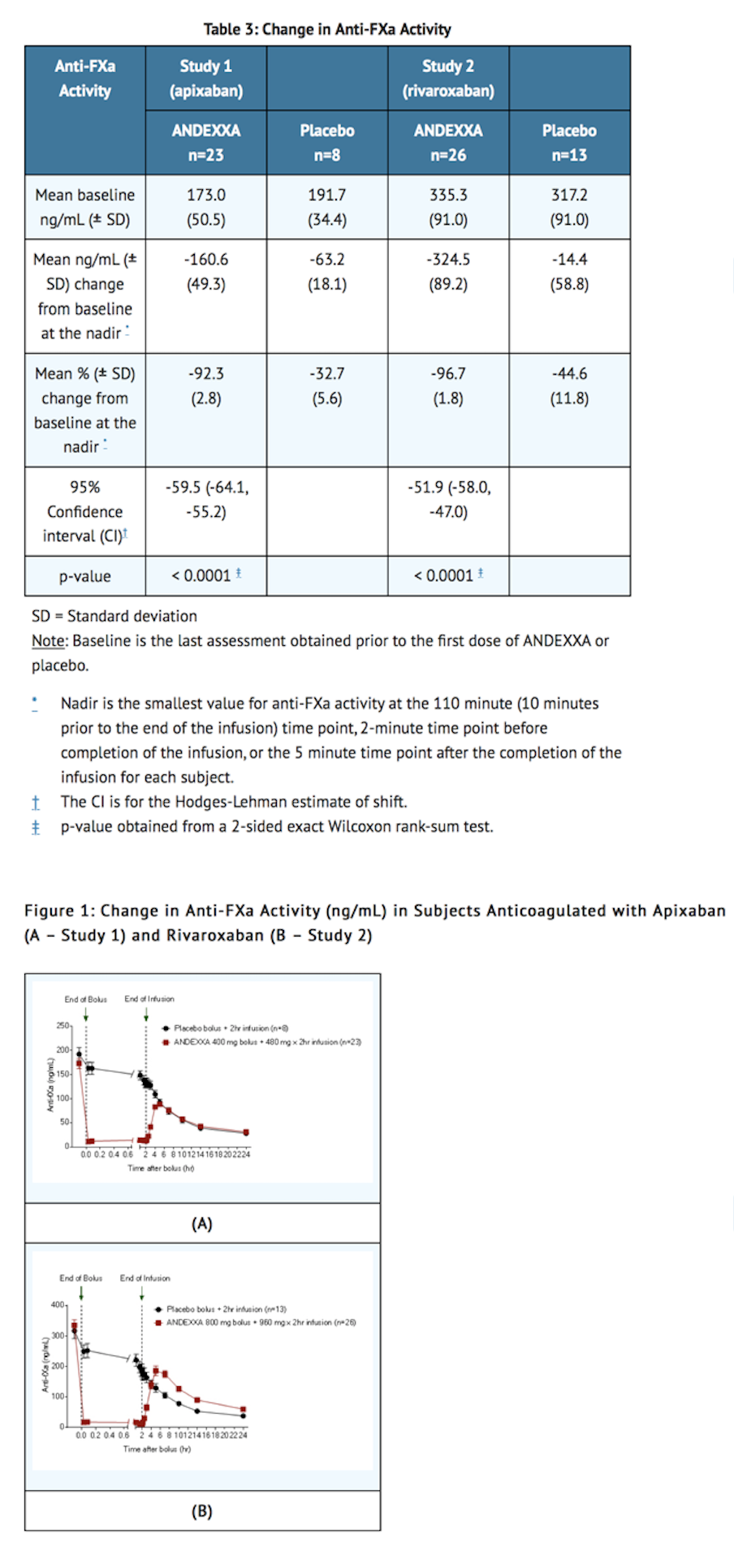
- Anti-FXa activity was measured prior to and after andexanet alfa or placebo administration.
- Dashed lines indicate the end of the bolus or infusion. A break in the x-axis is added to better visualize the immediate, short-term dynamics of anti-FXa activity following andexanet alfa treatment. The points on the graph represent the mean anti-FXa activity level; error bars illustrate standard error. There was a statistically significant difference (p < 0.05) in the percent change of anti-FXa activity normalized to pre-bolus between andexanet alfa and placebo until 2 hours after administration of infusion.
- A. Apixaban – with andexanet alfa 400 mg IV bolus plus 4 mg/min infusion for 120 minutes.
- B. Rivaroxaban – with andexanet alfa 800 mg IV bolus plus 8 mg/min infusion for 120 minutes.
ANNEXA-4 (NCT02329327)
- In an ongoing multinational, prospective, single-arm, open-label study, andexanet alfa was administered to patients taking FXa inhibitors who presented with acute major bleeding.
- Interim results of the study include data for 185 patients. Of the 185 patients, 129 were considered efficacy-evaluable, defined as patients who: 1) were dosed with andexanet alfa; 2) had a baseline anti-FXa activity above 75 ng/mL; and 3) were adjudicated as meeting eligibility criteria for acute major bleeding.
- For anti-FXa activity, the median decrease from baseline to nadir was -93% for apixaban and -90% for rivaroxaban. andexanet alfa has not been shown to be effective for bleeding related to any FXa inhibitors other than apixaban and rivaroxaban.
How Supplied
- Andexanet alfa is supplied in cartons of 4 single-use vials each containing 100 mg of andexanet alfa as a white to off-white lyophilized cake or powder.
Storage
- Unopened vials should be stored refrigerated at 2°C to 8°C (36°F to 46°F). DO NOT FREEZE.
Images
Drug Images
{{#ask: Page Name::Andexanet alfa |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Andexanet alfa |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Inform patients that reversing FXa inhibitor therapy increases the risk of thromboembolic events. Arterial and venous thromboembolic events, ischemic events, cardiac events, and sudden death were observed within 30 days following andexanet alfa administration.
Precautions with Alcohol
Alcohol-Andexanet alfa interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
- Andexxa
Look-Alike Drug Names
There is limited information regarding Andexanet alfa Look-Alike Drug Names in the drug label.
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.