Adrenal atrophy pathophysiology
|
Adrenal atrophy Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Adrenal atrophy pathophysiology On the Web |
|
American Roentgen Ray Society Images of Adrenal atrophy pathophysiology |
|
Risk calculators and risk factors for Adrenal atrophy pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Maryam Hadipour, M.D.[2]
Overview
The adrenal glands produce hormones that help regulate your metabolism, immune system, blood pressure, response to stress and other essential functions. Adrenal atrophy may be caused by a loss of ACTH and trophic support of the adrenal cortex or direct damage to the tissue due to exogenous corticosteroid overuse or an endocrine disease, affecting the glands.
Pathophysiology
Physiology
The normal physiology of adrenal atrophy can be understood as follows:
Adrenal glands produce hormones that help regulate your metabolism, immune system, blood pressure, response to stress and other essential functions. The glands are composed of two parts:
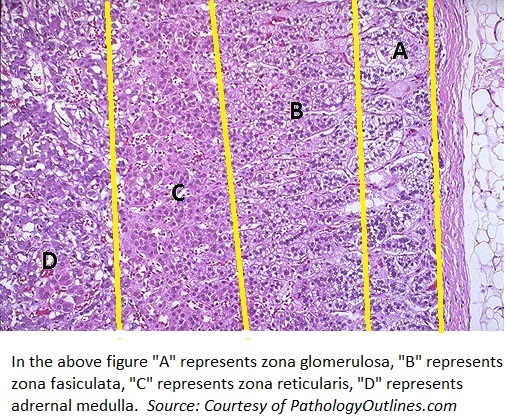
- The adrenal cortex is the outer region and also the largest part of an adrenal gland. It is divided into three separate zones: zona glomerulosa, zona fasciculata and zona reticularis. Each zone is responsible for producing specific hormones.
- The adrenal medulla is located inside the adrenal cortex in the center of an adrenal gland. It produces “stress hormones,” including epinephrine.

Pathogenesis
The exact pathogenesis of adrenal atrophy is not fully understood. However, it is thought that adrenal atrophy is caused by direct insult or the lack of stimulation of the gland. As a result, the disease can be categorized as primary or secondary.
- Primary Adrenal Atrophy: The primary atrophy is due to direct insult to the adrenal tissue due to:
- Infections (TB, CMV, histoplasmosis, paracoccidioidomycosis)
- Vascular impairments (hemorrhage from sepsis, adrenal vein thrombosis, HIT)
- Deposition disease (hemochromatosis, amyloidosis, sarcoidosis)
- Drugs (azole anti-fungals, etomidate (even one dose), rifampin, anticonvulsants)
- Cytotoxic agents such as mitotane.
- Secondary Adrenal Atrophy
The secondary atrophy is mainly due to the loss of ACTH and trophic support of the adrenal cortex, and this may result in deficits in functional capability of the cortex to produce glucocorticoids. This situation occurs in patients who are on prolonged glucocorticoid therapy, which leads to prolonged inhibition of endogenous pituitary ACTH secretion. Removal of the therapy often results in adrenocortical incompetence. Adrenal atrophy may caused by inhibition of pituitary ACTH or hypothalamic function. Compounds such as valproic acid, bromocriptine, cyproheptadine, ketanserin, ritanserin, somatostatin analogs, glucocorticoids, 4′-thio-beta-d-arabinofuranosylcytosine, and hexachlorobenzene have been noted previously to impair hypothalamo-pituitary function through deficits in ACTH or CRH in various species.
Genetics
The development of adrenal atrophy is the result of multiple genetic and environmental factors, as discussed above. However, the congenital adrenal hyperplasia, a form of adrenal hypotrophy is known as a result of the mutation on the following genes:
- An X-linked gene, NROB1, encoding DAX-1 protein
- The steroidogenic factor 1 (SF-1) gene, encoded on the 9q33 loci
The autosomal recessive ACTH resistance syndromes such as triple-A syndrome and familial glucocorticoid deficiency, are among other genetics disorders yielding to adrenal atrophy.[1][2][3]
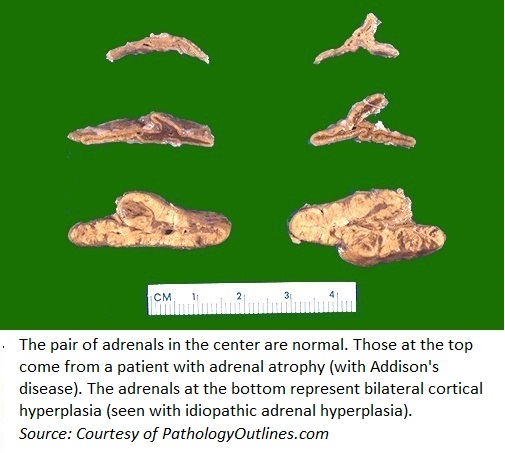
Gross pathology
On gross pathology we expect shrunken adrenal gland.
Microscopic pathology
On microscopic histopathological analysis

References
- ↑ Saleem F, Baradhi KM. PMID 31747186. Missing or empty
|title=(help) - ↑ Colagiovanni DB, Drolet DW, Dihel L, Meyer DJ, Hart K, Wolf J (2006). "Safety assessment of 4'-thio-beta-D-arabinofuranosylcytosine in the beagle dog suggests a drug-induced centrally mediated effect on the hypothalamic-pituitary-adrenal axis". Int J Toxicol. 25 (2): 119–26. doi:10.1080/10915810600605898. PMID 16597550.
- ↑ McQueen, Charlene (2010). Comprehensive toxicology. Oxford: Elsevier. ISBN 978-0080468686.